The Centers for Medicare and Medicaid Services (CMS) has published the proposed changes for the Calendar Year (CY) 2019 Physician Fee Schedule (PFS).1 Probably the most controversial of these proposed changes is the Patients Over Paperwork initiative, which streamlines documentation requirements and reimbursement for Evaluation and Management (E/M) services in the office and outpatient setting, affecting Current Procedural Terminology (CPT) codes 99201 through 99215.
CMS has announced that it plans to eliminate differential payments for most E/M codes on January 1, 2019. For the E/M codes only, Medicare will pay one rate for all new patient visits at levels 2 through 5 E/M code range and a different single rate for all established patient visits at levels 2 through 5 E/M code range.
The primary goal is to reduce administrative burden so clinicians can spend more time on patient care and less time on documentation and determining what level of service to bill for the visit. Clinicians billing these office visit CPT codes to Medicare, Medicare Advantage plans, and Medicare Railroad in 2019 will have the option to document by continuing to use the 1995 and 1997 guidelines, by Medical Decision Making (MDM), or by total time.
The proposed minimum documentation requirement to bill an E/M service based on MDM can be compared to current level 2 visit guidelines where a straightforward MDM is measured by minimal problems, minimal data reviewed, and minimal risk. CMS has also proposed that the history and exam for established patients need only be updated as to what has changed since the last visit, rather than redocumenting the same information in order to count “points” toward a specific level for each component.
This also means that clinicians can indicate in the medical record that they have reviewed the history of present illness entered by ancillary staff, rather than having to redocument the same information.
The other proposed alternative for determining the level of service is to document based on time. Currently, you can only count time if more than 50% of the face-to-face time is spent counseling and/or on care coordination for the patient. The proposal is that the clinician should document the medical necessity of the visit and show the total amount of time spent by the billing clinician face-to-face with the patient. The typical times in current CPT guidelines for each level of service would still apply.
CMS is also proposing new prolonged care add-on code GPRO1, “Prolonged evaluation and management or psychotherapy service(s) beyond the typical service time of the primary procedure in the office or other outpatient setting requiring direct patient contact beyond the usual service; 30 minutes.” The minimal time spent and documented would need only to meet the threshold of 16 minutes in order to bill for it instead of the 31 minutes required in order to bill prolonged service CPT codes 99354 (first hour) and 99355 (each additional 30 minutes).
Also proposed are add-on G-codes to help make up costs incurred by those specialties who treat patients with more complex problems. Code GCG0X, “Visit complexity inherent to evaluation and management associated with endocrinology, rheumatology, hematology/oncology, urology, neurology, obstetrics/gynecology, allergy/immunology, otolaryngology, or interventional pain management-centered care” and GPC1X, “Visit complexity inherent to evaluation and management associated with primary medical care services that serve as the continuing focal point for all needed health care services.” The codes are intended to be used with current E/M codes 99201 through 99215. CMS believes that code GPC1X will be used predominantly by family practice or pediatrics.
Unfortunately, there were no proposed auditing guidelines to determine how much documentation would be needed in order to base the E/M level on MDM or even time, making the auditor’s job very difficult beginning in 2019. During a CMS panel discussion on E/M Coding Reform,2 Dr. Kate Goodrich, CMS chief medical officer and director of the Center for Clinical Standards and Quality (CCSQ), stated that when adopting the proposed documentation guidelines, it will be imperative to have a clear, written policy in place for what is required when updating medical records.
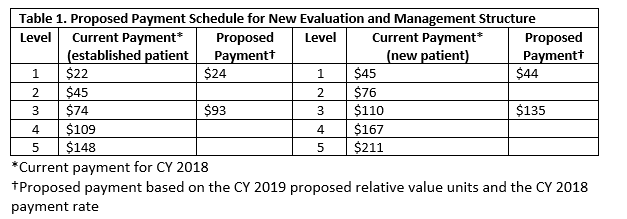
Since CMS is reducing the burden of documentation, you can probably guess that they are reducing the reimbursement as well. The proposal is to streamline payment for E/M codes that fall in the visit level 2 through 5 range, or CPT codes 99202 through 99205 and 99212 through 99215. Table 1 shows the proposed payment schedule for the new E/M structure.
During the question-and-answer portion of the August 22, 2018 listening session on the Physician Fee Schedule Proposed Rule: Understanding 3 Key Topics, hosted by the CMS Medicare Learning Network (MLN) events team, CMS confirmed that the 15% reduction rate for reimbursement for services provided by nonphysician practitioners will still apply with this new payment rule.
CMS has also proposed assigning Multiple Procedure Status 2 to codes 99201 through 99215, which means that when these codes are billed with other procedures, the most expensive code will be reimbursed at 100% and the least expensive procedure on the same visit will be reduced by 50%. This includes situations where modifier -25, “Significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of the procedure or other service” is appended to the E/M code.
Another, additional proposed change that will impact urgent care providers is that ancillary staff will be allowed to obtain and enter the History of Present Illness (HPI) as long as the record clearly indicates that the HPI has been reviewed by the provider. Currently, CMS has determined that the provider must personally obtain the HPI directly from the patient.
CMS states the reason for the Patients Over Paperwork initiative and E/M reform is that across America, the number-one complaint among clinicians was that current documentation requirements were extremely cumbersome and took away from actual patient care. They estimate a savings of 51 hours per year, per clinician if the proposed documentation requirements are implemented.
Keep in mind that these proposed changes are only for claims billed to Medicare, Medicare Advantage plans, and Medicare Railroad. CMS states that private payors were not consulted on the proposed changes, but the expectation is that they will eventually follow suit. CMS plans to continue to solicit comment on how documentation guidelines can be improved in subsequent years.
References
- Centers for Medicare & Medicaid Services Physician Fee Schedule. Details for title: CMS-1693-P. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Federal-Regulation-Notices-Items/CMS-1693-P.html. Accessed September 29, 2018.
- Centers for Medicare & Medicaid Services. CMS Office E/M Proposal. July 18, 2018. Available at: https://www.youtube.com/watch?v=W2QBTQNxfSY. Accessed September 28, 2018.