David Hourani, MD; Bradley M. Golden, DO; Daniel McCollum, MD; John R. Barrett, MD
Urgent Message: Mistaking traumatic facial paralysis for Bell’s palsy can delay treatment and have lifelong consequences. Prompt imaging and otolaryngology consultation are critical in determining disposition and management.
Citation: Hourani D, Golden BM, McCollum D, Barrett JR. Delayed-Onset Facial Nerve Palsy Following Post-Auricular Gunshot Wound: A Case Report. J Urgent Care Med. 2024; 18(x):13-16.
Keywords: facial nerve palsy; cranial nerve VII palsy; temporal bone trauma; temporal bone fracture; facial; nerve; palsy
Abstract
Introduction: Facial nerve palsy is a common presentation to emergency departments (ED) or urgent care (UC) facilities.
Clinical Presentation: A 29-year-old male presented to the ED with right-sided facial droop for 2 days. Nine days prior to presentation, he had been seen in the ED after a post-auricular gunshot wound (GSW) with injury to the superficial auricular and post-auricular area. Non-contrast head computed tomography (CT) at that time demonstrated diastatic temporal bone fractures but was otherwise unremarkable.
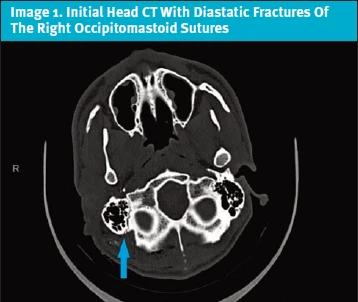
Physical Exam: On his second presentation, his exam was significant for complete right forehead and perioral paralysis but with preserved closure of the eye. A repeat head CT with and without contrast was obtained, which showed a new mastoid effusion in comparison with his CT from 9 days prior.
Case Resolution: Otolaryngology (ENT) was consulted, and the on-call ENT physician performed bedside incision and drainage. The patient was discharged home with 2-day otolaryngology clinic follow-up, oral and otic antibiotics, and corticosteroids.
Conclusion: Traumatic facial nerve palsy is a relatively common presentation to acute care settings. Thorough history and physical exam are essential for early recognition. Misdiagnosis or delay in treatment can result in significant, long-term consequences. If available, prompt CT imaging and ENT consultant involvement are recommended for determination of appropriate disposition and management. If unavailable, as is often the case in UC, immediate ED referral where ENT coverage is available is important to prevent avoidable delays in definitive care.
Introduction
Facial nerve palsy a common presentation to the ED and UC setting. While many cases are idiopathic, an underlying congenital or acquired etiology can sometimes be identified. Acquired causes tend to be infectious, inflammatory, neoplastic, iatrogenic, or traumatic. We present the case of delayed-onset facial nerve palsy 9 days after an auricular and post-auricular gunshot wound.
Case Presentation
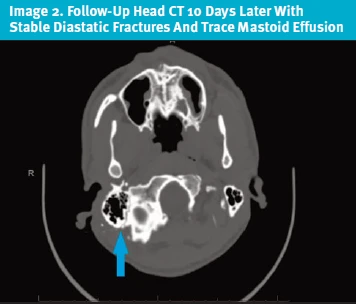
A 29-year-old male with no significant past medical history presented to the ED with right-sided facial droop for 2 days. Nine days prior to presentation, he had been seen in the same ED for a GSW to the back of the head, which resulted in injuries to the superficial auricular and posterior auricular area. At his initial ED presentation, non-contrast head CT demonstrated diastatic temporal bone fractures on the side of the GSW but was otherwise unremarkable (Image 1). He was discharged the same day with prophylactic amoxicillin-clavulanic acid after having his wound closed by the ENT on-call who had evaluated the patient in the ED. He reported he had been compliant with taking the prophylactic antibiotic. He denied any prior history of facial droop. At the second visit, he noted right-sided ear and head pain but denied fever, chills, otorrhea, or wound drainage.
Physical Exam
On exam, his neurologic and cranial nerve exam revealed no deficits except for an isolated finding suggestive of CN VII (facial nerve) palsy. Specifically, complete paralysis of the right forehead and perioral regions was noted. Closure of the eye was preserved and therefore, his facial nerve palsy was classified as House-Brackman grade 3 (Table 1).1 His otoscopic exam was limited by auricular pain and auditory canal edema. He had an evident auricular and posterior auricular wound with overlying eschar, which was debrided at the bedside. No overlying erythema or purulent drainage was noted, but some bogginess and tenderness overlying the mastoid area was noted.
| Grade | Description | Characteristics |
|---|---|---|
| 1 | Normal | Normal facial function in all areas |
| 2 | Mild dysfunction | Gross: slight weakness noticeable on close inspection; may have very slight synkinesis At rest: normal symmetry and tone Motion: Forehead – moderate-to-good function Eye – complete closure with minimum effort Mouth – slight asymmetry |
| 3 | Moderate dysfunction | Gross: obvious, but not disfiguring difference between two sides; noticeable but not severe synkinesis At rest: normal symmetry and tone Motion: Forehead – slight-to-moderate movement Eye – complete closure with effort Mouth – slightly weak with maximum effort |
| 4 | Moderately severe dysfunction | Gross: obvious weakness and/or disfiguring asymmetry At rest: normal symmetry and tone Motion: Forehead – none Eye – incomplete closure Mouth – asymmetric with maximum effort |
| 5 | Severe dysfunction | Gross: only barely perceptible motion At rest: asymmetry Motion: Forehead – none Eye – incomplete closure Mouth – slight movement |
| 6 | Total paralysis | No movement |
Evaluation and Medical Decision Making
A repeat head CT with and without contrast was obtained, given concern for infection (Image 2), which showed a new small mastoid effusion in comparison with his CT from 9 days prior. There had been no progression of the fractures or new fractures.
Given that the patient had a new, objective neurological deficit in the form of right facial paralysis consistent with a CN VII palsy, ENT was consulted in the ED as this issue was believed to most likely represent a traumatic sequala. Despite the fact that he was clinically well-appearing with reassuring vital signs and a normal temperature, infection/mastoiditis was suspected.
Differential Diagnosis and Final Diagnosis
Given a new, hard/objective neurologic finding, central nervous system (CNS) processes such as ischemic or hemorrhagic stroke were considered. However, the clear presence of forehead involvement, which suggests a cranial nerve rather than central lesion, in addition to the head CT results, made CNS lesions less likely. Given the recent penetrating trauma and the new mastoid effusion on CT, infection (ie, mastoiditis) remained on the differential, and bedside incision and drainage was performed by ENT without resultant purulent drainage. In discussion with ENT, the patient was diagnosed with a traumatic right facial nerve palsy.
He was discharged home with 2-day ENT follow-up, oral ciprofloxacin, a 7-day course of prednisone, and ciprofloxacin-dexamethasone otic drops. He was also given lubricating eye drops and instructions on eyelid taping in consideration for possible progression of the palsy and issues with eyelid adduction and subsequent corneal erosions.
Case Resolution
When the patient was seen in the ENT clinic 2 days later, his House-Brackman score remained 3. The antibiotics were stopped, but the 7-day course of prednisone was continued. A week after this, his House-Brackman was unchanged, and the prednisone was continued for another 4 days. Urgent electromyography (EMG) was obtained in consideration of possible facial nerve decompressive surgery. After this time, he was unfortunately lost to follow-up, however, and the remainder of his clinical course is unknown.
Discussion
The facial nerve is the most commonly injured cranial nerve after blunt head trauma,2 and trauma (including iatrogenic) is the second most frequent cause of facial nerve palsy.1 This can occur with or without temporal bone fractures and can present with either immediate or delayed onset. Temporal bone fractures result in facial nerve injury in approximately 7% of cases.3 For patients with immediate onset, the diagnosis is less difficult, and the prognosis for recovery is poor. These patients will often undergo surgical exploration.4
In contrast, delayed onset of symptoms has a more favorable prognosis and is associated with near-complete to complete recovery in 90% of patients.5 Delayed onset of facial paralysis after temporal bone fracture appears to be relatively uncommon.6 As opposed to the more common idiopathic facial nerve paralysis (ie, Bell’s palsy), in the setting of recent head trauma, patients with facial paralysis benefit from rapid ENT evaluation. This is true even in cases where head CT does not show temporal bone fractures or other significant findings, as facial nerve edema may require urgent decompressive surgery to ensure optimal prognosis for recovery.4,7 In clinical settings without access to CT imaging or immediate ENT consultation, the knowledge that delayed onset facial nerve palsy can occur as a complication following head trauma can help the astute UC clinician recognize the importance of ED referral, which is often not indicated in typical cases of Bell’s palsy.
Imaging combined with a thorough history and physical exam is central to the evaluation of patients with facial nerve palsy immediately after head trauma as well as in cases with somewhat delayed presentations. Initial evaluation of such patients with possible traumatic facial nerve palsy begins with non-contrast head CT. Additional high-resolution CT of the temporal bones may also be helpful.8 In cases of traumatic facial nerve palsy without causality found on CT, proceeding with magnetic resonance imaging (MRI) is indicated.8,9 Dedicated imaging studies, such as temporal bone CT or MRI, can often be deferred after an initial negative head CT in cases where rapid ENT follow-up is arranged.
EMG and electroneurography may also be used by specialists to confirm the initial diagnosis or to serially track progress or degeneration. These studies, however, are not emergently indicated and can be ordered at the discretion of the consulting specialist in an outpatient setting.8,9,10
The House-Brackman is the standard scoring system for quantifying the severity of facial nerve paralysis. (Table 1) This system is useful for quantifying the patient’s status and facilitating discussions with consultants. Treatment recommendations differ based on the severity of the facial paralysis.2,4,7,11
Although of questionable utility, the mainstay of treatment for traumatic facial nerve palsy are systemic corticosteroids.7 Similar to the treatment of Bell’s palsy, steroid treatment recommendations are typically a 5-7 day burst.12 If there is concern for concurrent otitis media or mastoiditis, systemic antibiotics are appropriate as well.13 While severe cases of Bell’s palsy are often treated with antiviral therapy, there is no indication for antivirals in traumatic facial nerve palsy. Finally, eye care for patients with incomplete eye closure (taping eyelids closed at night and using eye lubricant or artificial tears during the day) is an important component of therapy in both Bell’s palsy and traumatic facial nerve palsy.14
Ethics Statement
The patient was unable to be contacted because he was lost to follow-up in our hospital system and did not respond to calls to the phone number on record by the research team. Therefore, demographics and some details of the case were changed to protect patient anonymity and confidentiality.
Takeaway Points for Urgent Care Clinicians
- Traumatic facial nerve palsy can occur somewhat commonly after head injury.
- Thorough history and physical exam are essential in early recognition. Mistaking traumatic facial paralysis for Bell’s palsy can delay treatment and have lifelong consequences.
- Prompt imaging and otolaryngology consultation are critical in determining disposition and management. Initial therapies may range from oral corticosteroids to surgical decompression.
Manuscript submitted January 21, 2024; accepted February 29, 2024.
References
- House JW, Brackmann DE. Facial Nerve Grading System. Otolaryngology–Head and Neck Surgery. 1985;93(2):146-147. doi:10.1177/019459988509300202.
- Odebode TO, Ologe FE. Facial Nerve Palsy after Head Injury: Case Incidence, Causes, Clinical Profile and Outcome. J Trauma. 2006;61(2):388-391. doi:10.1097/01.ta.0000224140.26660.5c. Accessed April 7, 2021.
- Cervenka B, et al. Treatment of Temporal Bone Fractures. J Neurosurg. 2016;77(5):419-429. doi:10.1055/s-0036-1584197.
- Honnurappa V, et al. Facial Nerve Decompression after Temporal Bone Fracture—the Bangalore Protocol. Front Neurol. 2019;10. doi:10.3389/fneur.2019.01067. Accessed November 8, 2021.
- Li Q, et al. Clinical Features and Outcomes of Delayed Facial Palsy after Head Trauma. Auris Nasus Larynx. 2016;43(5):514-517. doi:10.1016/j.anl.2015.12.017.
- Exadaktylos AK, et al. The Clinical Correlation of Temporal Bone Fractures and Spiral Computed Tomographic Scan: A Prospective and Consecutive Study at a Level I Trauma Center. J Trauma. 2003;55(4):704-706. doi:10.1097/01.ta.0000038550.11890.a5. Accessed May 17, 2022.
- Nash JJ, et al. Management and Outcomes of Facial Paralysis from Intratemporal Blunt Trauma: A Systematic Review. Laryngoscope. 2010;120(7):1397-1404. doi:10.1002/lary.20943. Accessed April 19, 2021.
- Rotondo M, et al. Post-Traumatic Peripheral Facial Nerve Palsy: Surgical and Neuroradiological Consideration in Five Cases of Delayed Onset. Acta Neurochir (Wien). 2010;152(10):1705-1709. doi:10.1007/s00701-010-0747-x. Accessed October 21, 2021.
- Jäger L, Reiser M. CT and MR Imaging of the Normal and Pathologic Conditions of the Facial Nerve. Eur J Radiol. 2001;40(2):133-146. doi:10.1016/s0720-048x(01)00381-3. Accessed May 1, 2020.
- Cools MJ, Carneiro KA. Facial Nerve Palsy Following Mild Mastoid Trauma on Trampoline. Am J Emerg Med. 2018;36(8):1522.e1-1522.e3. doi:10.1016/j.ajem.2018.04.034. Accessed August 29, 2019.
- Sun DQ, et al. Surgical Management of Acute Facial Palsy. Otolaryngol Clin North Am. 2018;51(6):1077-1092. doi:10.1016/j.otc.2018.07.005. Accessed June 3, 2021.
- Garro A, Nigrovic LE. Managing Peripheral Facial Palsy. Ann Emerg Med. 2018;71(5):618-624. doi:10.1016/j.annemergmed.2017.08.039. Accessed March 14, 2021.
- Bilge S, et al. Peripheral facial nerve palsy in children: clinical manifestations, treatment and prognosis. Egypt J Neurol Psychiatr Neurosurg. 2022;58(1):152. doi:10.1186/s41983-022-00596-1.
- de Almeida JR, et al. Management of Bell palsy: clinical practice guideline. CMAJ. 2014;186(12):917-922. doi:10.1503/cmaj.131801.
Author Affiliations: David Hourani, MD, Augusta University Medical Center, Department of Emergency Medicine. Bradley M. Golden, DO, Augusta University Medical Center, Department of Emergency Medicine. Daniel McCollum, MD, Augusta University Medical Center, Department of Emergency Medicine. John R. Barrett, MD, Augusta University Medical Center, Department of Emergency Medicine. Authors have no relevant financial relationships with any ineligible companies.
Read More
- Hearing The Hoof Beats Of Zebras! Facial Nerve Palsy: A Case Report
- Rash, Facial Palsy, And Ear Pain
