Urgent message: Although free air in the mediastinum is generally a benign, self-limited condition, most patients should be admitted to the hospital and observed for signs of serious complications, which could be fatal.
By Tracey Quail Davidoff, MD
A previously healthy 17-year-old male presents to urgent care with a one-week complaint of sore throat, fever, and nasal congestion. On the last day, he had experienced sharp chest pain, which worsened with deep inspiration, swallowing, and laying flat. The pain improved when he sat up. He has never experienced this pain before. On exam, the vital signs are:
- T: 97.1
- P: 74
- R: 14
- BP 109/72
- Oxygen Saturation is 100% on room air
The patient appeared anxious and was bending forward and holding his chest. There was no jugular venous distention. The trachea was midline. Breath sounds were uniformly decreased, possibly due to poor effort and splinting. A crunch could be heard on auscultation of heart sounds, which were otherwise normal.
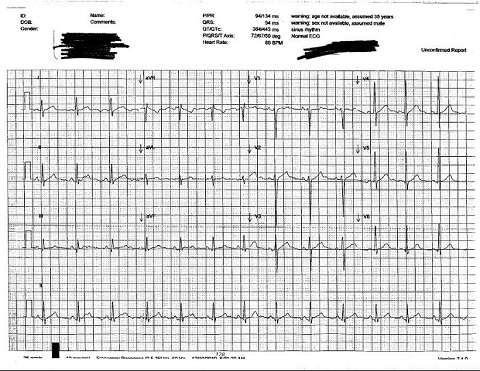
The ECG was normal (Figure 1).
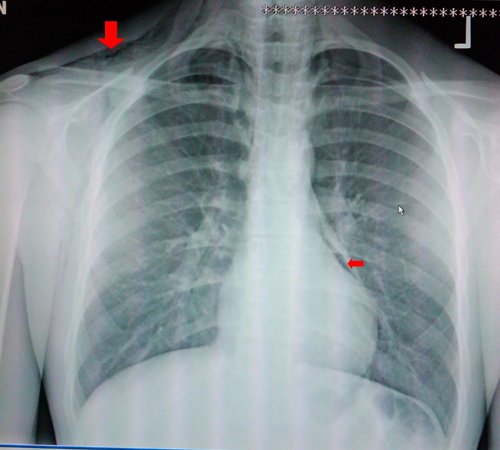
The post-anterior CXR showed subcutaneous emphysema in the right shoulder and neck area, as well as pneumomediastinum, especially noted on the left heart border (Figure 2). On the lateral CXR, air was noted in the pericardium behind the sternum (Figure 3).
Figure 2. Post-anterior chest.
Pneumomediastinum is defined as free air in the mediastinal structures. This can occur spontaneously when intrathoracic pressures become elevated, such as during an exacerbation of asthma, coughing, vomiting, childbirth, seizures, and Valsalva maneuver. Spontaneous pneumomediastinum generally occurs in young, healthy patients without serious underlying pulmonary disease, mostly between 15-40 years of age.
Risk factors include inhalation drug use (eg, marijuana, cocaine); asthma; athletic exertion; respiratory tract infection; childbirth; emesis; especially forceful, severe cough; mechanical ventilation; and respiratory or upper gastrointestinal endoscopy. Ruptured esophagus from forceful vomiting, known as Boerhaavefs Syndrome, is life-threatening.
Patients may or may not present with symptoms, as pneumomediastinum typically is a well-tolerated disease. A study of 24 adult patients with spontaneous pneumomediastinum found that 67% of subjects had chest pain; 42% had persistent cough; 25% had sore throat; and 8% had dysphagia, shortness of breath, or nausea/vomiting.1 Chest pain usually radiates to the neck, back, or shoulders and is exacerbated by deep inspiration, coughing, or supine positioning. Neck pain, jaw pain, dysphagia, dysphonia, and/or abdominal pain may also occur but are unusual.
A physical exam most commonly reveals subcutaneous emphysema. Hammanfs sign is a precordial crunching noise occurring with each heartbeat and is rarely present. Many patients have no physical findings.
Chest radiography shows a thin line of radiolucency outline the cardiac silhouette, and thin, lucent, vertical streaks of air within the mediastinum. The aorta and hilum are highlighted, and there may be a ring around the right pulmonary artery. Subcutaneous emphysema may be seen in the shoulders and neck. Pneumothorax may also be present and may require an expiratory film to be visualized. Air may also be visible in the retrosternal space on the lateral view. If esophageal rupture is suspected a contrast-enhanced esophagography should be performed. A CT scan may improve diagnostic sensitivity in pneumomediastinum; if clinical suspicion is present, it should be obtained.
Pneumomediastinum is generally a benign, self-limited condition, with the exception of esophageal perforation. The mortality rate is as high as 70% in patients with Boerhaave’s syndrome, even with surgical intervention. Most patients with pneumomediastinum should be admitted to the hospital and observed for signs of serious complications such as pneumothorax, tension pneumothorax, and mediastinitis.
Reference
1. Koullias GJ, Korkolis DP, Wang XJ, Hammond GL. Current assessment and management of spontaneous pneumomediastinum: Experience in 24 adult patients. Eur J Cardiothorac Surg. 2004;24:852-855.