Urgent message: Integration of various techniques when performing minor procedures on children can enhance clinical care for patients and families while bringing within reach administrative and financial goals.
Emory Petrack, MD, FAAP, FACEP, Lisa S. Perry, CCLS, and Kristine Vehar, RN As the practice of urgent care medicine continues to grow, urgent care centers grapple with several important issues, among them the needs to provide optimal clinical care, reduce medical legal risk, and deliver excellence in customer service; the latter is especially true when centers are located in competitive markets.
Although pediatric care in the urgent care setting has traditionally received relatively little emphasis, it is an area of focus whose time has come; spotlighting child and family centered care helps urgent care centers enhance clinical care for children and families while also bringing within reach administrative and financial goals.
A plethora of ways exists for enhancing care for families and children in urgent care settings. This article focuses on but one: improving care for children presenting in need of minor procedures, such as blood draws, IV placements, local wound care, and suturing.
While a variety of pharmacologic and non-pharmacologic techniques for enhancing such pediatric procedures are described in this paper, success in achieving broad care, satisfaction, and business goals is dependent upon the integration of techniques.
In other words, each technique alone presents certain benefits to urgent care centers and the children and families they treat, but it is the sum of techniques used together that creates synergy and paints a uniquely positive picture families remember and share with others in the community.
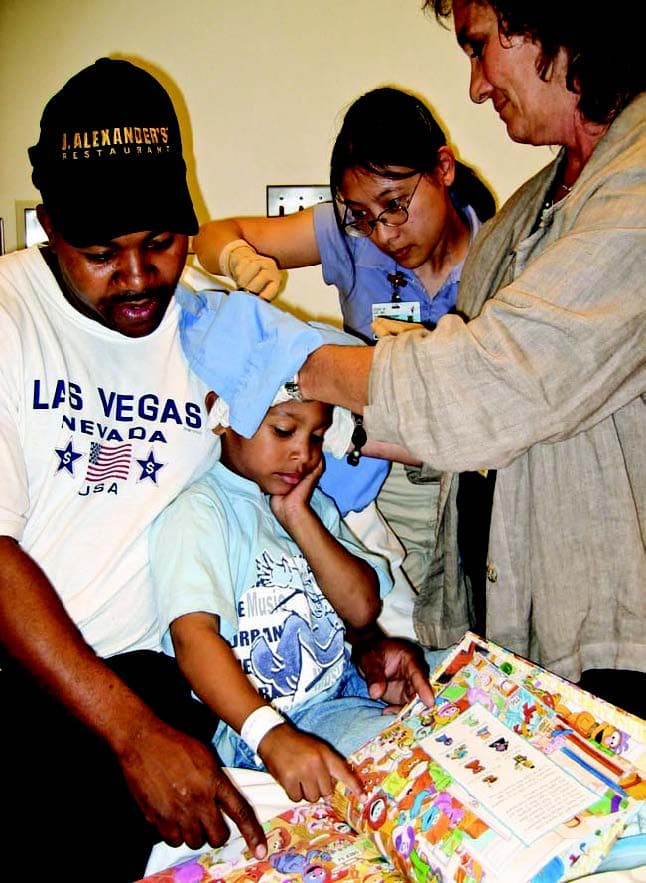
Figure 1, which shows a 4-year-old boy undergoing repair of a scalp laceration, is an example of what can be achieved when the techniques described here are success- fully integrated into an urgent care center’s repertoire.
This article will employ a case-based approach to explore a variety of techniques.
Pharmacologic Techniques
IV and Blood Draws
A 6-year-old presents to the urgent care center with sig- nificant vomiting and diarrhea, requiring IV rehydration. The child is awake and alert, but is very anxious about the need for an IV, as is the child’s mother. One method that has been around for several years is the application of a eutectic mixture of lidocaine and prilocaine (EMLA) or lidocaine topical (LMX) 4% cream, which is applied to intact skin to provide anesthesia before needle insertion. The challenge with such creams, however, is that EMLA takes about an hour to start working; LMX 4% takes 30 to 45 minutes. Frequently, parents do not want to wait, and using these creams significantly reduces throughput time in busy centers.
An alternative to creams is the 70 mg lidocaine/70 mg tetracaine topical (Synera) patch, which is impregnated with lidocaine and tetracaine. When the package is opened, the patch heats up to enhance its effectiveness. This patch is effective in 20 minutes, and is, therefore, much more useful in the emergency- and urgent care setting.
Figure 2 shows a 13-year-old girl, just seconds after an IV line placement. She was extremely anxious about the need for IV placement; the Synera patch and several nonpharmacologic techniques, dis- cussed later in this article, were used before placement.
Yet another alternative will be available in the near future: Zingo, produced by the pharmaceutical company Anesiva. Zingo is a device that delivers powderized lidocaine, which is injected into the epidermis with com- pressed air. Delivery is painless, and analgesia is achieved in one to three minutes. An important benefit of this method is that the analgesia becomes part of the procedure itself, not requiring significant additional time.
Although uncommon in the urgent care setting, the need to place an IV or draw blood in young infants does arise occasionally. Concentrated sucrose solution has been shown to reduce pain in infants less than 2 months old. A 24% sucrose and water solution (Sweet-Ease) is avail- able for this purpose. Placing 0.5 ml directly on the tongue one minute before the procedure leads to endogenous endorphin release and pain reduction. Offering a pacifier after the sucrose solution may help further soothe the infant.
Suturing
A 4-year-old comes to the urgent care center after running into the corner of a dresser. The child had no loss of consciousness, but did sustain a 2 cm laceration to the forehead. Although dermal glue is considered for closure, a decision is made to suture due to the wound’s depth and abraded edges. The family, naturally, is very concerned about how the child will handle the suturing.
Lidocaine-epinephrine-tetracaine (LET) gel is this author’s method of choice for lacerations requiring suturing, as it provides complete anesthesia for suturing in 30 minutes for approximately 60% to 80% of patients. In other children, it can reduce the pain of a subsequent lidocaine injection.
LET gel tends to work best on the scalp and face, but provides variable anesthesia in the extremities, as well. This treatment requires preparation by a pharmacist and is not commercially available. It is important to note that less-than-complete anesthesia may result from improper use.
For proper pain control, the gel is applied generously into the laceration. A small piece of cotton is also inserted and liberally saturated with additional gel. A small gauze pad is applied over the wound. After 30 minutes, the gauze and cotton are removed, and the wound can be tested for pain with a small gauge needle. Additional buffered lidocaine anesthesia may also be offered if needed.
Non-Pharmacologic Techniques
Establishing Trust
Urgent care centers have at their disposal a variety of non- pharmacologic techniques to improve the experience of children who require minor procedures. At the foundation of each technique is the establishment of trust with the child and family.
To children who are in pain or sick, being in an urgent care center is like being in a foreign country. They are un- familiar with the environment and do not understand what is happening and being said around them. When in such a state, children who need invasive procedures, especially if restrained, often “fight for their lives.” When this happens, physicians and other medical staff unwittingly contribute to potential psychological trauma that can lead to difficulties with future medical en- counters and procedures.
Some physicians and staff still prefer parents to step out of the room during a procedure. From the child’s perspective, this can be traumatic, as the child cannot understand why the parent would turn them over to a stranger who then causes pain and anxiety.
To the child, the parent is the foundation of all trusting relationships. It is almost always better to allow the parent to remain with the child at all times. Language and communication form the cornerstone on which trust is built. Urgent care professionals should address the child’s feelings honestly and ask if he or she is scared. The parent should be permitted to touch the child and to help him or her through the experience.
While nothing short of general anesthesia can guarantee that a child will not cry and become upset, techniques such as these may minimize the intensity and duration of crying, as well as the amount of restraint needed. Children learn to trust when they feel a sense of control. This is why, whenever possible, urgent care providers should allow children presenting for minor procedures the ability to choose among options.
Such options include the choice of position for older children, the choice to watch or look away, or the choice of distractions, discussed later in this article. Children may also be asked to help hold themselves still. A parent can play a supporting role by helping to hold or position the child. Staff can also acknowledge parental anxiety while helping parents calm down and focus on the needs of the child.
Positioning Techniques
Children are commonly restrained during minor proce- dures, as movement often leads to poor outcomes and even safety issues. However, children move less if they feel a sense of control and if restraint is used only as much as is absolutely necessary.
This is especially true if a parent does most of the holding. Using good positioning techniques can further reduce the need for papoose boards or other restraints. Infants can be positioned with the parent holding or partially holding them. Infants may also be placed on a stretcher, with the parent’s face right next to the infant’s face to provide comfort [Additional images, including one that illustrates this point, can be found at www.jucm.com.]. The infant may be offered a pacifier and the parent encouraged to speak to the child, as a parent’s voice can be very soothing. Parents may also be asked to pick up a baby immediately after a procedure for quick calming.
Ideally, toddlers should be sitting in the caregiver’s lap for procedures. Alternatively, child and parent may sit chest to chest, with the child’s arm extended on the table for IV placement or suturing of an extremity.
School-aged children can also sit comfortably in a parent’s lap. Children need less restraint if they are being held by someone they trust.
Teens and older children do best when given choices, enabling them to maintain as much control as possible.
Adolescents may be offered a choice of positions, such as sitting or lying down, and care should be taken to respect their privacy.
Preparation and Distraction Techniques
Once trust has been established and an appropriate positioning technique chosen, the child is prepared to cope during the actual procedure. Language alone can turn an experience from positive to negative very quickly.
For example, the phrase “don’t move” instantly evokes fear in children and creates unnecessary anxiety. A better choice of language might be “do your best to hold yourself still so I can help you better.”
For the best possible experience, children should be told what to do, rather than what not to do.
Words like “pinch” for IV placement, and “pressure” or “pushing” for sutures or staples are far less scary, and therefore far more comforting. The child should also know that although they will not feel pain during suturing, they will feel a sensation of pushing or pulling on the skin. If children really want to watch during a procedure, it is best to allow them to do so. Forcing children to look away increases anxiety and erodes the trust that has been established.
Children older than 3 or 4 should be told what will happen at each step before any action is performed, preferably by showing and telling what can be expected. Children may be shown the instruments and allowed to feel the suture material, which can be referred to as “string bandaids.”
A demonstration set of non-sterile equipment can be kept on hand for this purpose. If the child is too young to understand, a touch of the parent’s body where the laceration is located will encourage positive modeling in the child. Combining appropriate language with visualization of what will be happening leads to less anxiety on the part of both patient and caregiver.
For intravenous placement, it helps to refer to the IV as a “straw” through which fluids and medicines can be given. Children may also be comforted in the knowledge that by using the straw, no further needles will be needed later. The needle can be referred to as a “helper” to get the straw under the skin into the vein. Providers can also demonstrate how the tourniquet is used and how the area is cleaned before it is actually done. Once the child is appropriately prepared for the procedure, distraction techniques can further improve the experience as the procedure is accomplished.
While several modalities exist for different developmental ages, it is important to understand that no technique will be as effective if the preceding methods are not adequately applied. Establishing trust, choosing the best position, and preparing the child for the procedure creates the foundation for the consistent and effective use of later distraction techniques.
Bubble bowing is an excellent distraction technique for children 3 years of age and older who are undergoing a procedure. Older children may be asked if they prefer to blow away the pinch of an IV into the air—or into the bubbles. This technique gives the child choice and control and helps them to develop better coping skills. Alternatively, the child could squeeze a parent’s hand or a rubber ball to focus their energy elsewhere and enhance distraction.
Reading developmentally appropriate books is an excellent distraction for children undergoing minor procedures.
Likewise, with an inexpensive CD player and head- phones, different kinds of music appropriate for different developmental ages can also be made available.
Storytelling is another distraction alternative, one in which parents can often be counted on to participate.
Simple toys also work to distract younger children through play. The key to successful distraction is to engage the patient and/or caregiver in choosing the best technique for each individual child.
Integration of Pharmacologic and Non-pharmacologic Techniques
Pharmacologic and non-pharmacologic techniques can each be used to improve the experience of children requiring minor procedures in the urgent care setting. The real power, however, comes when the provider is able to fully integrate these seemingly diverse approaches.
Most providers are familiar with the pharmacologic approach. It makes sense to start a discussion with a parent and older child about pharmacologic options. Providers should consider using some of the newer options, such as the Synera patch for IV placement. LET gel, while not necessarily eliminating the need for lidocaine infiltration, works very well when used correctly, and should always be considered for laceration repair.
Once a decision is made about which pharmacologic agent to use, the provider should consider how the agent will be integrated with non-pharmacologic techniques. This decision is based on the specific procedure, the de- velopmental age of the child, and discussions with the child and/or caregiver.
Typically, it takes less than five to 10 minutes to estab- lish trust, decide how to best position the child, prepare the child, and incorporate a distraction technique into the procedure. This is time well spent, and will result in much better experience for both the child and the family.
Summary
The reality is that few urgent care centers focus on the specific needs of children; even fewer do so well and consistently. The good news is that clinical care can be significantly enhanced by paying attention to the needs of children requiring minor procedures.
In addition, as families in the community learn that a specific urgent care center attends well to the needs of children and families, word will spread. Thus, enhancing care for children is an excellent business practice and marketing strategy in competitive markets.
Suggested Readings
- Sinha M, Christopher NC, Fenn R, et Evaluation of nonpharmacologic methods of pain and anxiety management for laceration repair in the pediatric emergency department. Pediatrics. 2006;117:1162- 1168.
- Child life services (Policy Statement). Pediatrics. 2006;118:1757-1763.
- Stevenson MD, Bivins CM, O’Brien K, et Child life intervention during angiocatheter insertion in the pediatric emergency department. Pediatr Emerg Care. 2005;21:712-718.
- Child life services can provide competitive ED Management. 2004;16(10):115-117.
- Magaret ND, Clark TA, Warden CR, et Patient satisfaction in the emergency department a survey of pediatric patients and their parents. Acad Emerg Med. 2002;9:1379-1388.
- Petrack EM, Christopher N, Kriwinsky Pediatric pain management in the emergency department: Patterns of analgesic utilization. Pediatrics. 1997;99:711-714.



