Urgent message: Though not considered as at “at risk” for severe disease with COVID-19, children have suffered significant disruptions to educational and personal activities throughout the pandemic. Recognizing urgent care’s role in testing for the virus could show benefit for families and urgent care centers alike.
Rita P. Nunag, MD; Francesca M. Darquea, MD; Claire Loiselle; and Magdy W. Attia, MD
Citation: Nunag RP, Darquea FM, Loiselle C, Attia MW. COVID-19 testing pattern in a suburban pediatric urgent care center. J Urgent Care Med. 2021;16(3):39-43.
ABSTRACT
Background and Objectives
The COVID-19 pandemic disrupted educational, social, and recreational activities for children. Widespread testing became a primary strategy to limit spread. Pediatric urgent care centers (PUCCs) were at the forefront of performing these tests. We aimed to describe the pattern of testing in the PUCC population and summarize differences between symptomatic and asymptomatic in exposed and nonexposed patients who tested positive and negative for COVID-19.
Methods
This was an IRB-exempt retrospective study of patients who underwent PCR COVID-19 testing between March 28, 2020 and January 31, 2021 at a suburban PUCC. All patients presenting to the PUCC underwent a “COVID screen” using a CDC screening tool for symptoms. All patients were able to obtain a COVID-19 molecular RT-PCR test regardless of the COVID-screen designation. Demographics, reason(s) for testing, exposure source, type and duration of symptoms, and test results were obtained. Patients were stratified as symptomatic or asymptomatic, with or without exposure, and compared based on their COVID-19 test results. Data were analyzed using descriptive statistics and appropriate test for statistical significance.
Results
During the study period, 1,087 COVID-19 tests were obtained. The study population was 48.9% male, 81.8% Caucasian, 7.6% Black, and 3.4% Asian; 4.9% were Hispanic or Latinx. The mean age was 8.8 (SD±5.8) years. Of the 1,087 patients tested for COVID-19 during the study, 10.5% were positive. The demographics of the positive group did not differ significantly from the study population except for age (mean 11.3; SD±5.8 years; P<.0001). Of 55.1% symptomatic patients, 12.8% tested positive compared with the asymptomatic group (44.9%), where only 7.6% tested positive; P<.005. Of the study sample, 48.9% reported exposure and were more likely to test positive: 16.9% compared with nonexposed, 4.3%; P<.0001. Exposures within the household accounted for 27.4%, of whom 35.6% tested positive, 44.6% were symptomatic, and 28.4% were asymptomatic. Of those reporting exposures but who were asymptomatic, only 9.9% were positive; P<.0001. Of asymptomatic patients with no known exposure, only 0.8% were positive. Although there was a significantly higher rate of positive tests in symptomatic patients, only loss of taste/smell was significant (18 patients with 12 positive; P<.0001). The remainder of known COVID-19 symptoms were not singularly associated with a positive test.
Conclusions
In our cohort, most COVID-19–positive patients had a known exposure. Symptomatic patients with a known exposure were more likely to be positive than symptomatic patients without an exposure. Symptomatic household contacts were the most common and associated with the highest rate of positive test. The lowest positivity rate was in asymptomatic patients without exposure. Loss of taste or smell was not a common symptom but was highly associated with testing positive. All other remaining COVID-19 symptoms alone were not significantly associated with a positive test. This data may guide testing and isolation recommendations in low-resourced areas.
INTRODUCTION
On March 11, 2020, the World Health Organization declared the COVID-19 outbreak a global pandemic, recognizing that the rapid spread of the virus and severity of illness associated with the SARS-CoV-2 infection had created a public health crisis. Educational, social, and recreational activities for children were disrupted due to pandemic regulations imposed by various public health officials. Widespread testing became a primary strategy in identifying COVID-positive patients for isolation and contact tracing to contain the spread of the disease as well as to assess community burden of the infection.
Pediatric urgent care centers (PUCCs) were at the forefront of performing these tests in children. Patients and their families were advised by healthcare providers to follow recommendations for quarantine and isolation from the Centers for Disease Control and Prevention, which often extended beyond reporting of test results. Understanding the patterns of test results in symptomatic and asymptomatic patients in those with and without an exposure to an index case, as well as clinical features of those who tested positive vs those who tested negative, may prove valuable in establishing more efficient testing, quarantine, and isolation recommendations to providers in similar or, more likely, lower-resourced clinical settings.
The aim of this report is to describe patterns of COVID-19 testing in a suburban PUCC and to summarize test results in symptomatic and asymptomatic patients with or without exposure to index cases for the purpose of risk stratifying potentially positive patients.
Methods
This is an IRB-exempt retrospective cohort study of pediatric patients who underwent PCR COVID-19 testing between March 28, 2020 and January 31, 2021 at a suburban PUCC in Pennsylvania. All patients presenting to the PUCC underwent a “COVID screen,” incorporating CDC screening question guidelines: fever >100.4°F (38°C) in the past 72 hours; cough; shortness of breath; rhinorrhea; sore throat; gastrointestinal symptoms including nausea, vomiting, diarrhea, or abdominal pain; or exposure to a suspected or confirmed COVID-19 case within the last 14 days. Any single positive reply was viewed as a positive screen. Exposure was based on a patient/parent report and may not have met the CDC standard of within 6 feet for at least 15 minutes. All patients were able to obtain a COVID-19 test if clinically indicated or upon request, regardless of the COVID-screen result.
Initially, patients were stratified as symptomatic or asymptomatic. Symptomatic patients were evaluated in the traditional patient-room manner. Asymptomatic (absence of fever, cough, rhinorrhea, sore throat, gastrointestinal symptoms) patients, with or without known COVID-19 exposure, were given the option of mobile evaluation and testing. The initial database of patients tested for COVID-19 contained unique identifiers, test dates, and test results. All COVID-19 samples were obtained by nasopharyngeal swab and performed as molecular RT-PCR at commercial labs. Results were usually obtained 48 to 72 hours after the PUCC visit. All patients were advised to quarantine pending results of the COVID-19 test, and to follow CDC quarantine guidelines postexposure, if applicable. A retrospective chart review was performed to describe this population and included demographics, reason(s) for testing, whether there was a known or presumed exposure, and nature of that exposure.
Data were stored electronically on a password-secured drive. All patient identifiers were removed and study subjects were given identification numbers. After compiling a complete data set, we performed statistical analyses. The dependent variable was the PCR COVID-19 test result. Subset analyses included comparison of demographics and clinical features associated with positive tests in those who were symptomatic vs asymptomatic, with and without known exposure. We summarized data as ratios and means/standard deviations (SD), and used appropriate statistical analyses based on the nature of variables: Chi square for dichotomous variables and comparison of means for continuous variables.
RESULTS
Study Population
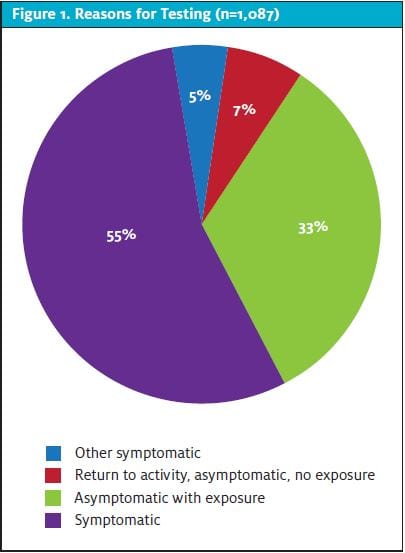
During the study period, 1,087 COVID-19 PCR tests were obtained during 1,087 unique patient visits to our PUCC. The study population was 48.9% male. Of patients, 81.8% identified as Caucasian, 7.6% Black, and 3.4% Asian. Of these, 4.9% were Hispanic or Latinx. The mean age was 8.8 (SD±5.8) years. Of all patients, 60.7% were evaluated in the traditional patient-room setting; 39.3% of patients presented for the sole purpose of receiving a COVID-19 test and chose the mobile-testing model where history, vital signs, and a limited physical examination were performed while the child was in the family vehicle. Reasons for testing are shown in Figure 1.
Of the 1,087 patients tested for COVID-19 during the study period, 114 (10.5%) were positive. The demographics of the positive group did not differ significantly from the study population except for older age (mean 11.3 years; SD±5.8 years; P<.0001).
Test Results in Symptomatic and Exposed Patients
A total of 599 (55.1%) patients presented with symptoms that could be attributed to COVID-19 based on the evolving CDC criteria, while 488 (44.9%) were asymptomatic. Of all patients tested, 532 (48.9%) reported a COVID-19 exposure; of those, 170 (32.0%) were symptomatic. Of the symptomatic patients who were tested, 77 (12.9%) tested positive, compared with 37 (7.6%) from the asymptomatic group; P<.005. These 77 symptomatic patients accounted for 67.5% of all positive cases. Ninety (16.9%) patients who reported exposure tested positive, vs 24 (4.3%) patients without exposure; P<.0001. These 90 patients accounted for 78.9% of all positive cases (Figure 2).
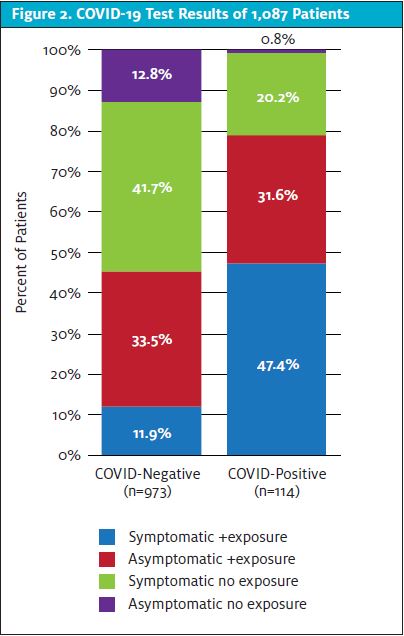
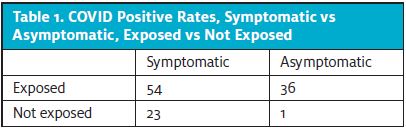
Of asymptomatic patients with exposure (n=362) at the time of testing, 36 (9.9%) were positive; P<.0001. Fifty-four of 170 (31.8%) patients who reported symptoms and an exposure were positive; P<.0001. (See Table 1.) Only one asymptomatic patient of 126 (0.8%) with no known exposure was positive (Figure 2).
Of exposures, 146 (27.4%) were within the household and 52 (35.6%) tested COVID-19 positive; 65 (44.6%) were symptomatic. More specifically, 29 (44.6%) symptomatic patients with known household exposure tested positive for COVID-19, and 23 (28.4%) asymptomatic patients with household exposure tested positive; P=.042.
Fifteen of 87 (17.2%) patients who reported an exposure in a social setting were positive, six of 76 (7.9%) who reported a school/work/daycare exposure were positive, seven of 37 (18.9%) who reported a sports exposure were positive, and 10 of 186 (5.4%) who reported an unspecified exposure were positive.
Symptom data
Although there was a significantly higher rate of positive tests in symptomatic patients, only loss of taste or smell was a symptom significantly associated with COVID-19 infection. Twelve of the 18 (66.7%) patients who reported loss of taste or smell were COVID-positive; P<.0001. Of these 18 patients, only two reported a known COVID exposure, and both tested positive. Of note, the mean age of patients complaining of loss of taste or smell was 15 years (SD±3.7 years).
Symptomatic patients included in this cohort had at least one or more of these symptoms reported but none was singularly associated with a positive COVID-19 test: fever prior to arrival at the PUCC, P=.318; fever present during visit, P=.365; cough or shortness of breath, P=.594; congestion or rhinorrhea, P=.628; sore throat, P=.564; or gastrointestinal symptoms, P=.056.
DISCUSSION
Our report describes a population of children presenting to a PUCC and who were symptomatic or asymptomatic, with and without exposure to a COVID-19 index case. Testing availability was limited at the onset of the pandemic and in the early weeks of our study, similar to other PUCCs surveyed at the time.1 Once the supply chain was established, testing protocols were no longer restricted, and our data were reviewed periodically to quantify community demand for COVID-19 testing, test supply availability, and to identify patterns of infection.
As a PUCC, our families were subject to the terms of their insurance regarding urgent care payment, although there was no charge for the test itself. Only PCR testing was performed in our PUCC; therefore, families seeking “rapid antigen testing” or those with financial barriers were not part of our study population. While age restrictions may have posed a barrier for testing at other testing facilities during the peak of our study, we found that our positivity rate was similar to the overall prevalence of positive tests in the community at the time.2
Of our COVID-19-positive cohort, 78.9% reported an exposure. Transmission rates have been reported as highest in household settings,3,4 and our study concurs with those reports. A study in Spain suggested overall household transmission rates of 31% to 37%, and 10% to 14% for social exposures,3 which closely matches our data of 35.6% positive among household exposures and 17.2% among social exposures. However, another meta-analysis found the household transmission rate to be 16.9%, with transmission to children lower than to adults (17% vs 28%, respectively).4
These findings should be interpreted with the understanding that lockdown measures may have limited exposure beyond the household during the timeframe of our study. Additionally, our asymptomatic patients were encouraged but not required to defer testing for at least 48 hours after a known exposure. Our study may have been impacted by a shorter incubation period prior to testing, as well as ample access to testing in the community.
A study published early in the pandemic using a mathematical model based on global data determined symptomatic COVID-19 infection in children to be approximately 20%.5 A separate pediatric urgent care study reported symptomatic rates of 52% in their COVID-positive patients,6 closer to our findings of a 67.5% symptomatic COVID-positive rate. This disparity of symptom frequency in pediatric COVID patients may be unique to utilization of urgent care and accessibility of testing in our geographical area. However, transmission via asymptomatic cases poses an ongoing concern,7,8 and PUCCs can be a valuable resource for accurate COVID testing where available.
One study suggested mobile testing sites were frequently utilized for testing of young adult employees for return to work,9 but did not note reasons for pediatric testing, beyond referral by primary care offices. Our study indicates 7% of our tests were done solely for clearance to participate in an activity, whether school, sport, or work, without symptoms or exposure. We suggest this represents a significant cost and emotional burden to families and children attempting to maintain activities for healthy, low-risk children amid the pandemic restrictions. Overall, slightly less than 1% of asymptomatic patients without exposure tested positive for COVID-19.
CONCLUSION
In our PUCC cohort of 1,087 patients, 55.1% were symptomatic, 48.9% reported a COVID-19 exposure, and 10.5% were COVID-19 PCR positive. Of COVID-positive patients, 78.9% had a known exposure and 67.5% were symptomatic. Of tests requested, 6.8% were by patients without symptoms or known exposure for the purpose of returning to or to participate in an activity, work, school, daycare, or sports.Patients who were symptomatic with a known exposure were more likely to be positive than symptomatic patients without an exposure. Household contact was the most frequently reported exposure and was associated with the highest rate of positive tests, more so if the patient was symptomatic. The lowest positivity rate was in asymptomatic patients without exposure. Loss of taste or smell was not a common symptom but was highly associated with testing positive for COVID-19. All remaining COVID-19 symptoms alone were not significantly associated with a positive test.
These data may help to risk-stratify patients’ pretest probability from birth to 20 years old regarding likelihood of positive COVID-19 status and guide testing indications and isolation recommendations pending test results, especially in low-resourced areas.
REFERENCES
- Hsiang W, Forman H, Jain S, et al. COVID-19 testing capabilities at urgent care centers in states with greatest disease burden. F1000Res. 2020;9:328.
- Covid Act Now. Delaware County, PA. Available at: https://covidactnow.org/us/pennsylvania-pa/county/delaware_county/?s=1933851. Accessed June 10, 2021.
- Pollán M, Pérez-Gómez B, Pastor-Barriuso R, et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet. 2020;396(10250):535-544.
- Madewell ZJ, Yang Y, Longini IM Jr, et al. Household transmission of SARS-CoV-2: a systematic review and meta-analysis. JAMA Netw Open. 2020;3(12):e2031756.
- Davies NG, Klepac P, Liu Y, et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020;26(8):1205-1211.
- Miao K, Illuzzi F, Hwang AC. High prevalence of asymptomatic COVID-19 in the pediatric population. J Urgent Care Med. 2020;15(1):21-23.
- Furukawa NW, Brooks JT, Sobel J. Evidence supporting transmission of severe acute respiratory syndrome coronavirus 2 while presymptomatic or asymptomatic. Emerg Infect Dis. 2020;26(7):e201595.
- Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970-971.
- Flynn EF, Kuhn E, Shaik M, et al. Drive-through COVID-19 testing during the 2020 pandemic: a safe, efficient, and scalable model for pediatric patients and health care workers. Acad Pediatr. 2020;20(6):753-755.
Author affiliations: Rita P. Nunag, MD, Nemours Children’s Hospital, Delaware, Wilmington DE; PM Pediatrics, Wayne, PA. Francesca M. Darquea, MD, Nemours Children’s Hospital; Tricounty Pediatrics, Abington, PA. Claire Loiselle, Nemours Children’s Hospital. Magdy W. Attia, MD, Nemours Children’s Hospital; Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA. The authors have no relevant financial relationships with any commercial interests.
