Published on
Urgent Message: Fast trackmodels aim to improve patient throughput metrics for low-acuity patients. In this quality improvement project, a process for fast track in the pediatric urgent care significantly improved patient flow.
Hayley L. Ross, MD; Sandra P. Spencer, MD; Traci Ertle, MSN, RN, CPEN; Anthony Watkins, MSN, RN, NE-BC; Mark Feldman, MD; Derrek Massanari, MD, MPH; Bernadette Johnson, MD; Alexandria J. Wiersma, MD
Citation: Ross HL, Spencer SP, Ertle T, Watkins A, Feldman M, Massanari D, Johnson B, Wiersma AJ. Fast Track Improves Patient Flow and Wait Times in the Pediatric Urgent Care: A Quality Improvement Project. J Urgent Care Med. 2024; 18(10):26-33
Abstract
Background: Pediatric urgent care (UC) centers have proliferated across the United States over recent decades. Many emergency departments (ED) use “fast track” models where patients with lower-acuity presentations and those who require fewer resources are triaged with the goal of improving appropriateness and efficiency of care in the ED as a whole. This fast track model, however, has not been widely implemented or studied in UC settings.
Objective: Children’s Hospital Colorado operates a community site that serves urgent care and emergency patients. The hospital receives a high volume of low-acuity pediatric patient presentations, which are evaluated by our urgent care team. With rising site volumes, the length of stay (LOS) and door-to-provider time for UC patients had been increasing at our facility. This quality improvement (QI) project aimed to improve both metrics and monitor for any adverse effects this change may have on ED patient throughput. To accomplish this, we implemented an UC fast track (FT) process.
Methods: A multidisciplinary QI team reviewed our existing process and designed interventions using the define, measure, analyze, improve, control (DMAIC) framework. The team focused on 4 distinct project interventions: repurposing physical space; reallocating staff resources; determining fast track patient criteria; and outlining patient flow through the facility and electronic medical record (EMR). The specific aims were to decrease mean door-to-provider time to <30 minutes and to decrease mean length of stay to <60 minutes.
Results: Following implementation of the FT system, mean UC door-to-provider time decreased from 83 minutes to 21 minutes (upper confidence limit [UCL] 42, lower confidence limit [LCL] 1) and the mean UC LOS decreased from 160 minutes to 102 minutes (UCL 146, LCL 58). ED patient door-to-provider times improved from 44 to 25 minutes (UCL 55, LCL 0).
Conclusion: Using QI methodology, we implemented an urgent care FT process. This decreased both LOS and door-to-provider time for low-acuity patients without negative impact on higher acuity ED patients. This project can serve as a model for other UCs that are struggling to meet goals for these metrics to improve throughput for low-acuity patients who can be rapidly evaluated and discharged.
Introduction
The expansion of dedicated pediatric urgent care (UC) services over the last 20 years has improved the delivery of quality, efficient care for acutely ill and injured children with lower-acuity concerns. Over 35 states now offer pediatric-specific UC facilities, and there are more than 350 discrete pediatric UC locations.1 Though numerous factors contribute to this proliferation, patients and guardians seek UC services with the expectation that care will be cost sensitive and efficient and allow for avoiding more costly care and longer wait times commonly associated with seeking care in both general and pediatric-specific emergency departments (EDs).2
In response to this growth of pediatric UC facilities and in recognition of the developing field of UC medicine, providers and institutions have invested in ensuring the delivery of high-quality care as well as programs to develop leadership and academic advancement in the new field.3 The Society for Pediatric Urgent Care, formed in 2014, aims to further education, academic progression and leadership development within the field of pediatric UC. The American Academy of Pediatrics also has demonstrated concern over quality in pediatric UC and recently started a Section on Urgent Care Medicine.4 Pediatric UC fellowships now exist as a response to the specific clinical competencies required in the field.5 The growing number of care sites and the parallel scholarly development in the field has created a ripe environment for the improvement of care delivery to meet the expectations of families seeking UC services in pediatric centers.
The QI project institution’s community-based hospitals offer ED and UC services that are co-located in the facility. Patients presenting for care undergo triage on arrival to receive either UC- or ED-level services based on guardian preference, medical complexity, chief complaint, and anticipated resource needs. UC patients and ED patients are cared for by 2 distinct provider groups who are intended to function as separate yet complementary teams. At the project institution, both levels of patients are evaluated in dedicated areas within the same department. As site volumes rapidly rose following the COVID-19 pandemic in 2021 and exceeded prior historical volumes, ED-level patients consumed a disproportionate amount of facility resources and impacted availability of dedicated UC space and services. Teams increasingly struggled with efficient delivery of UC services, leading to an increase in door-to-provider and LOS for UC patients. These metrics are worthy of attention as previous work has demonstrated that increased LOS can have negative impacts on patient safety at all acuity levels within a facility.6
A review of the literature shows that other groups have addressed similar issues by implementing low-acuity, fast track (FT) systems within the ED setting.7 Prior studies have demonstrated that implementation of a FT model may improve LOS and door-to-provider times in both general and pediatric EDs.8,9 These models may be particularly impactful in the pediatric setting as low acuity patients represent a disproportionate number all pediatric presentations to ED settings and, therefore, contribute to department overcrowding.10 In addition, patients with low acuity concerns as determined by the Emergency Severity Index (ESI) are also likely to be discharged home and require relatively few resources.11,12 As the project facilities’ patient acuity levels are consistent with national data, it was expected that this FT model could help to meet the project aims without significantly increasing the cost of care or resources required.
Specific Aims
The group aimed to implement a FT model to provide timely care for low-acuity patients triaged to the UC area within our facility. Secondary aims included assessing the impacts of this model on patient throughput metrics. The project goals included decreasing mean UC door-to-provider time to <30 minutes and decreasing mean UC LOS to <60 minutes in the first 6 months of implementation.
Methods
The project site is a community-based satellite location for a quaternary care pediatric medical center. The ED and UC are located within the same physical space, and all patients access services through a single entrance. The clinical teams are assigned to distinct UC and ED shifts. Services available within the UC setting are clearly defined, and the scope is consistent among all institutional locations that offer UC services. The UC area is open from 11AM-8PM daily and serves patients ages 0-22 years of age. Patients presenting for care during hours when the UC is open are initially assessed upon arrival by a registered nurse (RN) and assigned to be evaluated within the UC or ED based on chief complaint, anticipated resources, medical complexity, and guardian request. In the project facility, normally >50% of patients presenting during UC hours are triaged to the UC area.
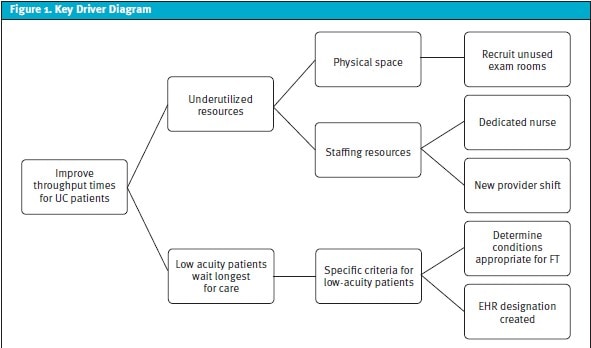
A quality improvement (QI) team was established; team members included UC facility leadership, nursing staff, advanced practice providers, and physicians. Using the define, measure, analyze, improve, control (DMAIC) framework, the group mapped the preintervention processes over a several month period.13 The group identified 4 primary components of the project: physical space; staffing resources; determination of fast track patient criteria; and patient flow through the facility and EHR. A key driver diagram helped to aid in project implementation (Figure 1).
To address the physical space, the team identified and recruited 3 underutilized exam rooms. Their location at the front of the UC space, close to the waiting room, made them ideal for allowing easy movement for patients between the waiting area and triage space. In preparation for patient care, the team ensured these rooms had necessary equipment and supplies. We also included a second, underutilized waiting room located within the department as a space that could function as a dedicated waiting area for FT patients during their visit.
The QI group then focused on allocation of limited staffing resources. With the anticipated rapid patient throughput, the team determined that successful implementation required staff dedicated solely to FT patients. The were no budgetary allowances to add staff for the project, and therefore, plans required revision of the existing staffing model. During the initial intervention phase, the FT team staffed the area for 8 of the 9 hours of UC services because the typical clinician’s shift is 8 hours. The group assigned 1 provider and 1 RN to be responsible for patients in the FT area. In response to staff and provider feedback during the “improve” phase of the DMAIC framework, provider coverage was ultimately expanded. This was accomplished by allocating 1 provider to FT during the first 5 hours of the day and then utilizing another provider scheduled for a previously existing UC shift to cover the remaining 4 hours, while also staying for the final hour to manage overflow patients waiting at the close of UC hours. RN coverage already spanned this timeframe and did not require adjustment. The intended workflow was for both RN and provider to physically evaluate new patients together to promote efficient completion of the triage process as well to rapidly establish a definitive care plan.
The group then considered a list of chief complaints already defined by our institution to meet criteria for UC level care. The group then determined if each complaint could be adequately and efficiently cared for by the FT team. Considering a patient’s ESI level, chief complaint, and anticipated resources, we created a list of inclusion criteria for evaluation in the FT space (Table 1). We validated this list against previously published criteria from other FT projects in the literature.9 We excluded chief complaints that involved a clinician-performed procedure, patient monitoring, or anticipated LOS >30 minutes. Throughout the project period, the multidisciplinary group met regularly and reviewed feedback from staff regarding the inclusion criteria.
| General Criteria for Fast Track | Sample Conditions Triaged to Fast Track | Sample Conditions Triaged to General Urgent Care |
| Meets urgent care criteria Emergency Severity Index level 4 or 5Anticipated length of stay <30 minutes | Croup without respiratory distressEar pain Rash Simple fractures Sore throat | Breathing concerns requiring monitoringDysuria requiring catheterization for urinalysis Incision and drainageLacerationsVomiting requiring oral rehydration |
The group then addressed virtual patient flow through the EMR. Using the original process and UC scope, an RN assigned a patient to “ED” or “UC” level of care in the EMR. With the new process, the RN would assign an additional designation “UC-FT” to denote patients to be seen by the FT team. This designation was added as a comment instead of a distinct class in the EMR. The nursing and clinician staff were also educated on this designation and the indication that such patients were to be seen by the FT team in the FT rooms.
Finally, the team considered patient flow through the physical space. After patients were identified in the EMR, they were called from the general waiting room to be placed in a FT-designated room for vital signs, completion of secondary triage questions, and clinician evaluation. At the completion of evaluation in the FT room, the patients returned to the main waiting room. During followup meetings, the group learned that on particularly high-volume days the general waiting room was crowded and began moving FT patients to the smaller, underutilized waiting room within the ED/UC space to await an open FT exam room.
The primary study outcome measures were mean door-to-provider time for UC level patients and mean LOS for UC patients. The study group selected these measures as they are reported in other FT projects in the literature and reflect the study goal of improving efficient UC patient flow through the department.9,14 Additional process measures included: left without being seen (LWBS) rates for all ED and UC patients; and UC patients still in the waiting room at the end of UC hours.
Balancing measures for this project were the mean LOS for ED patients and the mean door-to-provider time for ED patients, as it was the hope that improved efficiency on the UC side of the facility might positively impact ED throughput metrics. The study group selected these balancing measures due to the facility design and availability of both ED and UC services within the same space.
We assessed intervention effectiveness using x-bar and p statistical process control (SPC) charts. This allowed us to quickly evaluate the process, determine if modifications were required, and plan the next cycle of interventions. We obtained baseline data for the 12 weeks preceeding implementation of the intervention. Data obtained following the intervention was collected for a total of 31 weeks. Center lines were adjusted and data re-centered when there was special cause variation using established special cause rules.15 Upper (UCL) and lower confidence limits (LCL) were established as 3 standard deviations from the mean.
Results
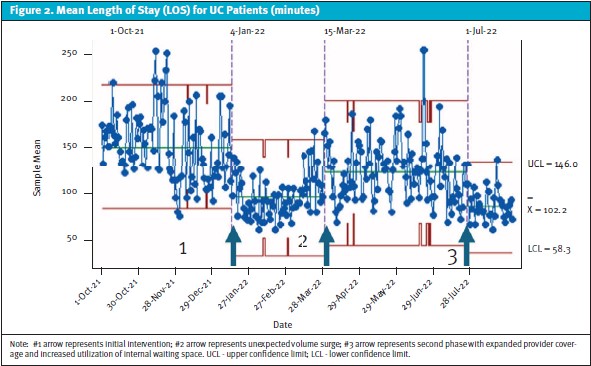
Over the course of the initial phase of the intervention, the mean LOS decreased from 159.8 minutes to 111.4 minutes (Figure 2). Control charts obtained during this time show a sustained decrease in LOS for the first 10 weeks of the intervention. In mid-March of 2022, the facility experienced an unanticipated volume surge. UC LOS again increased but did not reach the pre-intervention baseline. Once volumes returned to expected historical baseline levels, the UC LOS again improved to 102.2 minutes (UCL/LCL ± 44 minutes).
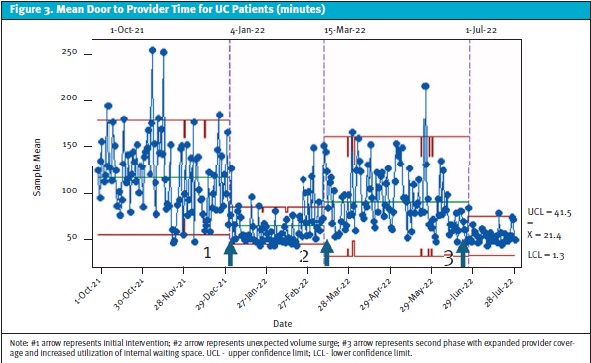
Our second outcome measure was door-to-provider time. During the initial intervention phase mean door-to-provider time decreased from 82.7 minutes to 32.5 minutes (Figure 3). As with the LOS, the improvements were sustained until the volume surge in March 2022. With normalization of volumes during the later phases of the intervention, door-to-provider time again improved below initial intervention mean to 21.4 minutes (UCL/LCL ± 20 minutes).
The team closely monitored process measures throughout the intervention. During the initial phase, LWBS rates also improved from a baseline of 5.9% to 3.5%. The mean number of UC patients in the waiting room at the end of UC hours improved from 6 to 1.13 patients.
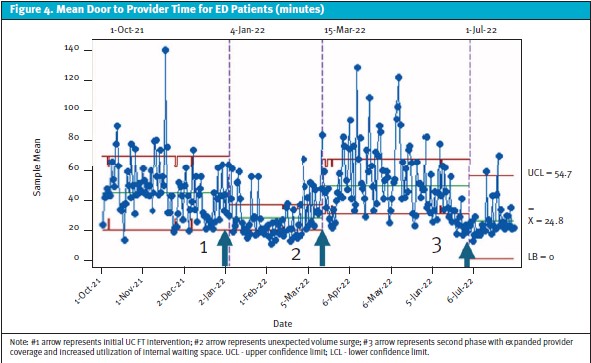
Balancing measures obtained included mean LOS for ED patients and door-to-provider time for ED patients. Our data demonstrated an improvement in door-to-provider time for ED patients during the FT intervention period from 43.7 to 24.8 minutes (UCL +30 minutes, LCL 0 minutes) (Figure 4). With the opening of the FT space, there was also improvement in the mean LOS of ED level patients from 196.7 minutes to 164.8 minutes. This confirmed that the intervention did not adversely impact ED efficiency metrics.
Discussion
This QI project demonstrated the successful implementation of a FT system for UC patients. The project achieved the target outcomes by improving UC door-to-provider time and UC LOS while simultaneously improving these metrics for ED patients as well. The outcomes after the project interventions suggest that a FT model can improve patient throughput in a UC setting. This novel application of the FT model in a UC setting could prove useful considering the national expansion of pediatric UC currently unfolding.
Metric improvements were sustained during the intervention period from baseline in both patient LOS and door-to-provider time for UC patients. Though the improvements observed did not meet the initial pre-project targets in the initial implementation period, the goal for mean door-to-provider time during subsequent phases of the project was attained. Despite not achieving the initial goal for UC LOS, this metric did improve by 35%. Importantly, these improvements were sustained even during the time of unanticipated volume increases during March 2022, suggesting this model can mitigate the adverse effects of surges on throughput metrics.
A unique characteristic of the facility where the project was undertaken is that the care of both ED and UC patients occurs within the same physical space by complementary but distinct care teams. Not only were adverse impacts to throughput of ED patients avoided, but improvements in ED patient LOS and the mean door-to-provider time were also observed. These results suggest that this process may be useful in similar care models where UC and ED settings are co-located.
In creating this process, the group improved the target metrics with creative use of existing human resources and physical space. An additional clinician dedicated to FT patients was added to daily staffing, however, existing nursing staff were simply reallocated to manage FT patients. Thus, the only additional costs related to implementation of the program were the slight increase in clinician hours to adequately staff the FT area of the UC space. As the interventions yielded faster door-to-provider times, shorter LOS, and fewer LWBS, it seems reasonable that these improvements could offset the limited increased expenses of increasing provider coverage. This makes such a plan an attractive option for leaders seeking to positively modify patient flow in the UC setting in a budget-conscious manner.
Although there were many aspects of the initial intervention that functioned as intended, the plan for tandem evaluation by the RN and provider for FT patients proved challenging. The rationale for this intervention was to limit redundancies by minimizing repetitive history taking and ensuring all care team members were aware of the plan simultaneously. However, as the group obtained feedback from providers and RN staff, it became clear that the asynchronous nature of the RN and provider workflows made this component of the intervention impractical to implement. Though tandem patient evaluation may be more achievable at the start of a shift, the individual clinical staff members had different responsibilities that would often preclude them from coming together easily to evaluate the next new FT patient.
This QI project ultimately concluded prematurely due to a nationwide respiratory virus surge of late 2022. During this time, UC and UC FT rooms were allocated to ED patients who were facing prolonged boarding while awaiting inpatient admission, further underscoring how increased inpatient LOS and occupancy portends increases in ED boarding and LOS and negatively affects ED thoughput. Future work exploring implementation of FT programs in UC should explore how to preserve FT workflows even in times of significant volume increases.
Limitations
This QI project was undertaken at a single community-based site associated within a quaternary academic medical center. The instution has experts in quality improvement project development and implementation that may not be available at smaller institutions. The project site cares for both ED and UC patients within the same physical space, though the UC patients are cared for in a distinct area. Therefore, it is certain that this UC functions somewhat differently than many freestanding UC locations. In this project, there was no control site for comparison, and therefore it is uncertain how these metrics may have changed without the intervention.
The implementation and success of the project were dependent on availability of unused physical space, specifically a waiting area and unused exam rooms. Not all centers may have sufficient unused, existing physical space to immediately implement this FT process. Additionally, many UC centers do not have RNs and may have only a single provider staffing them throughout the day. In settings such as these mentioned above, implementation may require more upfront financial investment and time to roll out.
Finally, due to constraints surrounding data extraction from the EMR, it was not possible to separate specific data for FT patients from all UC patients to compare these groups. Addition of a distinct patient class within the EMR to distinguish FT-UC patients from all UC patients would be advisable to those pursuing future work on this topic to permit more granular analysis of patient differences.
Conclusion
This quality improvement project involved developing and implementing a novel fast-track urgent care model. The initiative resulted in a 74% reduction in door-to-provider time and 36% reduction in UC LOS. Interestingly, improvements in these metrics for patients in the co-located ED were also observed. The FT process also continued to function and reduce door-to-provider and UC LOS times during a large volume surge. This work is the only project the authors are aware of involving the implementation of a FT model in a dedicated UC setting. The results of this QI project suggest that a FT model can improve efficiency in an appropriately selected UC setting.
Acknowledgements
The authors would like to acknowledge the work of the entire multidisciplinary group at Children’s Hospital Colorado North Campus and thank the leadership that supported this project.
Ethics Statement
This was a quality improvement project conducted to evaluate and optimize operational processes. It did not involve the collection or analysis of private, identifiable data from human subjects. Therefore, this quality improvement project did not require Institutional Review Board approval and adhered to the ethics policies for Children’s Hospital Colorado.
Manuscript submitted January 29, 2024; accepted June 3, 2024.
References
- Sankrithi U, Schor J. Pediatric Urgent Care-New and Evolving Paradigms of Acute Care. Pediatr Clin North Am. 2018;65(6):1257-1268.
- Gross TK, Lane NE, Timm NL, MEDICINE COPE. Crowding in the Emergency Department: Challenges and Recommendations for the Care of Children. Pediatrics. 2023;151(3).
- Conners GP, Kressly SJ, Perrin JM, Richerson JE, Sankrithi UM, PRACTICE CO, et al. Nonemergency Acute Care: When It’s Not the Medical Home. Pediatrics. 2017;139(5).
- American Academy of Pediatrics, Section on Urgent Care Medicine 2023.
- Patel A, Cohen J, Pattishall A, Berkowitz DA, Coco T, Herold S, et al. The Emergence of Academic Pediatric Urgent Care Fellowships. Pediatr Emerg Care. 2021;37(12):e899-900.
- Carter EJ, Pouch SM, Larson EL. The relationship between emergency department crowding and patient outcomes: a systematic review. J Nurs Scholarsh. 2014;46(2):106-115.
- De Freitas L, Goodacre S, O’Hara R, Thokala P, Hariharan S. Interventions to improve patient flow in emergency departments: an umbrella review. Emerg Med J. 2018;35(10):626-637.
- Berkowitz DA, Brown K, Morrison S, Payne A, Pettinichi J, Schultz TR, et al. Improving Low-acuity Patient Flow in a Pediatric Emergency Department: A System Redesign. Pediatr Qual Saf. 2018;3(6):e122.
- Martin HA, Noble M, Wilmarth J. Improving Patient Flow and Decreasing Patient Length of Stay in the Pediatric Emergency Department Through Implementation of a Fast Track. Adv Emerg Nurs J. 2021;43(2):162-169.
- Li J, Ramgopal S, Marin JR. Resource Utilization During Low-Acuity Pediatric Emergency Department Visits. Pediatr Emerg Care. 2022;38(2):e983-e987.
- Shelton R. The Emergency Severity Index 5-level triage system. Dimens Crit Care Nurs. 2009;28(1):9-12.
- Green NA, Durani Y, Brecher D, DePiero A, Loiselle J, Attia M. Emergency Severity Index version 4: a valid and reliable tool in pediatric emergency department triage. Pediatr Emerg Care. 2012;28(8):753-757.
- Monday LM. Define, Measure, Analyze, Improve, Control (DMAIC) Methodology as a Roadmap in Quality Improvement. Glob J Qual Saf Healthc. 2022;5(2):44-46.
- Celona CA, Amaranto A, Ferrer R, Wieland M, Abrams S, Obusan F, et al. Interdisciplinary Design to Improve Fast Track in the Emergency Department. Adv Emerg Nurs J; 2018;40(3):198-203.
- Nelson L. The Shewhart Control Chart – Test for Special Causes Journal of Quality Technology 1984;16(4):237-239.
Author Affiliations: Hayley L. Ross, MD, Department of Pediatrics, Section of Emergency Medicine, University of Colorado School of Medicine, Aurora, Colorado. Sandra P. Spencer, MD, Department of Pediatrics, Section of Emergency Medicine, University of Colorado School of Medicine, Aurora, Colorado. Traci Ertle, MSN, RN, CPEN, Children’s Hospital Colorado, North Campus. Anthony Watkins, MSN, RN, NE-BC, Children’s Hospital Colorado, North Campus. Mark Feldman, MD, Department of Pediatrics, Section of Emergency Medicine, University of Colorado School of Medicine, Aurora, Colorado. Derrek Massanari, MD, MPH, Department of Pediatrics, Section of Emergency Medicine, University of Colorado School of Medicine, Aurora, Colorado. Bernadette Johnson, MD, Department of Pediatrics, Section of Emergency Medicine, University of Colorado School of Medicine, Aurora, Colorado. Alexandria J. Wiersma, MD, Department of Pediatrics, Section of Emergency Medicine, University of Colorado School of Medicine, Aurora, Colorado.
Download the article PDF: Fast Track Improves Patient Flow and Wait Times in the Pediatric Urgent Care: A Quality Improvement Project
