Urgent message: Acute ankle injuries can progress to chronic issues. It is essential that the urgent care clinician be aware of the mechanisms of common ankle injuries, their pathophysiology, essential diagnostic tests, and which injuries require transfer for a higher level of care.
LISA SCHUERMAN, RN, MSN, APNP
Introduction
The ankle is one of the most common sites for acute musculoskeletal injuries, with sprains accounting for 75% of ankle injuries. The ankle joint is composed of the tibia, fibula, and talus. The ligaments bind the bones together. Ankle sprains occur when the ligament is stretched beyond its limits and ligament fibers tear. An ankle injury, if not properly treated by the urgent care clinician, can result in long-term chronic ankle instability
Case Presentation
Emily is a 20-year-old collegiate soccer player. She presents to an urgent care center, reporting that she has had foot pain for the preceding week. She reports that she was seen by her primary-care provider 1 week earlier, and the physician diagnosed a grade I ankle sprain. Her injury occurred while playing soccer 7 days earlier. Initially, she did not have pain on the lateral side of her foot—only on the lateral side of the ankle. She completed a week of RICE (rest, ice, compression, and elevation) with analgesics, but her pain continued. She ambulates with an antalgic gait. Her vital signs are normal. Assessment of the foot reveals swelling over the fifth metatarsal. X-ray results are pending.
Background
It is vital for the health-care provider to be aware of the tests and treatments required for proper patient care. In addition, the provider must know which patients require a higher level of care in an emergency department (ED) or at an orthopedic clinic to help prevent chronic issues. Acute ankle trauma is responsible for 10% to 30% of sports-related injuries in young athletes.1 Each year, an estimated 1 million people in the United States present to clinicians with acute ankle injuries.2 More than 40% of ankle sprains have the potential to cause chronic problems.3 There are different types of ankle sprains, which are graded according to the amount and type of damage to the ligaments and stability. In addition, the Ottawa ankle rules are helpful for determining a diagnosis. Clinical knowledge of ankle injuries is usually limited in practitioners’ training. Therefore, urgent care providers must become familiar with what laboratory tests must be ordered, what examination techniques to use, and how to interpret test results.
Pathophysiology
There are three main groups of ankle ligaments: the deltoid (medial), talofibular (lateral), and the syndesmosis. The deltoid ligaments support the medial part of the ankle. Four ligaments make up the deltoid ligament and form a triangle in the medial portion of the ankle. An injury to the medial part of the ankle is usually associated with a fracture (Figure 1).
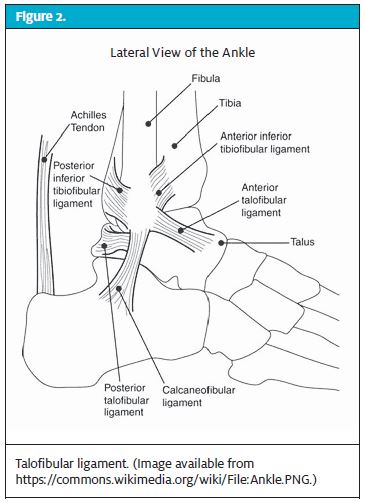
The talofibular ligaments support the lateral part of the ankle. This is the weakest portion of the ankle joint, and thus many sprains occur here on the lateral side. The majority of ankle sprains are inversion injuries and are in this category (Figure 2).
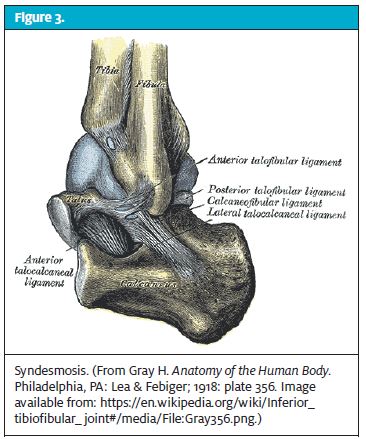
 The interior ligaments make up the syndesmosis, which connects the tibia and fibula (Figure 3). Between 5% and 10% of ankle injuries occur here. These are high ankle sprains, which are caused by sudden twisting injuries and require expert care and follow-up with an orthopedic practitioner.
The interior ligaments make up the syndesmosis, which connects the tibia and fibula (Figure 3). Between 5% and 10% of ankle injuries occur here. These are high ankle sprains, which are caused by sudden twisting injuries and require expert care and follow-up with an orthopedic practitioner.
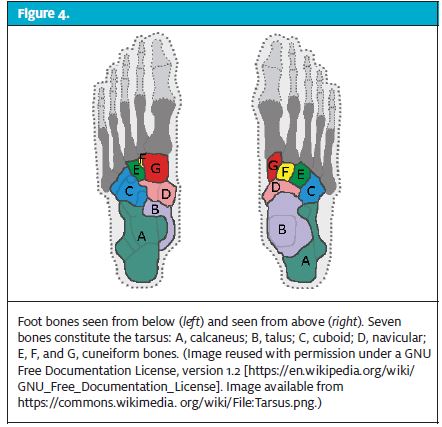
Figure 4 shows the bones of the foot.
Medical History and Physical Examination
A thorough medical history is needed to help guide the practitioner through a complete physical examination. Questions that practitioners should ask themselves include the following:
- What types of laboratory and other investigative tests are important to perform?
- Are x-rays necessary in this case?
- What treatments are beneficial in this situation?
- Does this patient need referral to a higher level of care?
These are important aspects of the medical history:
- When did the injury occur?
- How did the injury occur? What is the mechanism of injury?
- What is the quality of the pain?
- Is there radiation of the pain?
- What is the severity of the pain?
- How long has this been going on, and what changes have occurred? Has this ever occurred before in this patient?
 Examination of the ankle should be done with the patient standing, walking, and then sitting. First have the patient stand, so that you can examine the ankle in the “normal” position. Inspect the ankles and feet and then compare the injured joint with the noninjured joint, looking for symmetry. Next, ask the patient to walk without shoes or socks, and observe their gait. The patient should be able to walk normally on their toes and heels, placing one foot in front of the other. Any variance should be documented. Then, observe the feet and ankles while the patient dangles their legs off the table. You should note slight plantar flexion and inversion of the feet. Here, you will want to palpate the patient’s medial and lateral malleoli. Remember, the distal portion of the fibula constitutes the lateral malleolus. At this point, you should also palpate the Achilles tendon and perform the squeeze test to ensure that the Achilles tendon is intact and that there is not a tear in the syndesmosis between the distal tibia and fibula. Differential diagnoses include sprain, fracture, and dislocation.
Examination of the ankle should be done with the patient standing, walking, and then sitting. First have the patient stand, so that you can examine the ankle in the “normal” position. Inspect the ankles and feet and then compare the injured joint with the noninjured joint, looking for symmetry. Next, ask the patient to walk without shoes or socks, and observe their gait. The patient should be able to walk normally on their toes and heels, placing one foot in front of the other. Any variance should be documented. Then, observe the feet and ankles while the patient dangles their legs off the table. You should note slight plantar flexion and inversion of the feet. Here, you will want to palpate the patient’s medial and lateral malleoli. Remember, the distal portion of the fibula constitutes the lateral malleolus. At this point, you should also palpate the Achilles tendon and perform the squeeze test to ensure that the Achilles tendon is intact and that there is not a tear in the syndesmosis between the distal tibia and fibula. Differential diagnoses include sprain, fracture, and dislocation.
Grading
Grading of ankle sprains focuses on the degree of ligament damage. A grade I sprain, stretching without tearing of the ligament or without instability of the joint, can be fitted with an ankle stirrup-type splint. The patient can be given crutches, be given instructions on their use, and be prescribed a nonsteroidal anti-inflammatory agent, such as ibuprofen, 200 to 800 mg every 6 hours. Teaching the RICE mnemonic to the patient regarding home treatment is helpful. Follow-up for grade I sprains includes use of an ankle stirrup and engaging in weight-bearing as tolerated. Crutches should be used for the shortest time possible. The patient can return to their primary-care provider in about 2 weeks for further follow-up if needed. Once the patient can ambulate without pain and range-of-motion exercises do not cause pain, the patient can then begin strengthening the muscles surrounding the joint.
In a moderate sprain, or a grade II sprain, there is some tearing and instability. There is usually more swelling and ecchymosis than there is in a grade I sprain. Point tenderness may also be present, with a resulting loss of joint function. Treatment for a grade II sprain is the same as for a grade I, with the addition of a Jones cast or a walking boot. For a grade II sprain, physical therapy may also be required. Crutches will also be needed, because staying off the foot will be imperative for the first 5 to 7 days to prevent chronic issues.
 For severe sprains, or grade III sprains, treatment includes placing the patient in a large, bulky dressing or a Jones cast. Alternatively, a walking boot can be used to prevent the patient from using crutches and yet allow participation in activities of daily living. The walking boot may be a better alternative for some patients, but it is expensive. It should be used for about 4 to 6 weeks, with follow-up care by an orthopedist.
For severe sprains, or grade III sprains, treatment includes placing the patient in a large, bulky dressing or a Jones cast. Alternatively, a walking boot can be used to prevent the patient from using crutches and yet allow participation in activities of daily living. The walking boot may be a better alternative for some patients, but it is expensive. It should be used for about 4 to 6 weeks, with follow-up care by an orthopedist.
A computed tomography (CT) scan may be useful to assess the degree of injury for grade III or syndesmotic injuries. Grade I sprains usually do not require an x-ray. However, radiographs of a grade II or III sprain may be necessary to rule out an ankle fracture, especially if the patient is unable to ambulate immediately after the injury occurred or cannot take four steps in your presence. You do not want to miss a high ankle fracture, because there is the possibility of chronic pain and instability.
Diagnostic Testing
Helpful diagnostic modalities include x-ray, CT, and magnetic resonance imaging (MRI).
- X-rays can
- Help rule out a strain versus a fracture
- Help in assessing narrowing of the space between the bones, which are normally covered by cartilage; narrowing can be a sign of arthritis
- Help in evaluating bone spurs, which are overgrowths of a joint and can be a sign of osteoarthritis
- Show a fracture
- CT can
- Help in the evaluation of ankle pain
- Depict cross-sectional slices of the ankle
- Help in the diagnosis of ankle fractures and can show soft tissue such as cartilage, ligaments, and muscles
- Show arthritis and sprains
- MRI can
- Show soft-tissue structures
- Show the bone, which is very useful in diagnosing injuries of the cartilage, tendons, and ligaments
Management of Specific Injuries
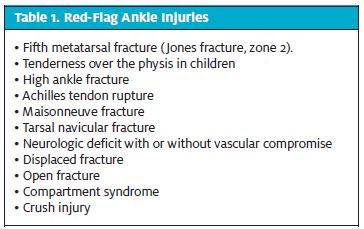
Table 1 lists red-flag ankle injuries.
 Ankle Strain
Ankle Strain
The most appropriate treatment for ankle sprains depends on which grade they are. The treatment is usually RICE. Resting time depends on the grade of the injury and can vary from 5 days for lower-grade to up to 6 weeks for severe tears or grade III sprains.
Fifth Metatarsal Fracture
Table 2 lists metatarsal fractures by zone. Multiple classification systems are used to describe the fractures. For example, there is the Torg classification system, which is used for fractures that are within 1.5 cm of the metatarsal tuberosity.4
Fractures of the fifth metatarsal can be easily missed (Figure 5). A Jones fracture (Figure 6) located in zone 2 is usually the result of a jumping or pivoting activity like basketball or soccer. The patient may have mild or severe pain and will usually have point tenderness over the fifth metatarsal. Treatment always requires avoidance of weight-bearing and use of a cast for 6 to 8 weeks, as long as the fracture is not displaced.
High Ankle Sprain or a Syndesmotic Sprain
Syndesmotic sprains, also called high ankle sprains, occur with rotational injures like external rotation or with high-impact sports such as soccer. Detecting high ankle sprains is imperative because the syndesmotic ligament connects the tibia and fibula, and a high ankle sprain can also accompany a fracture. Testing for this type of sprain or fracture includes the squeeze test and the external rotation test. One or both of these tests will elicit pain from a patient with a syndesmotic sprain. An x-ray will also be needed to rule out a fracture. Treatment for these sprains includes RICE (Table 3). If there is moderate to severe pain and the patient requires a walking boot, instruct them to wear the boot for up to 6 weeks. A good measure of healing is the hop test. If there is not a fracture and the patient can hop 15 times on the foot, then strengthening and weight-bearing can begin. A fracture requires use of a cast and avoidance of weight-bearing for up to 12 weeks. A displaced fracture may need surgical intervention to prevent chronic issues in the future.
Achilles Tendon Rupture
The Achilles tendon is the largest tendon in the body, connecting the calf muscles to the heel bone. The Achilles tendon can be torn during high-impact sports such as running and jumping, with the patient reporting a pop or snap and immediate sharp pain in the calf. Surgery is almost always required and merits a transfer to the ED and consult with an orthopedist.
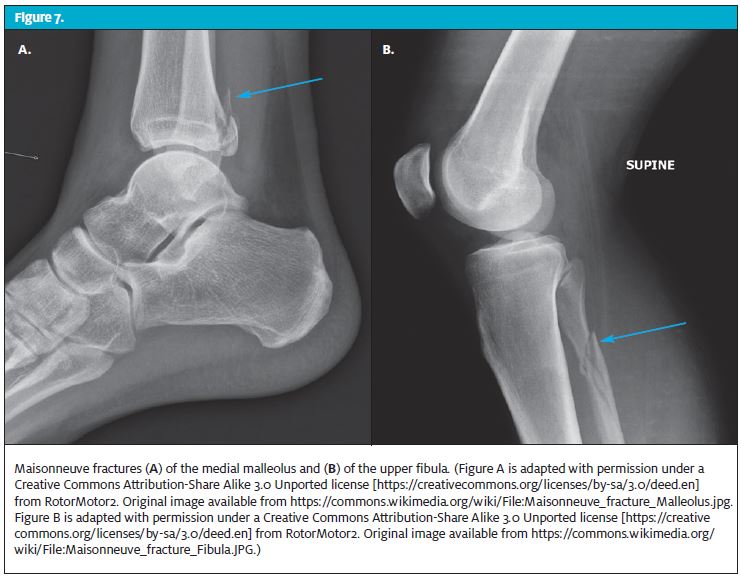
Maisonneuve Fracture
The Maisonneuve fracture (Figure 7) is both a fracture and a sprain and usually occurs from a falling accident related to a sporting event. The patient will have pain in the upper part of the fibula or tibia, and the ankle will feel quite unstable. The patient may have difficulty walking on it. This type of fracture generally requires surgical intervention along with the basic interventions for a sprain. Crutches will be needed for up to 12 weeks. Transfer to the ED and orthopedic referral will be needed.
Tarsal Navicular Fracture
A tarsal navicular fracture is usually diagnosed when there is a high level of suspicion for it. This fracture can be missed because of a lack of knowledge on the provider’s part, resulting in a delayed diagnosis. The patient may have pain in the forefoot. The mechanism of injury is related to the localization of stress placed on an avascular navicular bone. A navicular fracture is generally a stress-related fracture in a runner or someone who presents with vague mid-foot pain. Unfortunately, this fracture does not show up well on x-ray because of the many bones overlapping in the area. In addition, the talonavicular nerve runs along the medial portion of the arch of the foot and thus is involved in mid-foot pain. This can make for a tricky diagnosis and is usually not one that clinicians think about. If the x-ray findings are unequivocal, the clinician should then order a bone scan, followed by a CT scan. Treatment is RICE, followed with avoidance of weight-bearing and use of a cast and crutches for 6 to 12 weeks, with duration depending on how quickly the fracture heals. If one of these fractures is found, the patient must be evaluated by an orthopedist.
Avulsion Fracture
An avulsion fracture occurs when a bone fractures and a portion of it is torn away from the main mass of the bone. This is usually a result of a physical trauma such as a fall or a pull. Generally, this does show up on a simple x-ray. Treatment for this fracture is the same as for a sprain, assuming it is a nondisplaced fracture. For a displaced fracture, internal fixation and reduction by an orthopedic surgeon will be required.
Case Resolution
Assessment of Emily’s injured foot reveals continued swelling over the fifth metatarsal. Further assessment reveals tenderness on the lateral fifth metatarsal. Before her x-ray is read, you suspect a fifth metatarsal fracture. While you are explaining to her the difference between a nondisplaced and displaced fracture, the radiologist calls to discuss the x-ray with you. The x-ray shows a zone 2 fracture of the fifth metatarsal—a Jones fracture (Figure 6). You order placement of a non-weight-bearing cast, teach her how to walk with crutches, and instruct her to follow up with an orthopedist in 1 day.
Take-Home Points
- Palpate the entire fibula and tibia.
- Do not disregard medial or lateral malleolar tenderness.
- Always examine the fibular head in ankle injuries.
- Always examine the base of the fifth metatarsal.
- Determine whether the patient can bear weight. If negative x-ray findings are not convincing, then splint the ankle, advise the patient to avoid weight bearing, and recommend follow-up care in 1 week.
- Use caution in those under the age of 18 years. In these patients, ossification is incomplete, there is an increased tendency toward broken bones, and ligaments are stronger than the bones.
- Use extra caution in assessing those with limited cognition and verbalization skills or neuropathies, in those who are intoxicated, those with diabetes mellitus, and in those who are uncooperative.
- Encourage follow-up with a primary-care provider if healing has not begun in 5 to 7 days.
- Although the majority of ankle injuries that are seen in urgent care centers are minor and can be treated on an outpatient basis, keep in mind situations that call for referral for further evaluation
- Barker HB, Beynnon BD, Renstron PA. Ankle injury risk factors in sports. Sports Med. 1997;23:69–74.
- Bennett WF. Lateral ankle sprains. Part II: acute and chronic treatment. Orthop Rev. 1994;23:504–510.
- Safran MR, Benedetti RS, Bartolozzi AR 3rd, Mandelbaum BR. Lateral ankle sprains: a comprehensive review. Part 1: etiology, pathoanatomy, histopathogenesis, and diagnosis. Med Sci Sports Exerc. 1999;31(7 suppl):S429–437.
- Torg JS. Fractures of the base of the fifth metatarsal distal to the tuberosity. Orthopedics. 1990;13:731–737.