When an Uncommon—Potentially Catastrophic—Diagnosis Is Masked by a Common Complaint
In Bouncebacks, which appears quarterly in JUCM, we provide documentation of an actual patient encounter, discuss patient safety and risk management principles, and then reveal the patient’s “bounceback” diagnosis. This Bouncebacks case is unique in that it also went to trial, excerpts from which are also presented. This case is adapted from the Bouncebacks! Medical and Legal (Anadem Publishing) by Michael B. Weinstock, MD, and Kevin Klauer, DO, with risk management commentary by Gregory L. Henry, MD, past president of the American College of Emergency Physicians, and discussions by other nationally recognized medical and legal experts. It is available on Amazon.com. For more on Bouncebacks, visit www.embouncebacks.com.
MICHAEL B. WEINSTOCK, MD and JILL C. MILLER, MD
A case like this is not soon forgotten. It raises haunting questions: Is the “worst headache of my life” pathopneumonic for anything?How do we reconcile abnormal results with a conflicting clinical story? Have you ever been guilty of “diagnosis momentum”? What is the role of advanced-line antibiotics in the treatment of sinusitis?
Why such questions are haunting will soon become evident. A young mother of three. A common complaint. A tricky diagnosis. A tragic result. Like TV’s Law and Order, this case unfolds in two parts: The Medical Record and The Legal Record.
PART I. THE MEDICAL RECORD
The Patient’s Story
In 1999, Kelli Flood, age 32, had held a good job at Stem Outdoor Advertising. She made just under $50,000 per year. She was smart and pretty and had a sharp wit and a good work ethic. She and her second husband, Shane, were married on October 28, 1998, and took a honeymoon at a Sandals resort in the Caribbean.
Several days after the birth of their son, Jacob, on July 30, 1999, Kelli presented to her primary care physician with a headache and was diagnosed with sinusitis. She was given amoxicillin. The headaches continued to the point where, on August 8, she said her head pain was “indescribable, like my head was going to come off or split in two.”
That afternoon, a Sunday, at around 6 pm, Shane drove Kelli to the emergency department of the local hospital. Here is the first of two perspectives on what happened next.
The Doctor’s Version
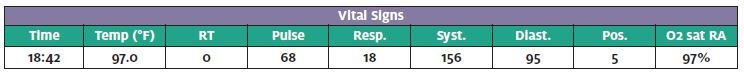
(The following, as well as other case notes to be presented, is from the actual documentation of the providers involved.) Chief complaint as noted by the triage RN (August 8, 1999: 18:32): Throbbing head, migraine comes on suddenly.
Nurse’s note: Headache has happened 3 times in past 7 days, c/o pain in the forehead and back of head. This headache was of sudden onset ½ hour ago. Had an epidural (with delivery). Ice to forehead, crying, headache 10/10.
History of present illness (18:55): This patient is a 32- year-old female who is 8 days postpartum. [Headache] began spontaneously at 1800 and is the worst one of her life. She was asleep and awoke with the discomfort. She was dx with sinusitis 5 or 6 days ago by her primary care doctor and placed on amoxicillin 500 mg tid. Since that time, the patient has had 2 other headaches, which were not quite as severe. HA is frontal and bi-temporal with photophobia and nausea but no vomiting. There is no phonophobia, numbness, or tingling.
PAST MEDICAL HISTORY
Allergies: Sulfa (swelling)
Meds: Amoxicillin, Tylenol extra strength, prenatal vi- tamins
PMH/PSH: Negative
Surgery: C-section 1987, broke arm 16 years ago, laparo- scopic surgery 1990
FH: Father diabetes
PHYSICAL EXAMINATION
Constitutional: A&O x 3. Patient does appear to be moderately uncomfortable.
Skin: No lesions are identified.
Eyes: EOMI. PERRL. Fundi are normal.
ENT: Minimal nasal mucosal erythema. The pharynx is normal. Bifrontal tenderness to palpation.
Neck: Supple, without masses. No LAN.
Lungs: CTAB.
Heart: RRR without rubs, clicks, or murmurs. Neurologic: Evaluation includes sensory, motor, cerebellar, and cranial nerve II-XII. Examination is intact. No meningeal signs are present.
MEDICAL DECISION MAKING
19:50: After discussing the possible effect of narcotics on the baby, who is being breast fed, mother did agree to an injection of Demerol 75mg IM and Phenergan 25mg IM. 20:15: Repeat vitals: pulse 64, respirations 18, BP 176/50.
Doctor’s progress note
Patient had moderate relief of pain with meds. She has cephalgia, which I believe is related to sinusitis, and I will switch her to Biaxin, Darvocet, and Entex LA. Recheck in 3 to 4 days if there is no improvement in the overall symptoms, sooner if worse. Released ambulatory at 20:35.
DIAGNOSIS
- Acute
- Acute cephalgia
Seth Hockenberry, MD
Patient Safety and Risk Management Issues
(Authors’ note: It is obvious from the progress note that this doctor cared about his patient. He not only spent a lot of time with her, he informed her when and why to return. The fol- lowing are some considerations about the initial evaluation.)
Error 1: Anchoring bias and diagnosis momentum Discussion: Once the emergency physician found erythematous nasal mucosa and “sinus tenderness,” he anchored on a diagnosis of sinusitis. This was likely coupled with diagnosis momentum, as the patient was actually taking amoxicillin for a previous diagnosis from her primary care doctor.1 Curiously, there was no documentation of clinical sinus symptoms such as rhinorrhea, post nasal drip, facial/tooth pain, or fever.
Teaching point: It is hard to diagnose sinusitis with- out symptoms of sinusitis.
Error 2: Differential diagnosis was too narrow Discussion: Whereas the two most immediately-concerning diagnoses in patients with nontraumatic headache remain subarachnoid hemorrhage (SAH)2-4 and meningitis, there are other “can’t miss” secondary causes of headaches, including:
- Brain mass
- Temporal arteritis
- Pseudotumor cerebri (idio- pathic intracranial hyper- tension)
- Carbon monoxide toxicity
- Acute angle-closure glaucoma
- Carotid artery dissection
- Cavernous sinus thrombosis
- Preeclampsia/eclampsia5-6
Regarding the “can’t miss” diagnosis of SAH, Kelli did give a history of sudden-onset headache, a symptom more concerning than “the worst headache of my life” (which also was present in her story). The onset always needs to be elicited in the headache history, and when a patient answers “sudden,” further questioning should establish whether it reached maximum intensity in one minute or less.
The “worst headache of life” is a commonly elicited history but really doesn’t mean much. After all, the first headache of your life is, by definition, both the worst and most benign headache you have ever had. But the fact that this patient had both sudden onset and intense pain required the physician to exclude SAH by a combination of CT scanand lumbar puncture (if the CT is negative).
Preeclampsia was concerning in Kelli Flood’s case since her headache was coupled with increased blood pressure. Preeclampsia/eclampsia can occur up to 30 days postpartum. The problem is that a headache (pain) can also cause the blood pressure to go up. Additional findings with preeclampsia may include:
- Hyperreflexia/clonus
- Abdominal pain
- Proteinuria
- Lack of a previous history of hypertension
Note: These are clinical signs that can be easily evaluated in an urgent care setting. Another easily derived diagnosis is post-dural puncture headache. These are worse when sitting up and better when lying flat, a diagnosis arrived at by his- tory alone. Kelli was postpartum but history of delivery was not elicited.
Primary headaches include the following:
- Migraine n Tension n Cluster
- Narcotic withdrawal
- Stress headaches
However, none of these was consistent with Kelli’s presentation.
Teaching point: Maintain a high index of suspicion for high-risk headache patients.
Error 3: Over-reliance on antibiotics for sinusitis
Discussion: Sinusitis is usually viral. The number needed to treat (NNT) with antibiotics to get one patient better faster is between 8 and 12. When the decision is made to use a second-line antibiotic (eg, macrolide, quinolone) instead of a first-line antibiotic (eg, amoxicillin, TMP/SMZ, doxycycline), the NNT skyrockets to 100.7 In other words, when a patient fails on amoxicillin, you would need to dispense 100 prescriptions at a cost of $100 for each medication (total cost: $10,000) to get one patient better faster. While it would have been okay to “bump up” the antibiotic from amoxicillin to clarithromycin in Kelli’s case, that she failed to improve on an antibiotic in the first place should have prompted a re-evaluation of the diagnosis.
Teaching point: Sinusitis is overdiagnosed and effect of antibiotics is overstated.
Error 4: Medical decision making
Discussion: “Confirmation bias” is the practice of find- ing evidence to support a diagnosis (as opposed to look- ing for data to disprove it).1 If an objective third party had looked at Kelli’s history without knowledge of her recent treatment for sinusitis, it is unlikely that doctor would have arrived at this diagnosis.
Teaching point: Gather evidence first and make a diagnosis based upon your findings.
THE ED BOUNCEBACK
The next day, Kelli’s headache worsened. She fixed din- ner but didn’t eat anything. “I went into the bedroom, because that’s where Jake was, and I couldn’t see him,” she testified later in court. “I yelled for Shane and said, ‘I can’t see the baby.’ So I sat down on the steps of the bathroom and I just don’t remember anything else.”
Kelli began to shake all over, her eyes rolled back in her head, and she was foaming at the mouth. Shane called 911.EMS note Found sitting on steps. She does not respond to verbal commands and is disoriented as to time and place. Glucose is 92.
The ED record
- Chief complaint (21:32): Possible seizures.
- Vital signs: Temp 97.4, pulse 78, resp 16, BP 172/99, sat 97% RA.
- PE: Pt. moaning with pain and shaking her head from side to side and crying. Knows answers to ques- tions. At times ignores questions. No gross neurolog- ical deficits.
- CT brain: No bleed or shifts. Small ventricles without signs of cerebral edema.
- Testing: Labs normal. CXR: no infiltrates. UA normal. n ED course: The patient’s BP did go up to 190/115, with worsened headache and crying. Mental status re- mains unchanged. Lasix IVP. Nipride drip. Demerol 25 mg and Phenergan 25 mg IV.
- Discussion with spouse: I stated to the husband that she may have encephalitis, and an LP was indi- cated. Further, acyclovir will be started, depending upon the results of the LP.
- Neuro consult: I spoke with Dr. Quinn, the neurol- ogist on call, and the decision was made not to do the LP since our lab is limited. The patient was admitted to the ICU.
FINAL DIAGNOSIS
- Severe cephalgia with acute mental status change and possible first-time
- Consider encephalitis, herpes
- Cannot entirely rule out a herald bleed with unde- tectable subarachnoid hemorrhage at this
Robert Carozza, MD
(Authors note: Hmmm … who has ever consulted a neurol- ogist and been talked out of an LP? This is a reportable event! There were still several diagnostic possibilities on the table, which the second ED physician had not ruled out, including subarachnoid hemorrhage, herpes encephalitis, meningitis, and eclampsia.)
HOSPITAL COURSE
- MRI showed ischemic changes in the right cerebellar cortex. EEG was unremarkable. Lumbar puncture:
- WBC 1, RBC 84, protein 77, glu- cose 46.
- Repeat MRIs showed cerebral infarcts in the frontal, parietal, and occipital lobes.
- On August 19, 1999, 10 days after admission, Kelli had an- other seizure and was transferred to a tertiary care facility.
- The differential now included postpartum cerebral angiopathy, cerebral vasculitis, and eclampsia. Kelli was treated presumptively with high-dose IV steroids and magnesium.
- At discharge, Kelli was mildly responsive and occasionally interactive.
FINAL OUTCOME
Kelli was left irreversibly triplegic. She lives at home and is cared for by her husband.
PART 2. THE LEGAL RECORD
Why sue?
Kelli Flood had a horrible outcome: a young mother, now triplegic, requiring lifelong medical care and assistance. Before her turn for the worse, she was sitting in the hospital room playing cards with her husband, waiting to go home to be with her family and newborn child. Suddenly she experienced a seizure from which she would never recover. It is not difficult to see why this family would file a malpractice suit.
Plaintiff attorney to Kelli Flood (plaintiff) on Day 6 of the trial
Would you describe Jacob for us?
A. He’s a wonderful little He’s three and a half. He is extremely active. He’s just … I can’t say enough about him. I’m a very proud mother.
Q. What are some of the things that you like to do with Jacob?
A. I like to help him count and teach him his I like to play “This Little Piggy” with him. He climbs up and sits on my lap. I let him brush my hair. He likes to read to me. He can’t read, but he likes to tell me stories that he makes up. He pretends. He likes to help me with anything I ask him to do. If I ask him, “Get Mommy a drink of water, would you, Jacob?,” he’ll run and get it. If I need a Kleenex, he runs and gets it.
Q. Does Jacob love you?
A. Yes, he does.
Q. How do you know that?
A. Because he tells me He throws his arms around my neck and says, “Mommy, I love you.”
THE ACCUSATION/CAUSE OF ACTION
Civil complaint
Plaintiff requires the use of a wheelchair and has only the use of her left hand. Prior to this event, plaintiff was the active mother of three children. She seeks past medicals of $561,266, future medicals of $10,393,754, and future wage loss of $1,300,000.
Synopsis of the court record
At trial, Kelli’s attorney argued that Seth Hockenberry, the first emergency physician to see her, failed to differentially diagnose postpartum preeclampsia and/or eclampsia and failed to presumptively treat her with magnesium sulfate.
THE TRIAL (January 2003)
(Author’s note: What follows are selected excerpts of testimony from the actual court record. Have you ever sat in a courtroom for two weeks while eight non-physicians decided whether your care was appropriate? Close your eyes, visualize world peace … then make sure your headache differential includes preeclampsia.)
Judge’s instructions to the jury
Good morning, ladies and gentlemen. Today is the 15th of January, 2003. We convene in Flood vs Hockenberry. Openingstatements will give you a preview of what the respective attorneys believe this case will show. In any lawsuit, the plaintiffs go first because they have the burden of proof.
This is not a criminal case and the burden of proof that you may have heard of about “beyond a reasonable doubt” does not apply in this case. In a civil lawsuit, the plaintiffs have the burden of proving their suit by a preponderance of the evidence, which is the greater weight of the evidence. That is evidence that you believe because it outweighs in your mind the evidence opposed to it. Are counsels ready to proceed with opening statements?
Opening statement by the plaintiff attorney
Good morning, ladies and gentlemen. I want to start out by talking a little bit about some rules that doctors fol- low, rules they learn in medical school and apply every day. Doctors have a duty to use ordinary care what a reasonably cautious doctor would do in the same situation. Those are rules you’ll follow, too, when you decide this case. There’s going to be a word mentioned by every doctor who testifies in this case. That word is “eclampsia.” It has been known for many, many years. A couple of things about eclampsia. Number one, fifty thousand women a year die from eclampsia. Number two, that’s in the world, okay? In the United States, ninety thousand to a hundred thousand women are diagnosed with a condition called “preeclampsia.” It is the second-leading cause of maternal death in the United States. Every textbook that’s on the subject talks about. Every doctor knows, or should know, what it is.
What is eclampsia? Eclampsia is a disease. These are not disputable things. Any woman who is pregnant or has recently delivered a baby can get it. Some people used to think that it was a toxin, a poison that would go through your body. That’s why it was [once] called “toxemia.” I look at it like a snake bite. If you get a snake bite, you’ve got to do something quick. If the poison goes through, well, what do you do? You go get the serum, right, to stop the poison. Well, there’s a serum in talking about eclampsia. It’s a drug called magnesium sulfate. Doctors use the [term] that it’s the “drug of choice.” That’s what they say. It’s the drug. In a study published in the New England Journal of Medicine, there were 1,049 patients who had eclampsia. They gave them magnesium sulfate. Guess how many of the thousand forty- nine continued to have seizures? Zero. It’s been known for a hundred of years. It’s the drug of choice.
Now, I mentioned preeclampsia; you have preeclampsia before you have eclampsia. The body gives out warning signs. So, what are the warning signs? There’s not much dispute here. Number one, you’ve got to be pregnant or postpartum. Number two is high blood pressure. There’s also often a severe headache, visual disturbances like photophobia, protein in the urine, brisk reflexes, nausea, and upper quadrant [abdominal] pain.
How does a doctor go about finding these signs? Easy. He takes a history. What happened? Are you pregnant? Recently been pregnant? Have you had headaches? Visual disturbances? Nausea? What’s the second way they do it? Lab tests, for example, proteinuria. What’s the third? An exam. So, history, exam, and testing.
Some other things about eclampsia that will be interesting to you. I call them truisms because they’re true about this disease. Number one, it gets worse if it’s untreated. It can move from preeclampsia to eclampsia in a short amount of time. That’s why it’s a medical emergency. How do you treat it? Mag Sulfate.
Okay. July 30, 1999, we’ve got a couple proud parents. Kelli Flood delivered a baby it was a pretty happy time. On August 8th, eight days postpartum, it’s the first opportunity to help Kelli. Kelli is seen by Dr. Hockenberry. Kelli was in bad shape. She was crying. She had [a severe] headache, she had visual changes, photophobia, nausea. He takes her blood pressure. It’s 156/95. Dr. Hockenberry thought that a cold was causing the most severe headache of her life and that the high blood pressure was caused by the pain. So he gave her a shot of Demerol. The headache got better, but the blood pressure went up. The pain was less and the blood pressure was more. It went from 156 to 176.
Do you know what he didn’t do? Order a urinalysis. This is no big complicated test; you pee into a bottle and check it with a dipstick. He didn’t do that. [And] He did- n’t check her reflexes.
Kelli was a career woman. She made $45,000 a year. She hasn’t worked since and will never work again. This is a picture of her family, her kids. [Shows photo to jury.] She can do a few things. She can read to them if the print is big or if she has a magnifying glass. She can count numbers a little bit. But she can’t throw a ball. She can’t drive to soccer. Kelli is frozen in her own body, and it was preventable.
Direct examination of the plaintiff expert witness by the plaintiff attorney
Q. You would agree that Mrs. Flood had a condition difficult to diagnose?
A. No, I wouldn’t agree to that, actually.
Q. I take it that you have criticisms of the physician?
A. That’s correct.
Q. In your review, were you able to formulate a diagnosis as to Mrs. Flood’s condition?
A. Yes.
Q. And would you please tell me what your diagnosis was in that regard?
A. I believe she had eclampsia. It is a continuum of the disease, and she presented in two different stages.
Q. Did you make a differential diagnosis?
A. Yes. First was eclampsia, second would be eclampsia, third would be eclampsia, fourth would be other causes of an intracranial process. And I’m going to lump them together for you: various forms of stroke, vasculitis, or infection but these would fall far beneath [eclampsia in probability]. Given the symptom complex and its findings,[eclampsia] is far and away the most likely diagnosis.
(Author’s note: There was much more to this trial: a claim that Kelli in fact did not have eclampsia but a different diagnosis called “postpartum cerebral angiopathy, allegations against other
players involved in her care—including the neurologist, and striking testimony from Kelli herself, given from her wheelchair. We jump now to the verdict.) The judge’s Instructions to the jury (January 29, 2003)
THE TWIST
As the jurors left the courtroom to deliberate, there was a flurry of activity on both sides. A defense offer of $500,000 to settle the case had already been declined, but an emergency call from the insurance company reached the defense attorney, cell phone in hand. The new offer: $750,000. This was conveyed to the plaintiff attorney who, after deliberating with Kelli in a hotel room across the street, declined the offer.
Panic ensued as the insurance company was told of the rejection. The ante was upped to $1 million. Additional telephone calls were placed, but the offer was again rejected by the plaintiff.
A preverdict assessment by the defense attorney
I felt from a scientific standpoint we had a winner, but I kept looking at a lady in a wheelchair. I was not confident [the jury] would walk away from her. They were asking for $15 million, which I did not think they would get, but I would not be surprised with $4-$5 million. Our defendant was very good.
THE VERDICT
Judge: It’s January 29, 2003. The record should reflect that the parties are all present, with counsel. The jury has indicated that they have reached verdicts. Mr. Long,
I understand you were selected as the foreperson.
Jury foreman: Yes, Your Honor.
Judge: Congratulations. Have you reached verdicts? Jury foreman: Yes, we have, sir. We, the jury, being duly impaneled, sworn, and affirmed, find for the defendants with respect to the claim against the defendant.
Summary
Seven jurors found for the defendant physician, Seth Hockenberry.
Judge: Ladies and gentlemen of the jury, this obviously was a long and very difficult case. Throughout the trial, as I would look over and watch you folks, I know you didn’t take your job lightly. I appreciate [the sacrifice of your time]. The parties had a dispute they couldn’t re- solve. Our system says that we call upon eight citizens to help resolve the issues. You did everything you were called upon to do. You should be proud of your service.
(Author’s note: The jury split 7-1, voting for the physician defendants. After the trial, the lead defense attorney was standing in the hall and saw the plaintiff being wheeled out of the courthouse. The wheelchair was being pushed by two people; one was the lone juror who voted for the plaintiff. When they exited the courthouse, she helped load the defendant into the van.)
POST-TRIAL REFLECTIONS FROM THE ATTORNEYS WHO ARGUED THIS CASE
The defense attorney
The jury didn’t buy whether two ED doctors ought to have been able to diagnose postpartum eclampsia when an OB [who had testified at 450 trials] had only seen it once.
The plaintiff attorney
- I think about this case at least once a week.
- The ED docs won the case as they [the jury] thought, “If a neurologist couldn’t diagnose it, how could we expect an ED doc to [make the diagnosis].”
URGENT CARE EVALUATION OF POSTPARTUM HEADACHE
Evaluation of headache in the urgent care is tricky, as most headaches are benign and self-limiting—except the headaches that are life-threatening! It is the bold and risk- taking physician who ignores abnormal findings while continuing to “play the odds” with a diagnosis of sinusitis. Whereas blood pressure is often increased from pain, the plaintiff attorney was exactly right: Why would the repeat BP be higher if Kelli’s pain was less?
Including preeclampsia (which can occur up to 30 days postpartum) in the differential would have allowed for simple bedside testing of reflexes, including clonus and proteinuria, and possibly an OB consult.5-6 If a 30-second phone call had been made to Kelli’s obstetrician, you might not be reading this case.
So, how can we find a needle in the haystack of common diagnoses?
First, just as a patient with untreated AIDS and a headache would automatically bring to mind meningitis or a mass, our postpartum patient represents a unique subset of patients. Consideration should be given to preeclampsia as well as to headaches that occur in post-partum patients, such as post-LP headache, cerebral venous sinus thrombosis, pituitary apoplexy, and sub- arachnoid hemorrhage.8
Second, if sinusitis is not improving, the first consideration should be to reassess the diagnosis.9-12 The data shows that the NNT with a second-line antibiotic com- pared to a first-line antibiotic for sinusitis (amoxicillin, TMP/SMZ, doxycycline) is 100. Do we really think that Kelli had the 1 in 100 case that needed advanced antibiotics? Third, though this sounds like a broken record, vital signs are called vital for a reason. The plaintiff attorney had a field day with the second (elevated) blood pressure check. “Why would the blood pressure go up,” he repeatedly asked, “if the pain went down?”
If there is an abnormal test result, particularly in light of diagnostic uncertainty, a note should be recorded explaining the medical decision-making process. n
References
- Croskerry Achieving quality in clinical decision making: cognitive strategies and de- tection of bias. Acad Emerg Med. 2002;9(11):1184-1204.
- Edlow JA, Caplan Avoiding pitfalls in the diagnosis of subarachnoid hemorrhage N Engl J Med. 2000;342(1):29-36.
- van Gijn J, Rinkel Subarachnoid haemorrhage: diagnosis, causes and management. Brain. 2001;124(pt 2):249-278.
- Edlow JA, Malek AM, Ogilvy Aneurysmal subarachnoid hemorrhage: update for emergency physicians. J Emerg Med. 2008;34(3):237-251.
- Chames MC, Livingston JC, Ivester TS, et Late postpartum eclampsia: a preventa- ble disease? Am J Obstet Gynecol. 2002;186(6):1174-77, 2002.
- Stella CL, Jodicke CD, How HY, et Postpartum headache: is your work-up complete? Am J Obstet Gynecol. 2007;196(4):318 e1-e7.
- Anon JB, Jacobs MR, Pool MD, Singer First-line vs second-line antibiotics for treat- ment of sinusitis. JAMA. 2002;287(11):1395-1396.
- Katzin LW, Levine M, Singhal AB. Dural puncture headache, postpartum angiopathy, pre-eclampsia and cortical vein thrombosis after an uncomplicated Cephalal- gia. 2007;27(5):461-464.
- Silberstein Headaches due to nasal and paranasal sinus disease. Neurol Clin. 2004 Feb;22(1):1-19, v.
- Eross E, Dodick D, Eross The Sinus, Allergy and Migraine Study (SAMS). Headache. 2007;47(2):213-224.
- Jones Sinus headaches: avoiding over- and mis-diagnosis. Expert Rev Neurother. 2009;9(4):439-444.
- Williams JW, Jr, Simel Does this patient have sinusitis? Diagnosing acute sinusitis by history and physical examination. JAMA. 1993;270(10):1242-1246.