Published on
Urgent message: Most burn injuries can be handled in an outpatient setting—if they are classified accurately, treated appropriately, and referred to a regional burn center when indicated.
TRACEY QUAIL DAVIDOFF, MD
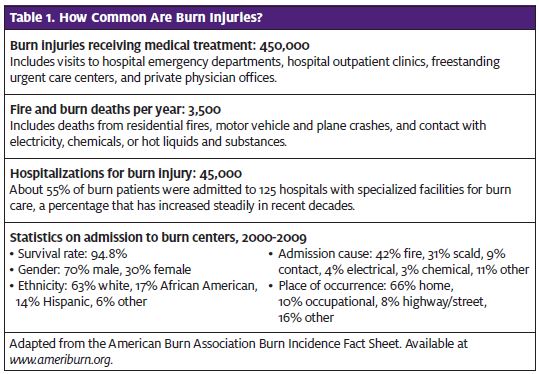
A “burn” is defined as a traumatic, thermal injury to the skin and deeper structures. Some or all of the cells of the skin can be destroyed not only by heat but also by cold, chemicals, electricity, or radiation. Burns are the third-leading cause of accidental death in the United States, and more than 1 million burn injuries are incurred in the US each year (Table 1). Burns are most common in males 18-35 years of age. Recent advances in burn care have dramatically decreased mortality to fewer than 10% of patients admitted to burn units. Mortality is twofold greater in women.
The most common type of burn in children is from a scald injury, caused, for example, by bath water that is too hot or boiling liquid from a pot on a stove.
In adults, the most common cause of burns is from direct flame or contact with a hot solid object such as a stove or oven. Hot liquids and steam also account for a fair amount of burns in adults.
Types of Burns
Four types of burns are commonly seen in the urgent care center: thermal, chemical, electrical, and radiation.
Thermal burns
Thermal burns occur from heat, either as a direct flame, contact with a solid object, steam, or hot liquids such as water or oils. The depth of injury is related to the con- tact temperature, duration of contact, and the thickness of the skin. Treatment and prognosis are related to the depth of the burn.
Chemical burns
Injury from chemicals is caused by a wide range of caus- tic reactions, including alteration of pH (eg, from acid or alkali burns), disruption of cellular membranes, and di- rect toxic effects on the metabolic processes of cells. Some examples include wet cement, hydrofluoric acid in tire cleaner, gasoline, phenols, and hydrocarbons.
The nature of the agent, as well as the length of con- tact, contribute to injury severity. This information is essential to the proper evaluation and care of chemical burns. For example, contact with acid generally produces tissue coagulation, whereas alkaline burns generate colliquation necrosis.
Systemic absorption of the burn-causing chemical is also a concern in chemical exposures. As a rule, for most chemical burns, exposure and reaction should be limited by dilution. This is accomplished by continuous irrigation of the burn with tap water or saline.
Most chemical exposures occur in the workplace or are household-related. Typically, the packaging of the chemical is brought in with the patient. If information regarding the chemical is not available, quickly searching the Internet or contacting your local poison control center may be helpful in determining the proper course of action.
Once the chemical has been eradicated, the resulting burn is treated in the same fashion as a thermal burn.
Electrical burns
Electrical energy is trans- formed into thermal energy as the current passes through human tissue. This causes cell damage and death. The magnitude of the injury depends on the pathway of current, resistance to current, and the strength and duration of current flow.
After an electric shock, patients may have electrical “entrance” and “exit” wounds. These usually occur on the hands, feet, or skull, or on oral mucous membranes, especially in children.
Electrical burns are usually painless white, gray, or yellow depressions in the skin. They can be deceiving, however, as a small wound may represent serious under- lying injury to subcutaneous structures. Compartment syndromes may occur.
Patients with serious electrical burns are at risk for rhabdomyolysis, renal failure, and cardiac conduction abnormalities. For this reason, evaluation in the hospital for any patient with an electric shock injury is warranted.
Radiation burns
The most common form of radiation burn is exposure to ultraviolet light, or sunburn. Higher amounts of radiation can cause deep internal burns; ultimately, alteration of DNA can cause cancer. Sunburn is generally treated as a first-degree, superficial, thermal burn. More serious radiation burns are beyond the scope of this article.
Evaluation
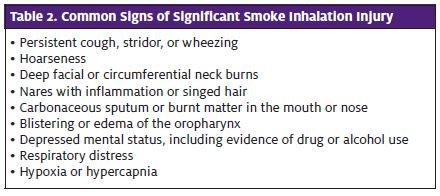
The initial approach to any burn patient should start with the ABCs. Concerns about burns to the upper airway, smoke inhalation (Table 2), and poisoning from toxic gases from burning plastics such as cyanide should always be considered. Hot and burned clothing should be reface but rarely involve the airway, unlike severe burns from prolonged heat exposure associated with smoke inhalation.
Fluid resuscitation should also be instituted as soon as possible with any moderate burns, as fluid losses and shifts may be massive. Although usually not a concern in most urgent care centers, rural areas or areas that may have a long transport time to the hospital may see patients who require fluid resuscitation in the urgent care center. Crystalloid, such as normal saline or lactated ringers, is preferred. Calculation of amounts of fluid is beyond the scope of this article but can be found in most emergency medicine textbooks (see Resources on page 20).
Burns are often associated with other injuries, such as are seen in motor vehicle crashes, blast injuries, falls from heights, and assaults. Clinicians should maintain a high index of suspicion to rule out associated injuries.
Major traumas, such as long-bone fractures and injuries of abuse or neglect, need to be considered in the evaluation of the burn patient.
Burn Classification and Treatment
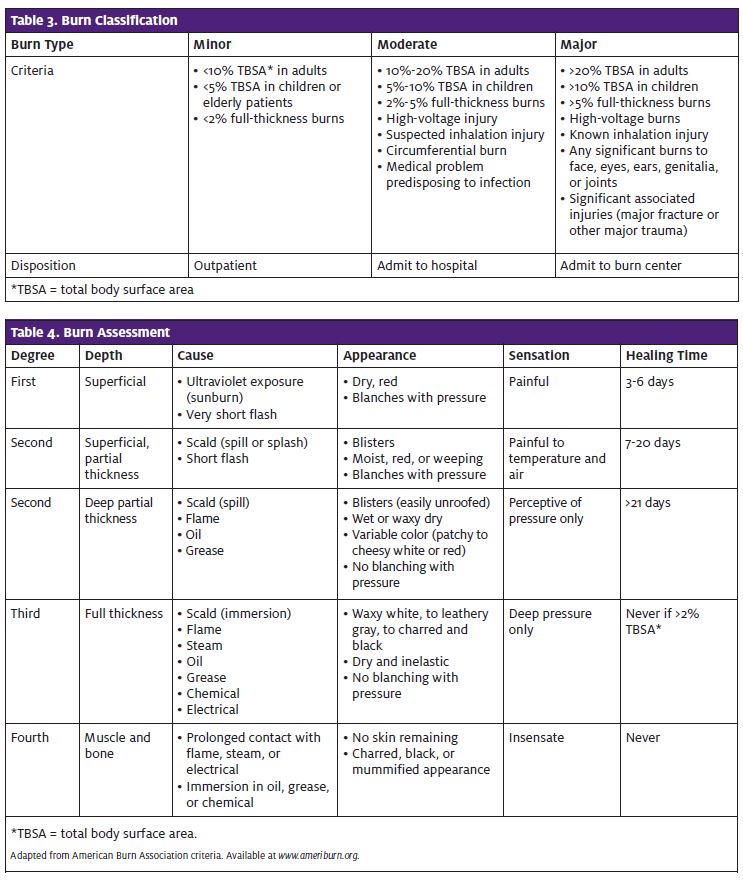
The purpose of classifying burns is to determine the best form of treatment and the prognosis, as well as whether evaluation and/or transfer to a burn center is warranted. Due to variable skin thicknesses and variation in exposures, burns may have multiple areas of varying depths, which may make classification difficult (Tables 3 and 4).
Furthermore, it may be several days or even weeks before the ex- tent of injury has fully developed. Thin skin on the forearms, me- dial thighs, perineum, and ears may sustain deeper injuries than initially predicted. Also, children under 5 and adults over 50 years of age may have thinner skin and therefore more serious injuries than expected.
Traditionally, burns were classified into three degrees, but a newer, more widely accepted classification system based on depth of injury is now used to determine prognosis and disposition of the burn patient.
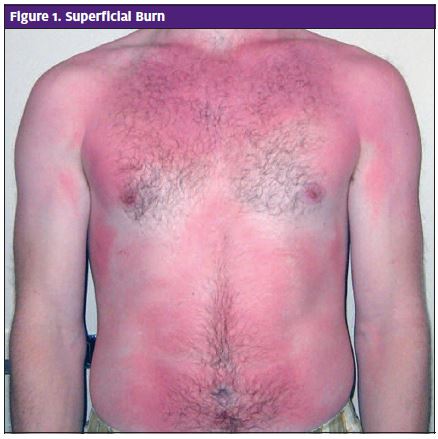
Superficial burns
Superficial burns involve only the epidermal layer of skin. They do not blister but are very painful, dry, and red, and will blanch with pres- sure. The classic superficial burn is sunburn (Figure 1). Redness is apparent within two hours of burning and is maximal within 12 hours. In two to three days, the redness and pain begin to subside; on day 4 or 5, the epithelium peels away from the newly healed epidermis. Superficial burns heal without scarring. Treatment is designed to improve comfort and is not required for actual healing. Topical treatment may include aloe, cool compresses with water, nonfat milk, or Burow’s solution. NSAIDs such as ibuprofen or naproxen may decrease pain and inflammation. Severe cases may respond to prednisone 1 mg/kg/day for three days. Narcotic pain medication may also be of benefit.
“Sun poisoning” is a syndrome of severe widespread sunburn associated with nausea, vomiting, and dizziness. IV fluids may be required in these cases. Local anesthetic containing topical preparations should be avoided; they are generally ineffective and may cause sensitization to the ingredients. Patients should be instructed to avoid sun exposure for three weeks. Patients should be questioned about the use of photosensitizing drugs such as tetracyclines, thiazides, sulfonamides, phenothiazines, sulfonylureas, griseofulvin, vitamin B6, and NSAIDs.
Partial-thickness burns
Partial-thickness burns can be divided into superficial and deep (Figures 2, 3, and 4). Superficial partial- thickness burns form blisters within 24 hours of injury between the epidermis and dermis. They are painful, red, may be weeping, and will blanch with pressure. They generally heal in seven to 21 days. If blisters break, a layer of fibrous exudate and debris may accumulate on the surface, which may cause bacterial colonization and delayed healing. Scarring is unusual, but skin changes may take months to dissipate. Pigment changes may occur. There is typically no functional impairment.
Deep partial-thickness burns extend deeper into the dermis, damaging hair follicles and glandular tissues. They are painful to pressure only. Blisters, if present, easily unroof. If absent, the skin may be wet or waxy dry, and may appear cheesy white or red. Blisters do not blanch with pressure. If no infection is present, they should heal without grafting in three to nine days. There is usually hypertrophic scarring, which may cause functional or cosmetic impairment. Grafting may be required in extreme cases.
Full-thickness burns
Full-thickness burns extend through and destroy all layers of the dermis and often injure deeper structures (Figure 5). Burn eschar, the dead and denatured dermis, may compromise the viability of a limb or respiratory function if on the torso or neck. A full-thickness burn is anesthetic. It can vary from waxy white to charred and black in color. The skin may appear and feel leathery. The skin is dry and inelastic and does not blanch with pressure. Hair falls out of the follicles easily. Blisters are not present. The full extent of injury may take several days to develop.
After several days, the wound eschar falls away from the underlying tissue, revealing unhealed granulation tissue. The wound heals by secondary intent, leaving contractures and scarring, which may be severe. Skin- grafting surgery is necessary to prevent deformity and facilitate healing. Full spontaneous healing, except in the smallest burns, is not possible without grafting. Fourth-degree burns are deep and potentially life-threatening. They extend through to fascia, muscle, and/or bone. Amputation or wide excision of deep tissue is required. The procedure itself may be life-threatening and disfiguring.
Immediate Care
Patients presenting with acute burns should have hot or burned clothing, jewelry, and obvious debris removed immediately to prevent further injury and constriction, and to enable accurate assessment.
Burned areas should be cooled using cool water or saline-soaked gauze. For small and moderate-size burns, cooling may minimize the zone of injury and certainly reduces pain. Although there is no specific time frame, duration of cooling is generally 15-30 minutes.
Ice and freezing should be avoided, as frostbite, hypothermia, and extension of burn damage can occur. Even with cool water, hypothermia may be a concern if more than 10% of total body surface area is burned.
Pain management
Burns hurt! Adequate pain management is essential and should not be withheld. Parenteral narcotics are of- ten required, sometimes in larger doses than are required for other injuries. It may be helpful to medicate patients before cooling, cleaning, and bandaging are undertaken. Regional anesthesia may be considered. Local injection or topical application of an anesthetic should not be used. Adequate narcotic prescriptions should be provided until the patient is able to follow-up. In addition, NSAIDs should be recommended for pain, as their antioxidant, anti-inflammatory, and anti-thromboxane properties may speed healing.
All burns should be cleaned by irrigation. Standard rec- ommendations usually include cool saline solution, but recent studies suggest that tap water may be reasonable. Skin disinfectants such as chlorhexidine and povidone/ iodine can act as an irritant and inhibit wound healing; as such, they are no longer recommended. Mild soap or antibacterial hand soap may be used, if necessary.
Intact blisters should not be unroofed. In most cases, they should be left in place unless rupture is impending or the blisters are in an area that will likely be traumatized and ruptured (eg, groin, bottom of foot, tip of finger, etc.). Needle aspiration is not recommended due to the increased risk of infection. The skin remaining from broken blisters should be carefully removed.
All partial- and full-thickness burns should have dressings after cleaning. Dressings prevent further trauma and infection, as well as increase patient comfort. Topical antibiotics should be applied to all partial-thickness burns unless the patient is being transferred to a burn center. A thin layer is preferred to copious application. Traditionally, silver sulfadiazine has been the first-line topical antibiotic. It should not be used on the face or in patients with sulfa allergies, pregnant women, newborns, or breastfeeding mothers.
Bacitracin, triple antibiotics (bacitracin, polymyxin B, neomycin), or polysporin (bacitracin, polymyxin B) may also be used. There are no studies proving the benefit of one over the other. Bacitracin is the least-expensive alternative; it may be preferred for this reason. It has been reported that 7%-13% of Americans are allergic to neomycin1; avoidance of triple antibiotics may therefore be prudent. Topical antibiotics should be continued until all wound epithelialization is complete.
A layer of non-adherent gauze should be placed over the antibiotic ointment. Loose strips of fine-mesh gauze (as opposed to continuous wrapping) should then be ap- plied to prevent constriction and provide protective padding and splinting of fingers and toes.
Fingers and toes should each be wrapped individually to prevent maceration of tissue when two burnt surfaces are adjacent. Gauze can be held in place with tubular- net gauze or loose wrapping.
Biologic dressings and bismuth-impregnated petroleum gauze are gaining popularity. At present, however, their use is largely limited to burn centers, where they are used on deeper wounds. They are applied only once and generally do not require changing. These dressings pro- mote lower rates of infection, are more comfortable, re- quire less pain medication, and promote faster healing. Conversely, biologic and impregnated-gauze dressings are expensive, difficult to apply, and have a narrow time frame for effective application: within six hours of injury. Occasionally, re-application is required if loosening occurs on day 2. The dressing will gradually peel off as wound epithelialization occurs, leaving fresh tissue beneath.
If the wound is deeper than appreciated or if infection occurs, a biologic dressing will be ineffective. In that event, grafting is required.
Brands of biologic dressings include Acticoat, Biobrane, and TransCyte. Amniotic membranes and animal products have shown promise as well. None of these dressing alternatives are practical in the urgent care setting at this point but may be useful options in the near future.
Tetanus
Tetanus status should be addressed for any wounds deeper than superficial thickness. In patients who have not received a complete primary immunization, tetanus immune globulin—as well as the primary immunization should be provided.
Antibiotics
Prophylactic antibiotics in any form are not recommended and have no proven benefit for the prevention of burn infections.
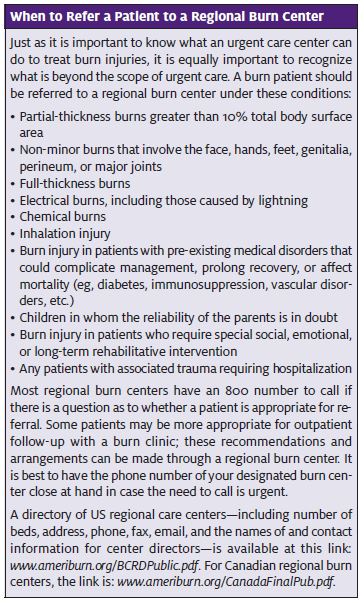
All patients who meet the criteria for serious burns should be transferred to a burn center (see When to Re- fer a Patient to a Regional Burn Center on page 18) .
However, initial difficulties in differentiating superficial partial-thickness burns from deep partial-thickness burns and full-thickness burns, as well as concerns about the unpredictable evolution of injuries, should make consultation with a burn surgeon a precaution to consider. This is especially true if burns are on the face, hands, perineum, or feet, or if burns are on high-risk patients (eg, individuals who are elderly, immunosuppressed, or diabetic).
Contacting a burn specialist can help with identification of patients who warrant follow-up and ensure appropriate and timely care that can prevent long-term damage. In addition, specialist consultation is a legally prudent course of action; the basis of a malpractice suit, particularly given the unpredictable course of burn injuries, could well be failure to seek specialist advice.
Reference
- Gehrig KA, Warshaw Allergic contact dermatitis to topical antibiotics: Epidemiol- ogy, responsible allergens, and management. J Am Acad Dermatol. 2008;58(1):1–21.