Published on
Urgent message: Malignancies in children are often discovered only inadvertently, in conjunction with seemingly less dire presentations. Awareness of relevant signs and symptoms by the urgent care clinician can be invaluable in identifying tumors that might otherwise escape notice until they are at an advanced stage.
Muhammad Waseem, MD
Introduction
The identification of a palpable abdominal mass in an urgent care center or emergency department is quite concerning, as it represents a serious underlying disorder. Any abdominal mass in a child is usually considered malignant until proven otherwise. Abdominal tumors are uncommon in children and can present with pain, vomiting, or abdominals mass.
Here, we report on a child who presented with history of constipation and an abdominal mass that was identified on physical examination and subsequently diagnosed as neuroblastoma.
Case Study
A 15-month-old female presented with a two-day history of constipation. There was no vomiting, fever, or abdominal pain. She previously had been in good health and had seen her pediatrician regularly. Her parent also noted her to have a swollen abdomen, which they attributed to “constipation.” She had been evaluated for this by her pediatrician and was taking stool softeners.
Findings
Physical examination revealed a well-developed, comfortable child with:
- temperature 99°F (36.9°C)
- pulse 108 beats per min
- BP 99/62 mmHg
- respiration 20 per minute.
The patient’s abdomen was mildly distended, with fullness on the left side and flank. A somewhat firm, nontender, nonmobile mass with rounded margins was palpable in the left lower quadrant and left lumbar regions. No guarding, rigidity, or tenderness was noted. Bowel sounds were audible. Rectal examination revealed no tenderness or masses; rectal vault was empty. The remainder of the physical examination was unremarkable.
Other findings included:
- white blood cell count 9.3 x 103/mcL (11.1 x 109/L)
- 1% neutrophils
- 4% lymphocytes
- 7% monocytes
- 2% eosinophils
- 6% basophils
- hemoglobin 11.3 g/dL
- platelet count was 733 x 103/mcL (733 x 109/L)
- serum electrolytes were normal
- aspartate aminotransferase 43 U/L
- alanine aminotransferase 16 U/L
- albumin 3.8 g/dL
- bilirubin 0.3 mg/dL
- alkaline phosphatase 188 U/L
- lactic dehydrogenase 317 U/L (105-215).
- Uranalysis yielded normal findings.
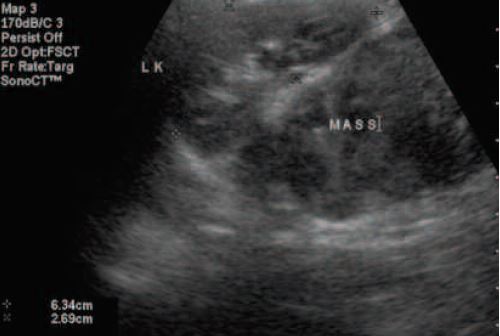
The initial renal ultrasound showed a retroperitoneal mass in the left flank without hydronephrosis or intrinsic renal mass (Figure 1). Subsequently, a contrast computed tomography (CT) scan of the abdomen revealed a left retroperitoneal mass between the left kidney and upper lumbar spine, with some displacement of the left kidney. (Figure 2). The urinary catecholamine metabolites, homovanillic acid (HVA), and vanillylmandelic acid (VMA) were also elevated.
The patient was referred to an affiliated tertiary care center for sub-specialty care.
Discussion
The child with an abdominal mass presents a unique challenge. A palpable mass in the abdomen of a child is a serious finding, with a fairly extensive differential diagnosis.
Abdominal masses may occur at any age, and may have a wide variety of clinical presentations. It is the urgent care clinician’s role to differentiate between benign conditions such as constipation and more serious causes of abdominal mass (Table 1).
When an abdominal mass is discovered on physical examination, the immediate goal is to determine its nature and extent. A tentative diagnosis can often be made from the presenting symptoms, age of the child, and the site of mass. Physical examination should focus on the location, size, and mobility of the mass, as well as other abnormalities on examination. The examination should also include measurement of serial blood pressures and a complete neurological assessment.
The presence of an abdominal mass may indicate the existence of colonic stools or tumors. In constipation, a mass can be palpated, which is usually associated with fecal impaction on rectal examination. Wilms’ tumor and neuroblastoma (NB) are the two common intra-abdominal masses in children. These are more prevalent in children younger than 4 years.
NB is the most common extracranial tumor in children,1accounting for 10% of pediatric malignancies. After tumors of the central nervous system, it is most common solid tumor in children.2 It is also the most common malignant tumor of infancy, with 50% of cases occurring in children younger than 2 years of age and 75% diagnosed by the fourth year of life.
The median age at diagnosis is 2 years, but the tumor may present in the neonate or even in adolescents and adults.3 NB occurs most commonly in the abdomen (65%), either in the sympathetic chain or more commonly in the adrenal gland.4,5 After the abdomen, the thorax is the second most common location of NB (15%) followed by the neck (1% to 5%) and the pelvis (2% to 3%).6
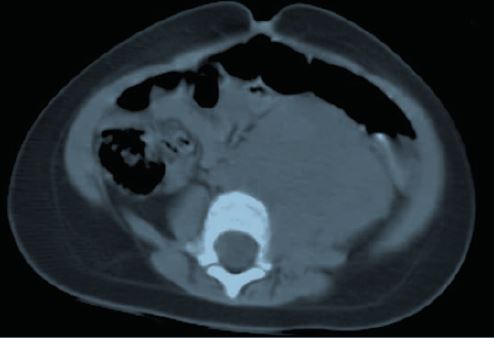
retroperitoneal mass between the left kidney and upper lumbar spine,
with some displacement of the left kidney
Table 1. Common Causes of Abdominal Mass in Children |
|
Clinical Presentation
NB may have diverse clinical features because of its variable sites of origin, propensity to metastasize, and secretion of hormones. Clinical features at presentation depend on the size and location of the primary tumor, and on whether the tumor has metastasized. Between 50% and 70% of patients with NB may have metastasis at the time of their presenation.7 Large masses may cause respiratory distress. The common sites for distant metastasis include the bone marrow, liver, and skin.8
The signs and symptoms of this tumor are dependent on the location of the primary tumor, which may occur anywhere along the peripheral sympathetic nervous system, and the sites of metastatic disease. Typically, the initial symptoms are nonspecific (general malaise, weight loss, unexplained fever), as in most patients the tumor is either retroperitoneal or in posterior mediastinum.9
Common symptoms
The common symptoms are:
- abdominal pain or discomfort
- sensation of fullness
- fever
- weight loss.
Although most children present with abdominal pain or a palpable mass, many present with manifestations of their metastatic disease, including bone or joint pain and periorbital ecchymosis.
Diagnostic Evaluation
An abdominal mass in a child must be considered malignant until proven otherwise. As such, any studies described here but not feasible for the urgent care setting should be facilitated via referral. They are included here for the sake of presenting as complete a picture of the diagnostic process as possible.
When an abdominal mass is detected in a child, imaging studies should be performed. Ultrasound is helpful in the initial evaluation of a child with an abdominal mass, as it is useful in determining the origin of the mass. It will also help determine whether the mass is cystic or solid.
Abdominal CT scan is a commonly used imaging modality for the assessment of a child with abdominal mass. It offers several advantages in the differential diagnosis of a possible Wilms’ tumor, such as confirmation of the intrarenal origin of the tumor, detection of multiple masses, determination of the extent of tumor, and evaluation of the opposite kidney.
Initial laboratory studies should include a complete blood count to identify anemia or thrombocytopenia suggestive of bone marrow invasion. NB produces catecholamine metabolites, which are used as tumor markers; therefore, a search for specific tumor markers secreted by the suspected tumor should also be made.
Elevation of urinary catecholamine metabolites, homovanillic acid (HVA), and vanillylmandelic acid (VMA) is used as a diagnostic screen,10,11 as this is present in 75% to 90% of patients with NB.12
Differential Diagnosis
Most abdominal masses in infants are due to problems of the urinary tract. Hydronephrosis and multicystic kidney are common causes of flank masses at this age.13 If a mass appears to be in the flank in an older infant or child, Wilms’ tumor and NB should be considered.
Additional features suggestive of Wilms’ tumor include fever, abdominal pain, or hematuria.
Hepatoblastoma is the most common primary hepatic tumor in young children. A high serum alphafetoprotein is often noted.
Lymphoproliferative conditions can also present with an abdominal mass. A suprapubic mass may be due to a distended bladder, which in turn may be secondary to urinary tract obstruction.
Conclusion
The presence of an abdominal mass in children includes a wide spectrum of diseases. This case emphasizes the value of performing a careful and thorough physical examination upon presentation. The presence of an abdominal mass should generate the suspicion for the possibility of tumor.
References
- Chandler JC, Gauderer MW. The neonate with an abdominal mass. Pediatr Clin North Am. 2004; 51: 979-997.
- Brodeur GM, Maris JM. NeuroblastomaIn: Pizzo PA, Poplack DG, eds. Principles and Practice of Pediatric Oncology. 4th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2002: 895-937.
- McLean TW, Iskandar SS, Shimada H, et al. Neuroblastoma in an adult. Urology. 2004; 64: 1232.
- Bousvaros A, Kirks DR, Grossman H. Imagining of neuroblastoma: A overview. Pediatr Radiol. 1986; 16: 89-106.
- Brouwers FM, Eisenhofer G, Lenders JW, et al. Emergencies caused by pheochromocytoma, neuroblastoma, or ganglioneuroma. Endocrinol Metab Clin North Am. 2006; 35: 699-724.
- Hiorns MP, Owens CM. Radiology if neuroblastoma in children. Eur Radiol. 2001; 11: 2071-2081.
- DuBois SG, Kalika Y, Lukens JN, et al. Metastatic sites in stage IV and IVS neuroblastoma correlate with age, tumor biology, and survival. J Pediatr Hematol Oncol. 1999; 21: 181-189.
- Castleberry RP. Biology and treatment of neuroblastoma. Pediatr Clin North Am. 1997; 44: 919-937.
- Kim S, Chung DH. Pediatric solid malignancies: Neuroblastoma and Wilms’ tumor. SUrg Clin North Am. 2006; 86: 469-487.
- Laug WE, Siegel SE, Shaw KN, et al. Initial urinary catecholamine metabolite concentrations and prognosis in neuroblastoma. Pediatrics. 1978; 62: 77-83.
- Shaw PH, Dickman PS. Neuroblastoma mimicking rhabdoif tumor of the kidney. J Pediatr Hematol Oncol. 2003; 25: 572-574.
- Weinstein JL, Katzenstein HM, Cohn SL. Advances in the diagnosis and treatment of neuroblastoma. Oncologist. 2003; 8: 278-292.
- Chandler JC, Gauderer MW. The neonate with an abdominal mass. Pediatr Clin North Am. 2004; 51: 979-997.
