Michael B. Weinstock, MD, Ana Echenique, MD, DABR, Joshua W. Russell, MD, MSc, FACEP, Ari Leib, MD, Jordan A. Miller, DO, David J. Cohen, MD, Stephen Waite, MD, Allen Frye, NP, and Frank A. Illuzzi, MD, FACEP
Abstract
Background/Objective
Patients with COVID-19 commonly present to Urgent Care (UC) centers. Our primary objective was to determine what percentage of UC patients with confirmed COVID-19 had normal vs abnormal chest x-rays (CXR). Secondarily, we aim to describe specific imaging characteristics and the frequency of each abnormal findings on plain film radiography (CXR).
Methods
A database of a large UC company in the greater New York City (NYC) area was reviewed for patients with positive SARS-CoV-2 PCR tests who also underwent CXR in UC between March 9 and March 24, 2020. Eleven board-certified radiologists, with knowledge that they were only reading imaging studies of COVID-19 patients, were each given a subset of the CXRs with oral and written instructions to re-read the films while disregarding the initial reading. Their readings were classified as normal, mild, moderate, or severe disease. They subsequently characterized specific findings. Lastly, overreads were compared with the initial CXR reading.
Results
Of the 636 CXRs reviewed among patients with confirmed COVID-19, 363 were male (57.1%) and 273 were female (42.9%). Patient ages ranged from 18 to 90 years of age, with most (493 patients, or 77.5%) being 30─70 years old. There were 371 CXRs re-read as normal (58.3%). Of the 265 abnormal cases (41.7%), 195 demonstrated mild disease, 65 demonstrated moderate disease, and five demonstrated severe disease. Interstitial changes and ground glass opacities (GGO) were the predominant descriptive findings in 151 (23.7%) and 120 (18.9%) of the total, respectively. Location of the abnormalities were in the lower lobe in 215 (33.8%), bilateral in 133 (20.9%), and multifocal in 154 (24.2%). Effusions and lymphadenopathy were uncommon.
Discussion
This is the first study to specifically explore CXR findings of patients with confirmed COVID-19 evaluated in a UC setting. The vast majority of patients (566/636) had either normal or only mildly abnormal CXRs (89%), despite being symptomatic enough to warrant imaging as determined by the treating UC provider.
Conclusion
CXRs obtained from confirmed and symptomatic COVID-19 patients presenting to the UC were normal in 58.3% of cases, and normal or only mildly abnormal in 89% of patients. When abnormal, the most common findings were present in the lower lobes and the pattern was interstitial and/or multifocal. Pleural effusions and lymphadenopathy were uncommon.
INTRODUCTION
COVID-19, a novel disease caused by the SARS-CoV-2 virus, rapidly became a pandemic in early 2020, resulting in considerable worldwide morbidity and mortality.1,2 During this outbreak, acute care clinicians have been striving to accurately diagnose and define its clinical features in order to provide the best care for afflicted patients and limit the spread of the disease.
Plain film radiography of the chest (CXR) is a relatively inexpensive and widely available diagnostic modality in urgent care (UC) centers. However, to date, there is little evidence describing the utility of CXR in identifying patients with suspected COVID-19. Early observational studies discussing characteristic patterns of radiographic findings have focused predominantly on the use of computed tomography (CT) imaging. While CT has demonstrated good-to-excellent sensitivity (56%-91%) for COVID-19 lung pathology, depending on the interval between symptoms and imaging, cost and practical considerations (eg, sterilization after use) limit its utility, especially for use among ambulatory patients.3-6
As most patients with COVID-19 seem to have a mild course of respiratory illness, evaluations are most likely to take place in nonemergency department and nonhospital settings, such as UC centers.1 In such settings, CXR is by far the most widely available imaging modality.7 However, to date all published studies of thoracic imaging findings in patients with COVID-19 have focused on hospitalized patients.8 Among such patients, Wong, et al found that the initial CXR had a sensitivity of only 69% for any abnormality.3 One would expect because UC patients typically have less severe disease, that CXRs among such patients would have even lower sensitivity compared with hospitalized patients.
In the Wong, et al study, the most common radiographic features in confirmed COVID-19 patients were peripheral rounded consolidations, ground glass opacities (GGO), and pulmonary nodules. Distribution of the lung changes were more common in the lower zones and bilateral.3 Even in asymptomatic patients, radiographic progression of disease, from focal unilateral changes to diffuse GGO and consolidations, was observed.8 Pleural effusions were rare and were associated with an increased risk of poor outcome.3 Overall, the imaging changes reported peaked on days 10-12 of illness.3,8
Our primary objective in this study was to determine what percentage of patients with confirmed COVID-19 had normal vs abnormal CXRs. Secondarily, we aimed to describe the frequency of each specific type of abnormal finding on plain film radiography (CXR).
METHODS
The electronic medical record (EMR) database of a large UC network with over 100 centers in greater New York City (NYC) and New Jersey (NJ) was queried, and 718 patients who had tested positive for SARS-CoV-2 by PCR between March 9 and March 24, 2020 (during the time that greater NYC was the epicenter for COVID-19) were identified. The CXRs for these patients were initially divided among 14 board-certified radiologists. However, due to willingness and ability to participate due to difficulty with remote access, only 12 were able to participate in the study. These individuals were assigned approximately 50 CXRs each, except for two of the radiologists who reviewed an additional 50 CXRs each to make up for the two radiologists who were not able to participate, giving these two radiologists a total of approximately 100.
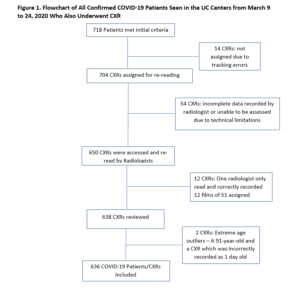
Most participants re-read and correctly resulted 47 to 100 films. However, one radiologist only read 12 films; these readings were excluded from this report because the number of cases was far below the contributions of the other participants, providing a total analyzed sample of 636 CXRs (Figure 1).
Figure 1. Flowchart of All Confirmed COVID-19 Patients Seen in the UC Centers from March 9 to 24, 2020 Who Also Underwent CXR
Participating radiologists were given oral and written instructions to first categorize films as normal, mild, moderate, or severe disease; for those classified as abnormal, they were asked to describe the specific findings. Initial CXR readings were part of these patients’ medical records, but the radiologists were instructed to ignore the initial reading when they re-read the images. Participating radiologists were informed that the CXRs were from patients with confirmed COVID-19.
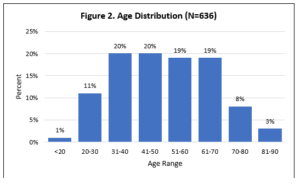
RESULTS
Eleven board-certified radiologists re-read CXRs of patients with PCR confirmed COVID-19 from multiple UC centers in the greater NYC area. Most participants re-read from 47 to 100 films, providing a total sample of 636 CXRs. Of these, 363 were male (57.1%) and 273 female (42.9%). Patient ages ranged from 18 to 90 years of age, with 493 patients (77.5%) being in the age range of 30─70 years old (see Table 1 and Figure 2).
| Table 1. Demographics of UC Patients with COVID-19 Whose CXRs Were Re-Read by the 11 Radiologists (N=636) | |
| Gender | n (%) |
| Male | 363 (57.1%) |
| Female | 273 (42.9%) |
Of the 636 CXRs included in this report, 371 were re-read as normal (58.3%). Of the 265 abnormal cases (41.7%), 195 were classified as mild disease, 65 were classified as moderate disease, and five were classified as severe disease. Interstitial changes and GGO were the predominant descriptive findings in 151 (23.7%) and 120 (18.9%) of the total, respectively. Location of the abnormalities were in the lower lobe in 215 (33.8%), bilateral in 133 (20.9%), and multifocal in 154 (24.2%). Effusions and lymphadenopathy were uncommon (see Table 2).
| Table 2. Characteristics of the Radiographic Findings Reported by the Panel of 11 Radiologists Who Re-Read CXRs of COVID-19 Patients Seen in Greater NYC UC Centers from March 9 to 24, 2020. (N=636) | ||
| Radiologic properties | Categories | n (%) of total |
| Severity | Normal | 371 (58.3%) |
| Mild | 195 (30.7%) | |
| Moderate | 65 (10.2%) | |
| Severe | 5 (0.8%) | |
| Type of infiltrate | Interstitial | 151 (23.7%) |
| Ground Glass Opacities (GGO) | 120 (18.9%) | |
| Consolidation | 34 (5.3%) | |
| Location | Lower | 215 (33.8%) |
| Upper | 128 (20.1%) | |
| Diffuse | 6 (0.9%) | |
| Focality | Multifocal | 154 (24.2%) |
| Focal | 71 (11.2%) | |
| Laterality | Bilateral | 133 (20.9%) |
| Centrality | Peripheral | 225 (35.4%) |
| Central | 45 (7.1%) | |
| Other | Effusions | 2 (0.3%) |
| Lymphadenopathy | 2 (0.3%) | |
Note: Numbers do not add to 100% as some patients had more than one finding.
The original readings from the medical records classified 468/636 (73.6%) CXRs as normal. When the CXRs were re-read for this study with the knowledge that the patients had COVID-19, 97 of these initial readings were changed to abnormal and two patients who had an initial finding of “possible pneumonia” were changed to “normal.”
Classification as normal or abnormal varied across the 11 radiologists who did the re-reads for this study. On the lower end, one participant classified 14% of CXRs as normal, while at the upper end another participant classified 86% of CXRs as normal. Most participants classified between 51% and 80% as normal.
Specific examples of CXR images are presented in Figures 3–6.
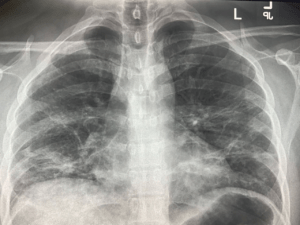
Figure 3. Multifocal mixed central and peripheral linear infiltrates extending out to lung periphery with superimposed ill-define patchy opacities at the bilateral lung bases. Lung apices spared. Overall low volume, study concerning for hypoventilation. (X-ray courtesy of Experity Teleradiology (www.experityhealth.com/teleradiology.)
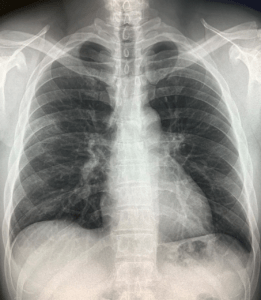
Figure 4. Subtle unilateral ground glass opacity at inferior margin of peripheral right upper lobe abutting the minor fissure. This patient has subtle unilateral involvement. (X-ray courtesy of Experity Teleradiology (www.experityhealth.com/teleradiology.)
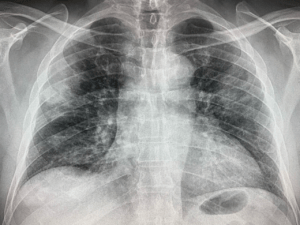
Figure 5. Severe bilateral involvement with ill-defined patchy consolidation at periphery of right upper lobe, ground glass opacity at peripheral left upper lobe and central infiltrates extending to the lung bases from the pulmonary hila. Small rounded patchy infiltrate also noted at right lung base. (X-ray courtesy of Experity Teleradiology (www.experityhealth.com/teleradiology.)
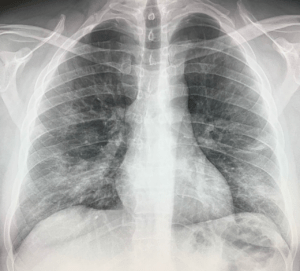
Figure 6. Hazy ill-defined opacity at lower aspect of right upper lobe as well as rounded patchy infiltrates in right lung base and periphery of left lung base. (X-ray courtesy of Experity Teleradiology (www.experityhealth.com/teleradiology.)
LIMITATIONS
Studies of this type are inherently limited due to their retrospective and observational nature. Additionally, only a single CXR series was obtained for each patient. Because patients presented at various phases of illness, it is impossible to know whether patients with normal CXRs at time of presentation developed radiographic findings later during their illness.
We did not have access to data regarding patients’ underlying health histories nor baseline CXRs, therefore it is unclear to what extent abnormalities identified may have reflected chronic pulmonary conditions. However, most patients (454, or 71.4%) were <60 years of age and healthy enough to present in an ambulatory care setting and, therefore, would be expected, with infrequent exception, to have normal baseline CXRs.
Regarding CXR interpretation, although the radiologists were instructed not to let the initial CXR read, or knowledge of COVID-19 diagnosis influence their interpretation, they were not blinded to this information and we cannot rule out that it might have had an impact on their classifications. The shift to classify more CXRs as abnormal during the re-read suggest that this might be so.
We also did not have any assessment of inter-rater reliability between radiologists on the re-reads. The difference in percentage of normal classification across participants suggests that clear individual differences do exist among radiologists. However, as our purpose was to show what findings would be reported for COVID-19 patients in a clinical setting, the variability in CXR classification serves to highlight the challenges in real-time assessment in such patients.
The initial CXRs were obtained at the clinical discretion of the treating provider. It is likely that variations in medical decision-making and CXR utilization among providers influenced the availability of CXRs available for analysis among patients confirmed to have COVID-19. The direction of any associated bias is difficult to predict because many factors (eg, number of patients waiting to be seen, patient expectations etc.) influence providers’ decisions about imaging in UC patients with respiratory complaints.
Finally, the radiologists re-read the available CXRs looking for known varieties of abnormalities. It is possible that there are indications of disease on CXRs related to COVID-19 that are not yet defined (as this is a novel illness) and, therefore, the radiologists might not be expected to identify them.
DISCUSSION
This report is the largest observational study to date examining plain film radiographic findings among patients with COVID-19 in an ambulatory care setting. The majority of COVID-19 patients who present in this setting show no identifiable abnormalities on standard CXR assessment.
Though chest CT has been shown to be more sensitive than CXR, CT is generally not available in ambulatory care settings. Additionally, after scanning a patient with suspected COVID-19, extensive cleaning and decontamination of a CT scanner is required, making routine use of CT is impractical. The CXR, on the other hand, is widely available assessment tool in UC centers and allows relatively rapid cleaning and turn-over between patients.
Recently thoracic imaging consensus guidelines in COVID-19 have been published by the Fleischner Society.9 In patients with mild clinical features, imaging is indicated after a positive viral test if the patient has risk factors for disease progression. In a patient with moderate to severe clinical features, imaging is indicated after a positive viral test if the patient is at risk for worsening of pulmonary status. If testing for COVID-19 is unavailable, imaging can determine if an alternative diagnosis is present (eg, lobar pneumonia) or, if findings suspicious for COVID-19 are revealed, can guide further workup.10
When present, the patterns of abnormal findings were similar to those reported in other series of hospitalized patients with COVID-193,8 with peripheral, multifocal, and lower lobe involvement and interstitial or ground glass appearance being the most common. Additionally, pleural effusions and lymphadenopathy were relatively rare findings, which is also consistent with existing studies of chest radiography in COVID-19 patients.8 Interestingly, alveolar disease was only bilateral in 133 (20.9%) of the total 636 CXRs, much less than reported in the CT literature where it is seen in 82% of cases.10 This may be due to the difficulty of perceiving early ground glass opacities on plain radiography and/or ambulatory patients presenting earlier in the course of illness.
In future reports we hope to examine what clinical signs, medical history, and demographic characteristic are associated with normal and abnormal CXR readings in patients with COVID-19.
CONCLUSION
CXRs obtained from confirmed and symptomatic patients with COVID-19 presenting to UC centers were normal in 58.3% of the patients, and normal or only mildly abnormal in 89% of patients. When abnormal, the most common findings involved the lower lobes and presented with an interstitial and/or multifocal pattern. Pleural effusions and lymphadenopathy were uncommon.
(This study was IRB approved and granted waiver of consent and full waiver of HIPAA authorization. No funding was obtained for this study.)
Acknowledgments:
The authors would like to acknowledge the following who donated their time and expertise to contribute to this paper:
Alyson Kendrick, QA Manager-TRS, Experity Teleradiology
B Ross MD, Radiologist
D Pellei MD, Radiologist
K Frame MD, Radiologist
C Chalfant MD, Radiologist
M Chalfant MD, Radiologist
M Donner MD, Radiologist
S Pawar MD, Radiologist
S Kathuria MD, Radiologist
M Hill MD, Radiologist
E Noeth MD, Radiologist
References
- Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. New Engl J Med. February 28, 2020. [Epub ahead of print]
- Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Inter Med. March 13, 2020. [Epub ahead of print]
- Wong HYF, Lam HYS, Fong AH-T et al. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. March 27, 2019. [Epub ahead of print]
- Xu X, Chengcheng Y, Jing Q, et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020;47:1275–1280.
- Ng MY, Lee EYP, Yang J, Yang J, et al. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol: Cardiothor Imag. org/10.1148/ryct.2020200034.
- Bernheim A, Mei X, Huang M, et al. ChestCT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. February 20, 2020. [Epub ahead of print]
- Trends in Urgent Care Radiology July 1, 2018 to June 30, 2019. Experity Urgent Care Quarterly. Issue 09; Winter 2020.
- Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425-434.
- Rubin GD, Ryerson CJ, Haramati LB, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Available at: https://pubs.rsna.org/doi/10.1148/radiol.2020201365. Published online April 7, 2020.
- Zhao W, Zhong Z, Xie X, et al. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. Am J Roentgenol. March 3, 2020. [Epub ahead of print]
Michael B. Weinstock, MD is Professor of Emergency Medicine, Adjunct, Department of Emergency Medicine, Wexner Medical Center at The Ohio State University; and Senior Editor, Clinical, JUCM. Ana Echenique MD DABR is Clinical Director, Quality Management, Experity Teleradiology. Joshua W. Russell, MD, MSc, FACEP is Supervising Physician, Legacy-GoHealth Urgent Care; Emergency Medicine Staff, PeaceHealth Health System; Associate Editor, Urgent Care RAP; and Editor-in-Chief, JUCM. Ari Leib, MD is Adjunct Clinical Assistant Professor Emergency Medicine Ohio University Heritage College of Osteopathic Medicine. Jordan Miller, DO is Junior Chief Emergency Medicine Resident. David J. Cohen, MD is Medical Director, Experity Teleradiology. Stephen Waite, MD is Clinical Associate Professor of Radiology, SUNY Downstate Medical Center, Brooklyn, NY. Allen Frye, NP is a clinician and research coordinator. Frank A. Illuzzi, MD, FACEP is Executive Vice President, Quality & Education, CityMD. The authors have no relevant financial relationships with any commercial interests.
(When referencing this article, please cite as follows: Weinstock MB, Echenique A, Russell JW, et al. Chest x-ray findings in 636 ambulatory patients with COVID-19 presenting to an urgent care center: a normal chest x-ray is no guarantee. J Urgent Care Med. 2020;14(7):13-18.
You can download a pdf of this article here

