Urgent message: Part 1 of this article, in the June issue, looked at initial considerations for enhancing urgent care profitability by providing physical therapy services. In Part 2, the authors address tactical considerations, from revenue to staffing models.
LAUREL STOIMENOFF, PT and HILARY HELLMAN, SLP
Babe Ruth said, “Yesterday’s home runs don’t win today’s games.” Consumers have gravitated to on-demand medical services and the market has responded. Urgent care centers now face competition, not only from new urgent care sites but also other on-demand services such as telemedicine, freestanding emergency rooms, primary care physicians extending hours and accepting walk-ins, and retail hot-model clinics. Without some innovation and new home runs in its arsenal, urgent care’s market share has the potential to erode.
In Part I of this article, we addressed the natural synergies between the urgent care scope of care and physical therapy. In most injuries, early therapy intervention expedites healing and returns the patient to prior levels of function faster. We therefore suggested that urgent care centers either have a referral relationship with a local therapy provider who can provide same- or next- day appointments or consider establishing a physical therapy department to support the urgent care clientele. Adding this service not only distinguishes your urgent care from the competitors but can also enhance the patient experience through the convenience of a single destination for initial and follow-up care and improved clinical outcomes.
Part II of this article addresses tactical considerations associated with implementing physical therapy in an urgent care practice and transforming this new service line into a profitable service valued by patients and the community.
Making the Decision to Implement Therapy Services
Determining the need for and viability of physical therapy within an urgent care center is fairly simple. A Service Line Needs Assessment can be performed in less than 60 days by evaluating the center’s demographics, patient diagnoses at time of service, and the likelihood that the current patient population would benefit from therapy intervention. Patients who are motivated to return to their preinjury or illness activity quickly tend to be a favorable demo- graphic. This can be a geriatric tennis player or a high school athlete who value interventions that are likely to accelerate the healing process. In addition, any patients who have limitations in strength and mobility secondary to trauma are obvious candidates but the assessor should not overlook patients with safety issues (fall risks), gait anomalies, balance/vestibular disorders, acute or chronic pain, incontinence, edema and hyper- or hypomobility in joints because they are also potential candidates who would benefit from on-site, skilled therapy services.
Patients are most likely to seek therapy close to home because it typically involves multiple visits. There are financial considerations because most commercial and public insurance plans require copayments or deductibles, resulting in out-of-pocket expense for patients at each and every visit. These costs may be perceived as prohibitive. Some patient choices may be limited because their insurance carrier has restricted contracts for in-network care. Patients seeking services covered by Workers Compensation have a higher likelihood of attending and completing a therapy prescription because these visit types are considered conservative treatment (as opposed to surgery) and the services are covered with no out-of- pocket obligation by the patient once medical necessity is established and authorization is secured. Injured workers are also often compensated for any lost time from work to attend medical and therapy care and may consider completing all authorized therapy as a “right.”
In Part I, we represented that 10 to 12 new patients in a physical therapy department per week will typically create a patient load for one full-time therapist of approximately 12 to 14 patients per day. Lower volumes may require creativity, such as part-time availability (for example, Monday/Wednesday/Friday Services), establishing a therapy service site supporting multiple urgent care centers, or continuing to outsource therapy services to responsive community-based therapy practices.
The Pro Forma
Once you confirm that patient demand will support a full- or part-time physical therapy practice via your urgent care clinic’s Service Line Needs Assessment, you should create a financial pro forma. An urgent care pro forma can assume approximately $40,000 to $50,000 in start-up capital used principally for furniture, fixtures and equipment (FFE). The pro forma should also assume initial staffing of 2.0 FTEs, including a physical therapist, a part-time physical therapy aide and part-time front office support.
Assuming the physical therapy space is contiguous to the physician space, the front desk staff for the physician services could also be responsible for physical therapy scheduling, authorizations, insurance verification, daily statistics, and time-of-service collections. Just as in urgent care practice, additional success factors included in the analysis should be the anticipated:
- # of therapy referrals/week
- # of therapy visits/day
- # of visits/referral
- Net revenue/ visit (NRPV)
- Revenue/cost per episode of care
Typical payment formats for NRPV include global rates or fee for service. Global rates often account for the additional time involved in the therapist’s initial evaluation and the creation of the plan of care.
Expenses are relatively low in the physical therapy practice when compared to the urgent care or other specialty services. They are heavily weighted toward the costs of human resources associated with staffing the site. Therefore, tracking labor cost per visit against your pro forma will be an important operations activity once implemented. The pro forma should assume one therapist caring for 12 to 14 patients per 8-hour day depending on acuity and support.
While profit margin in a typical physical therapy practice can be 15% go 20% of net revenue, the service line can also bring additional opportunities to an urgent care center by increasing credibility for your services with employers through extended occupational medical services and capturing word-of-mouth repeat business as a more comprehensive provider of choice for on- demand medical services. The physical therapy department can also support marketing and community out reach activities with schools, sporting events, and employer services.
Self-Pay and Out-of-Pocket Considerations
The 2012 UCA benchmarking survey provided the payor distribution of urgent care survey respondents. It represented that 12% of the participating urgent care clinic’s revenue was “self-pay.” This supports the need to implement a payment plan that extends to therapy services. Many urgent care clinics offer a medical discount plan and should consider adding therapy services to the plan agreement with patients. Just as a medical discount program can be heavily marketed as a patient loyalty program, so can a cash pay program for physical therapy services. Because physical therapy is a service that typically requires return visits over time to achieve therapy goals, policies related to handling self-pay or patient responsibilities must be determined and communicated in writing and up front.
The Physical Plant—Creating an Appealing Environment
The physical environment of the physical therapy clinic is a key component tied to staff efficiency as well as the likelihood that patients will complete their prescribed course of therapy and/or achieve the goals of care. Patients have a choice about where to seek care and whether to return for ongoing care. Operators need to create an environment that makes patients want to choose your physical therapy services over others and complete their course of treatment once started. One owner indicated that he placed a glass wall between his practice, including the reception area, and the physical therapy gym. Patients receiving care could see the new equipment and professional staff working with the patients one-on-one, and therefore selected his clinic over others.
Physical therapy services typically require use of one to two private rooms or curtained areas for patient evaluations and administration of some care and therapy modalities where patient privacy or modesty must be respected. The majority of therapy services, how- ever, take place in an open area that includes exercise equipment and supports active patient participation in the plan of care. This area is the “hub” and should be a professional one, but also upbeat. Patients socialize with one another and there is often a flat screen television with sports or other universally appealing content or videos. It should be immaculately clean and uncluttered with the feel of an upscale health club. Staffing and scheduling must support an environment where patients can be closely monitored and receive frequent cues and therapist involvement at every visit. Positive therapist and staff interactions with patients combined with an inviting physical plant are essential components to fostering patient loyalty and a desire to return for care. Include physical therapy services in not only your overall assessment of quality and clinical outcomes, but also patient satisfaction monitors and action plans.
Space.
The space determination will be dependent upon the number of new referrals seen each week.
Presuming each therapist will see about 10 to 12 patients per day, space needs can be less than 800 square feet to start. Assuming the practice will grow, an urgent care operator might consider seeking a first right of refusal for contiguous space if it is available. Extended hours more aligned with the urgent care schedule may also be a consideration versus adding space when limitations become problematic.
When possible it is preferable to have physical therapy located on the first floor with natural light and easy access to parking. Open area is most desirable for the physical therapy space and a clear line of sight for the therapist to all areas of the gym is preferred, especially if aides/techs and support staff are potentially going to be supporting patient care.
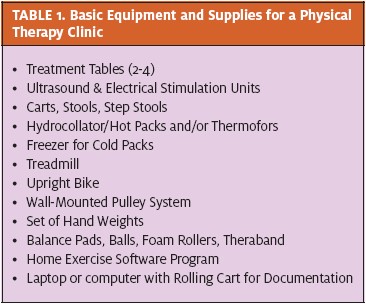
Therapy Equipment.
The equipment for a 1- to 2-therapist urgent care clinic is relatively inexpensive and will depend upon space, the number of patients expected, and the types of diagnoses to be seen. Physical Therapy Centers typically open with the basics and add equipment, services and supplies as the program grows and the needs of the patients and practice scope are better understood. Incorporation of items patients can use as part of their home exercise and post-discharge programs is essential. These items include therapy balls/bands, foam rolls and supplies.
Recruiting and Staffing
The therapy program will begin with one physical therapist and 0.5 to 1.0 aide/technician, assuming the existing urgent care front office staff has the ability to support the administrative and intake functions. If the existing front office is already at capacity, a 20- to 25- hour-per-week support person should be considered.
It is important to recruit a therapist who fits well into the culture of your practice, is well-experienced, skilled in treating the population you serve, and capable of being self-directed When recruiting a physical therapist you will want to include a description of the position, skills needed, and education and experience required. Because the therapist will be working independently and likely to be supervising some support staff, a therapist with experience in an outpatient setting would be more likely to flourish from the start. As with any hire, references will also be important to check prior to employment including not only clinical expertise but also service orientation, flexibility, initiative and patient interaction skills. Physical therapists typically have many career opportunities due to a national shortage of active licensees. Employers should consider differentiating the recruitment message including opportunities for job sharing and scheduling flexibility.
Operational Steps to Success
The business success of adding physical therapy is in the operational details. To provide the best care with the best clinical results, at the highest levels of patient satisfaction and greatest profitability, the workflow and processes must be focused on the patient experience and must efficiently eliminate any unnecessary time and steps so the flow is seamless.
The physical therapy patient process begins with the referral and ends with final payment with recommended processes as described below.
Referral.
The referral is received at the front desk in person, via the practice management system, email, fax or phone. Once received, the order drives the patient appointment schedule for the initial evaluation. Best-in- class therapy providers contact patients <24 hours to schedule the initial evaluation appointment and ensure patients are seen within 48 to 72 hours of the referral. Some patients may need to be seen or prefer to be seen on the same day as the referral. Data support that early therapy intervention results in faster recovery and reduced lost work time. Therefore, processes that support same-day access must be set up within the center. Patients who are not seen within 24 to 72 hours of their physician visit have a higher incidence of cancellations/no-show rates and tend to either find another provider or another avenue for care.
Authorization.
Obtain the current insurance information from the patient and verify the insurance benefit for therapy, co-pay, coinsurance and any preauthorization requirements. This information can be obtained online or by phone. For financial transparency, we suggest determining if an authorization is needed prior to seeing the patient to ensure services will be paid by payers. Some payors will allow the first-visit evaluation without an authorization but will require an authorization for subsequent visits while others will allow a set number of visits without authorization. A cash-pay price should also be available at a discounted rate when paid at the time of service or included in your urgent care medical discount plan when available. Efforts should be made to ensure the patient will be “in-net- work” based on contracts as multiple visits because an out-of-network provider can place a substantial financial burden on the patient. If physical therapy services are out-of-network, all efforts should be made to refer the patient to a convenient and capable in-network therapy provider.
Scheduling.
The scheduling methodology is very important and is different for physical therapy than for an urgent care practice. Physical therapy appointments are scheduled for 30 to 60 minutes and are for multiple visits over the course of 4 to 6 weeks depending on diagnosis, severity, financial coverage, and access. The front desk plays an important role in ensuring that the schedules are full and that there are adequate evaluations (10 or more) per week/per therapist. We recommend scheduling evaluations for 60 minutes that will also include initiating therapy and a home program when appropriate. Follow-up visits are generally scheduled on the half hour but extend for 45 to 60 minutes.
The benchmark for cancellations/no-shows is 10% or less. Every referred patient who is not ultimately seen results in an average revenue foregone of $600 to$1,000. Every patient who self-discharges because he or she cannot get an appointment at the desired time or does not see the value in continuing also results in a lost revenue opportunity. Scheduling personnel should notify the treating therapist when unable to meet a patient’s scheduling needs or when patients fail to schedule ongoing care prior to goals being met.
Access.
Employed patients do not want to miss work and will usually request an appointment either before or after work, whereas Workers Compensation patients are typically less concerned because lost work time is likely to be compensated (although employers appreciate before or after shift access). When assessing access it is important to differentiate between any open appointment time and the first available of a preferred A.M./P.M. slot. It is also important to be sure the scheduled hours meet the needs of the patients and not just the convenience of the therapist or staff. Following the evaluation, the patient will frequently be scheduled for 4 to 6 follow-up visits. When possible it is preferable to provide continuity and have one therapist see the patient throughout the entire course of care.
No-Show/Cancellation Policy.
A clearly defined no- show/cancellation policy is important and should be included in the initial paperwork requiring a patient signature acknowledging that he or she has read and understands the policy. If a patient no-shows for an appointment there is a good chance that he or she is self-discharging and not likely to keep future appointments. We recommend that a patient be called for any missed appointment and be called 24 hours before the next appointment to confirm attendance. If a patient does not return the call and confirm that he or she will be attending the next appointment, the front desk staff can open the slot for another patient. A no-show/same- day cancellation rate of greater than 10% has a significant impact on the productivity and profitability of a program. Discussions regarding attendance are best conducted between the therapist and the patient during the initial evaluation process because patient function and clinical outcomes are dependent on fulfilling the plan of care.
Billing/Coding.
The billing system used for your urgent care practice may be able to accommodate billing for physical therapy, but there are nuances and requirements specific to therapy visits. Many choose to out- source billing to an entity familiar with the specific rules, regulations, codes and modifiers used for therapy. It is recommended that training be provided to therapy providers and billing staff to ensure the payor rules are understood and followed. Many systems now integrate the billing and documentation so these functions are integrated. An audit system is recommended to ensure that the billing is accurate, is supported by the documentation, demonstrates skilled care and captures all of the appropriate charges.
Medicare (CMS) and many other payors continue to modify the billing/coding requirements and it is important to have the most current information at all times. As an example, CMS is currently piloting a Claims Based Outcomes Reporting (CBOR) program whereby, effective July 1st, specific “G” codes must be submitted at select intervals in order to convey patient progress toward therapy goals. Contracts and payor communications should be reviewed regularly and your therapy and billing staff should have an understanding of each payor’s requirements and their method of payment (CPT code, visit, episode of care). Your lead therapist(s) should also be providing input on payment processes and ultimately bearing responsibility for ensuring prompt payment when appropriate therapy services have been rendered.
It will be important to set processes in place for billing, collections, payment posting, denial management and education to achieve desired results.
Front Desk and Patient Arrival.
The front desk employ- ees are the first point of patient contact and their initial interaction sets the tone for the patient experience in physical therapy. It is important to provide education, training, and scripting for the front desk staff to ensure the best patient experience. Because initial evaluations are often scheduled in advance, insurance information should be verified and paperwork completed prior to beginning the therapy evaluation.
As in the urgent care setting, collecting the copay prior to the visit and setting a standard expectation that 100% of the copay will be collected daily by the front desk staff reduces costly collections issues on the back end. A close working relationship between the therapist and front desk staff ensures the most efficient processes.
Patient Visit.
The patient evaluation will be approximately 60 minutes and during that time, the therapist will complete the evaluation, develop a plan of care including the patient’s goals, begin treatment and most often provide the patient with a home program of exercises he or she is to do between the evaluation and next visit. During this visit the therapist will begin to plan for discharge and will involve the patient in determining the frequency and duration of care, including consideration of scheduling and financial responsibility. Follow- up sessions will be from 45 to 60 minutes with most courses of care being 10 visits or less.
Documentation.
The therapist will be responsible for documenting the visit in accordance with all professional, ethical, practice act and payor rules and regulations. The initial plan of care must be signed by the physician if required by the payor (CMS) and/or if the recommended plan of care is different than the initial physician order. Orders are often “evaluate and treat,” which provides the therapist the freedom to establish a plan of care consistent with the evaluation and established goals.
The documentation must support the need for skilled care and must support the charges billed. While services are warranted to improve the health and function of the patient based on diagnosis and presentation, a failure to document the need for the therapist’s skills has the potential to result in payment denials.
It is important to use a documentation system that is easy to navigate and does not take unnecessary time from the patient care. It will be important to evaluate whether or not the urgent care system will meet the needs of the physical therapy program or if alternatives will need to be considered including written documentation, dictation or a therapy-specific electronic health record system.
Conclusion
Physical therapy services typically complement the urgent care scope of care. Implementing physical ther- apy services as an adjunct to an urgent care practice requires an initial service line needs assessment, plan- ning, ongoing key performance indicator measurement, clinical quality oversight. and performance improve- ment. Successful implementation can provide a valued service to patients and a profitable service line for an urgent care center owner.
Babe Ruth knew that yesterday’s home runs would- n’t win today’s games and baseball wasn’t experiencing the tumultuous changes taking place in today’s health- care environment. The rules of baseball are relatively constant while the rules of healthcare delivery are being written and revised by the minute. Therapy services provide a conservative treatment solution supportive of today’s accountable care objective to secure the greatest health outcome at the lowest cost in a more holistic environment. Physical therapy complements the urgent care scope while also aligning with the future healthcare environment focused on outcomes, quality and wellness. The influence of new competition and price pressure coupled with an aging population, healthcare reform, and the potential for newly insured entering the market collectively support the implementation of a physical therapy service line. A well- planned and executed strategy will allow you to hit this one out of the park.
Read Part I: Creating Value By Adding Physical Therapy to Urgent Care – Part 1: Initial Considerations & Rationale

