Published on
Urgent message: The use of all-inclusive kits with compact, table-top analyzers provides a rapid quantification of HbA1c levels in patients. The use of these tests for in-house screening has the potential to increase the diagnoses of early or asymptomatic diabetes in young adults and under-served or overlooked populations.
Jay H. Shubrook, DO; Jane M. Caldwell, PhD; and Lindsey E. Fish, MD
Citation: Shubrook JH, Caldwell JM, Fish LE. HbA1c as screening/diagnosis for early or asymptomatic diabetes in your adults and underserved or overlooked populations. J Urgent Care Med. 2023;17(11):17-20.
Key words: urgent care, diabetes, HbA1c
ABSTRACT
Proactive screening for diabetes promotes early intervention, mitigates progression, and reduces the long-term consequences, expenses, and complications of the disease. The CLIA-waived HbA1c protocol can be performed by relatively untrained operators without prior patient fasting with a simple fingerstick for blood. Alternative screening methods such as non-CLIA-waived HbA1c, plasma glucose, or oral glucose tolerance are time-consuming and uncomfortable, and may require several return visits and fasting. Numerous studies have found HbA1c to be as effective as plasma glucose for screening. There is a growing trend for American adults, especially younger adults, to rely on UC facilities for chronic conditions. UC is the logical place for point-of-care (POC) screening by HbA1c.
INTRODUCTION
Diabetes is a major contributor to morbidity and mortality in the United States. Accounting for greater than 3% of all deaths in 2017, it is the seventh-leading cause of death in America.1 When left untreated, diabetes can lead to vascular and heart disease, kidney failure, limb amputation, and blindness.2 New research now links diabetes to major depressive disorder.3
The economic and social costs of treatment are high, as well. The total economic cost attributed to diabetes in the United States was $327 billion in 2017, representing 24% of all healthcare dollars.4
Reduced quality of life, absenteeism from work, and loss of loved ones by premature death impact not just the affected individuals, but their families, friends, and employers. Diabetes and its complications further burden an already taxed healthcare system.
Early detection of diabetes in adults with defined risk factors is the key to prevention and early treatment among asymptomatic or prediabetic individuals. The prevalence of prediabetes and diabetes has increased among adults in the United States, especially in younger populations. It is estimated that 24% of young adults between 18 and 44 years of age have prediabetes.5 This group has the greatest increase in relative diabetes prevalence and the most to gain from early screening and diagnosis.6 A meta-analysis of U.S. children and adolescents found that 25% of these youth were eligible for diabetes screening.7 HbA1c was cited as a useful nonfasting test in children as it also points to other cardiometabolic risk factors which could be reduced by proactive lifestyle interventions at this early age.
The Shift to Urgent Care
Urgent care centers have become the first level of medical care for a growing number of insured and uninsured Americans.8 Originally expected to provide only episodic acute care,8 urgent care has become the “new normal” healthcare site for many chronic conditions due to the rising need for accessible, rapid, and affordable healthcare. The Urgent Care Association estimates that more than 18% of all primary care visits and nearly 10% of all outpatient physician visits occur in urgent care centers.9 Healthcare has been historically difficult for patients to navigate. Many UC providers are now affiliated with primary care facilities which can streamline referrals.
In a 2019 health statistics report, the Centers for Disease Control and Prevention10 revealed that 32% of women and 26% of men in the U.S. had one or more visits to an urgent care center or retail health clinic (RHC) in a 12-month interval. Use of these “convenience” facilities decreased as age increased, pointing to use by younger adults. UC and RHC use also increased with increasing education levels. The CDC report recommended UC and RHC as providers of preventive care services such as vaccinations. UC facilities could adjust and respond to this trend from acute to chronic care by providing further preventive care services such as diabetes screening and referral of chronic conditions to primary care.
The Need for Point-of-Care Screening
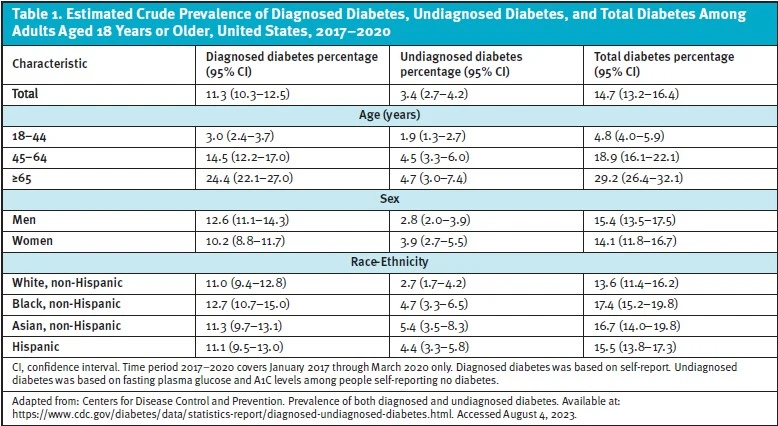
There are no definitive early signs or symptoms that can reliably diagnose type 2 diabetes. Early diagnosis requires a systematic screening program for at-risk patients. Research has shown that 8.5 million adults aged 18 years or older who met laboratory criteria for diabetes were not aware of or did not report having diabetes.11 This represents 2.8% of all U.S. adults and 21.4% of U.S. adults with diabetes.11
Previously undiagnosed diabetes and impaired glucose tolerance are common in patients with an acute myocardial infarction. In one study, approximately 25% of patients experiencing acute myocardial infarction were found to also have type 2 diabetes.12 One third of newly diagnosed diabetes patients find they already have a complication due to the disease.12 The likelihood of screening was higher with POC systematic screening than with use of an off-site lab test for screening.13 POC screening also was more likely to find prediabetes (53% vs 32% for POC and off-site lab, respectively.13) Nearly three quarters of the people who presented to the hospital with hyperglycemia but did not have known diabetes would have had the identification of chronic hyperglycemia with a HbA1c test.14
Comparison of Diabetes Screening Methods
For diabetes, in contrast to other diseases there is no distinction between screening and diagnostic testing.15 Therefore, the same tests are used for both purposes. Glycated hemoglobin, or hemoglobin A1c (HbA1c), was first noted in patients with diabetes by Rahbar in 1969. With recent advances including the proper instrumentation and kits, the HbA1c protocol can be performed by relatively untrained operators without prior patient fasting with a simple fingerstick for blood. The measurement of this deviant hemoglobin has become common practice for monitoring the progression and control of patients with known diabetes as it quantitates average blood glucose levels over several months.
The plasma glucose (PG) test is a one-point measurement which quantifies the patient’s plasma glucose concentration at the time of collection only. Because this concentration can fluctuate due to many factors, PG can miss patients who are below the cutoff range for positive diagnosis at that particular time. HbA1c is an average measurement of glycated hemoglobin over time. For comparison, PG is a point measurement while HbA1c is the slope of a line drawn through many points over time. The HbA1c is unique in that it does not require the person to fast and now can be done during the same appointment by venipuncture or POC fingerstick.
An older diabetes screening method, oral glucose tolerance (OGT), is costly, invasive, and inconvenient for patients. Healthcare providers risk losing patients who can’t or won’t overcome these hurdles to follow-up appointments.
Advantages of HbA1c Screening
POC HbA1c instrumentation became available in the 1990s.16 Results are generally available within 10 minutes and require a finger prick for whole blood, similar to the test for the glucometer. Prior fasting by the patient is not required, so the test can be administered spontaneously and does not require a return visit. The FDA has CLIA-waived most POC HbA1c testing, deeming the procedure so simple that there is little risk of error. No specific training is required for test operators who are exempt from other CLIA inspections and requirements.16
Cost Advantages of POC testing
Several studies indicate that POC HbA1c testing results in cost savings for both the patient and the greater healthcare system. While the single unit cost of POC HbA1c can be higher17 than other screenings, when factoring in the cost of additional visits for asynchronous testing it is less costly to use HbA1c in the long-term.18 A recent study published in The Journal of Urgent Care Medicine used HbA1cas a screening method in UC facilities. At-risk individuals were identified with an Early Diabetes Detection Pathway (EDDP)protocol.8 When combined with EDDP, HbA1c was found to be an efficient, rapid, and low-cost method to screen previously undiagnosed prediabetes and diabetes patients.
LIMITATIONS
Racial and ethnicity factors need to be considered during screening. It is known that some Asian populations have hemoglobin variants and other conditions that affect red cell turnover.20
Nonglycemic factors may also affect the measurement of HbA1c.2 Acute blood loss, chronic liver disease, hemolytic anemias, antiretroviral treatments, pregnancy, and vitamins E and C can falsely lower HbA1c.
Factors which may falsely elevate HbA1c are aplastic anemias, hyperbilirubinemia, hypertriglyceridemia, iron deficiency anemias, renal failure, and splenectomy.
Malnutrition can either lower or elevate HbA1c levels.
Healthcare providers should be aware of these confounding factors and consult a checklist to evaluate and consider their potential impact when a positive test occurs. POC HbA1c screening errs on the side of false positives. A referral could suggest other confirming tests such as plasma glucose if these factors are present.
The cost of false positives to the medical community and patients is low compared with the cost of missing a diagnosis in an asymptomatic patient. Some researchers recommend using both glucose and HbA1c as complementary screening protocols to reduce the risk of false positives and improve and hasten diagnoses.1
One study characterized HbA1c performance and compared it to fasting plasma glucose (FPG) among 3,540 Chinese, Malay, and Indian patients.20 HbA1c screening identified 95% of the individuals with diabetes; the remaining 5% had impaired glucose tolerance. The authors recommended HbA1c as an alternative to FPG screening among the ethnic communities tested. Furthermore, they recommended lowering the testing concentrations to a combination of HbA1c >6.1% and FPG >5.6 mmol/L to improve identification of prediabetes and diabetes in that population.20
According to the U.S. Preventive Task Force Services (USPTFS)20 and the American Diabetes Association,21 the HbA1c test should be performed using a method that is certified by the NGSP and standardized or traceable to the Diabetes Control and Complications Trial (DDCT)reference assay. It states, “Point-of-care A1C assays have not been prospectively studied for the diagnosis of diabetes and are not recommended for diabetes diagnosis; if used, they should be confirmed with a validated measure. POC HbA1c may be more generally applied for assessment of glycemic control in the clinic.”22
Insurance Reimbursement for HbA1c Screening
Both HbA1c and PG tests are reimbursed by Medicare and other insurers for patients with known diabetes.1 However, as of this writing, HbA1c is not covered by Medicare for screening of at-risk asymptomatic patients. The USPSTF has given HbA1c screening a grade B for routine screening of asymptomatic patients and implies that it is duplicative to glucose in this use.1 Health plans need to recognize the utility of HbA1c and provide coverage for this test.
In a study looking at differences in HbA1c screening among U.S. adults, the results indicated that despite having health insurance, people of color (such as Hispanic and African Americans) were less likely to have their HbA1c monitored by their healthcare provider.23 Further studies were advised to assess the impact of these racial disparities.
CONCLUSIONS
- Rapid POC HbA1c screening has been shown to increase detection of diabetes and prediabetes.
- HbA1c screening at POC is more cost-effective in the long-term for the patient and the healthcare system.
- Urgent Care, dental office and community health service screenings can all provide early detection and improve health outcomes for patients and their communities.
Manuscript submitted April 13, 2023; accepted May 17, 2023.
References
- Hilborne LH, Bi C, Radcliff J, et al. Contributions of glucose and hemoglobin A1c measurements in diabetes screening. Am J Clin Pathol. 2022;157(1):1-4.
- Pippitt, K, Li M. Diabetes mellitus: screening and diagnosis. Am Fam Physician. 2016;93:103-109.
- Watson KT, Simard JF, Henderson VW, et al. Incident major depressive disorder predicted by three measure of insulin resistance: a Dutch cohort study. Am J Psychiatry. 2021;178(10):914-920.
- Wang L, Li X, Wang Z, et al. Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, 1999-2018. JAMA. 2021;326(8):1-13.
- Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020: Estimates of diabetes and its burden in the United States. Available at: http://www.cdc.gov/diabetes/data/statistics-report/index.html. Accessed August 4, 2023.
- Gregg EW, Moin T. New USPSTF recommendations for screening for prediabetes and type 2 diabetes. An opportunity to create national momentum. JAMA. 2021;326(8):701-703.
- Wallace AS, Wang D, Shin JI, Selvin E. Screening and diagnosis of prediabetes and diabetes in US children and adolescents. Pediatrics. 2020;146(3):e20200265.
- Clark SR, Wilson ML. Original research: early diabetes screening in the urgent care, part 2. J Urgent Care Med. 2016;11(1):27-33.
- Stoimenoff L., Newman N. . Urgent Care Industry White Paper 2018: The Essential Role of the Urgent Care Center in Population Health.
- Black LI, Adjaye-Gbewonyo D. Urgent care center and retail health clinic utilization among adults: United States 2019. NCHS Data Brief No. 409. June 2021. Available at: https://www.cdc.gov/nchs/products/databriefs/db409.htm.
- American Diabetes Association. 2023. https://www.cdc.gov/diabetes/data/statistics-report/diagnosed-undiagnosed-diabetes.html.
- Norhammar A, Tenerz A, Nilsson G, Hamsten A, Efendíc S, Rydén L, Malmberg K. Glucose metabolism in patients. https://pubmed.ncbi.nlm.nih.gov/12090978/.
- Whitley PB. Systematic Diabetes Screening Using Point-of-Care HbA1c Testing Facilitates Identification of Prediabetes. Ann Fam Med. 2017;15(2). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5348235/.
- Jones D, Scharfenberg B, Perkins J, Childers K, Dogbey G, Shubrook JH. Glycated Hemoglobin (HbA1c) Identifies Undiagnosed Chronic Hyperglycemia in the Inpatient Setting. J Am Osteopath Assoc. 2016;116:350-357.
- Ekoe J-M, et al. Screening for diabetes in adults. Can J Diabetes. 42:S16-S19.
- Johns Hopkins Diabetes Guide. Point-of-care HbA1c machines. https://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_Diabetes_Guide/547180/all/Point_of_care_HbA1c_machines.
- Lee-Lewandrowski E, Lewandrowski K. Perspectives on cost and outcomes for point-of-care testing. Clin Lab Med. 2009;29(3):479-489. https://pubmed.ncbi.nlm.nih.gov/19840681/.
- Grieve R, Beech R, Vincent J, et al. Near patient testing in diabetes clinics: appraising the costs and outcomes. Health Technol Assess. 1999;3(15):1-74. https://pubmed.ncbi.nlm.nih.gov/10632625/.
- Health Quality Ontario. Point-of-Care Hemoglobin A1c Testing: OHTAC Recommendation. Ontario Health Technology Advisory Committee, June 2014.
http://www.hqontario.ca/Portals/0/Documents/evidence/reports/recommendation-poc-HbA1c-140731-en.pdf. - U.S. Preventive Services Task Force. Prediabetes and Type 2 Diabetes: Screening. August 24,2021. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/screening-for-prediabetes-and-type-2-diabetes.
- American Diabetes Association. 2 – Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes – 2022. Diabetes Care. 2002;45(Supplement 1):S17-S38. https://diabetesjournals.org/care/article/45/Supplement_1/S17/138925/2-Classification-and-Diagnosis-of-Diabetes.
- Twarog JP, et al. Difference in HbA1c% screening among U.S. adults diagnosed with diabetes: findings from the National Health and Nutrition examination Survey (NHANES). Prim Care Diabetes 2018; 12(6): 533-536. https://pubmed.ncbi.nlm.nih.gov/30049635/.
- Rowley WR, Bezold C, Arikan Y, et al. Diabetes 2030: Insights from yesterday, today, and future trends. Popul Health Manag. 2017;20(1):6-12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5278808/.
Read More
- A Case Of Late-Onset Diabetes
- Diabetes Mellitus: Current Diagnosis, Screening And Management Issues In Urgent Care
- Original Research: Early Diabetes Screening In The Urgent Care, Part 1
- Original Research: Early Diabetes Screening In The Urgent Care, Part 2
Download the article PDF: HbA1c as Screening/Diagnoses for Early or Asymptomatic Diabetes in the Urgent Care Facility

