Published on
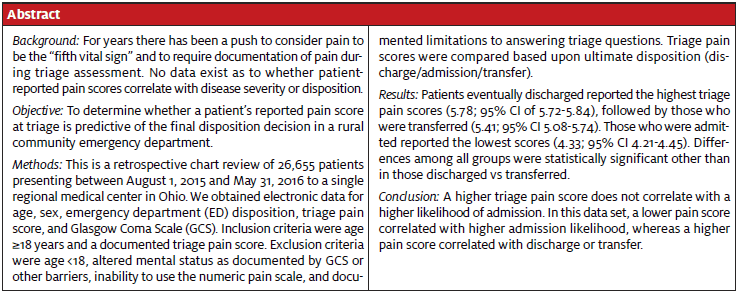
Urgent message: Efforts to have pain declared a “fifth vital” sign began nearly 25 years ago. Since then, several national accrediting and governmental agencies have taken up the cause of viewing pain as a distinct problem to be addressed as such. However, few data relevant to emergency and urgent care presentations exist.
Mark Pruitt, DO, Ya Wen, DO, Michael Pallaci, DO, and Godwin Dogbey, PhD
INTRODUCTION
Traditionally, there have been four vital signs: temperature, heart rate, respiratory rate, and blood pressure.1 Attempts to include pain as a fifth vital sign were first undertaken by American Pain Society President Dr. James Campbell in 1996. He stated, “Vital signs are taken seriously. If pain were assessed with the same zeal as other vital signs are, it would have a much better chance of being treated properly. We need to train doctors and nurses to treat pain as a vital sign. Quality care means that pain is measured and treated.”2 In 1999, the Department of Veteran Affairs instituted the Pain as the 5th Vital Sign Toolkit,3 which recommended aggressive pain screening and treatment, viewing pain as a vital sign.
In 2000, the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) began to require pain assessment and treatment as a condition for accreditation.4,5 A study published in 2007 on pain management in the Annals of Emergency Medicine recommended assessing pain with the initial vital signs and implementing immediate treatment, including using opiates, based on the pain score reported.6 Numerous articles, standards, and studies conclude that it is best practice to assess and manage pain; however, there is lack of evidence to indicate implication of physiologic process as with the other traditional vital signs.2-6
Traditional vital signs (temperature, heart rate, respiratory rate and blood pressure) are measurements of basic bodily functions.1 Deviations from normal ranges for these measures have been shown in multiple studies to have a direct association with hospital admission rates, ICU admissions, and mortality.7-10 Patients with documented abnormal traditional vital signs in the ED are four times more likely to be admitted than those with normal vital signs.7 Respiratory rate has been shown to be a predictor for cardiopulmonary arrest in admitted patients.8 In one study, tachypnea with a respiratory rate of 25-29 breaths per minute correlated with a 21% mortality, with mortality increasing as respiratory rate increased.9 The strongest predictor for ICU admission and hospital mortality from ED triage is not the presenting complaint, but abnormal vital signs.10
An increased emphasis on the recognition and treatment of pain has led some to recommend that a numerical rating of pain provided by the patient be added as a fifth vital sign. While the desirability of recognizing and relieving pain is intuitive and obvious, it is less clear whether the presence or severity of pain is correlated with patient outcomes or disposition, as has been proven for abnormal traditional vital signs.
Our literature search revealed no publications relating the presence or severity of pain to hospital admission, discharge, or transfer. Such a correlation would make a strong case that the importance of pain measurement is on par with the measurement of temperature, heart rate, respiratory rate, and blood pressure.
The goal of this study is to determine whether the reported pain score at the time of ED triage is predictive of hospital admission or transfer.7-10
MATERIALS AND METHODS
An exemption was approved by the Adena Health System Institutional Review Board (IRB), approval #16-02-001.
2.1 Study Population
The population included patients presenting to our rural regional medical center ED from August 1, 2015 to May 31, 2016. Inclusion criteria were age ≥18 years and a documented triage pain score. Exclusion criteria were age <18, altered mental status (AMS) as documented by Glasgow Coma Score (GCS) or impaired cognition, inability to use the numeric pain scale, and documented limitations to answering triage questions. Records without documented pain score or disposition were excluded. There were 26,665 patients who were at least 18 years of age who presented to our ED during this time period. Of these, 15,706 met inclusion criteria and were included in the data analysis.
2.2 Study Design
This study was a retrospective chart review. Data were extracted from the electronic medical record (EMR) by an employee of the information technology department (IT), and imported into a Microsoft Excel spreadsheet without patient identifiers. The IT employee was blinded to the intent of the study. Data were imported into the spreadsheet for each patient included their age, sex, ultimate disposition (discharge/admit/transfer), numerical pain score (conventional 0-10 scale), GCS, and whether barriers to communication were documented by nursing. The data were analyzed by the third author.
Our initial goal was a sample size of at least 160 patients to reach our desired statistical power of 0.8 to detect moderate differences in pain scores among the groups with a statistical significance of p<0.05. The final number of patients studied was 15,706.
2.3 Data Analysis
A one-way ANOVA was used to examine the question of statistical difference in disposition with the mean pain scales. A Games-Howell Post Hoc Test served to further determine which pairs of disposition differed with statistical significance. These statistical tests were also used for age group analysis to determine statistical significance of mean pain scales among various age groups. Levene’s test showed that the homogeneity of variance assumption was met (p<0.05) for age group analysis.
RESULTS
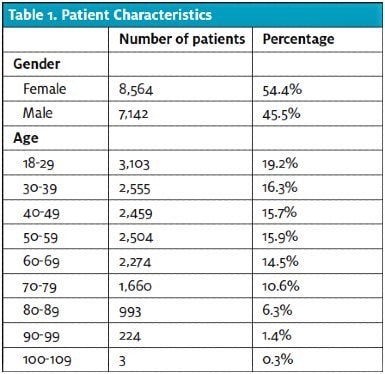
A total of 15,706 patients were included in this study. Their age and gender resemble the national population of ED patients per the 2015 National Hospital Ambulatory Medical Care Survey conducted by the Centers for Disease Control and Prevention,11 with a slightly older population in this study (Table 1). The disposition rates in this patient population were similar to other EDs in the U.S.11 and to the overall population at this facility (Table 2).
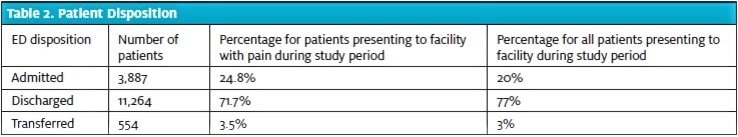
A large proportion of patients (76.6%) reported some level of pain, with most of those (64.0% of all patients; 83.6% of those with pain) reporting a pain score of 5 or greater (Table 3). For each of the three final disposition decisions, the mean pain score was calculated with its respective standard deviation, and a 95% confidence interval using one-way ANOVA (Figure 1). One patient was not included in the calculations due to incomplete data (unable to determine final ED disposition).
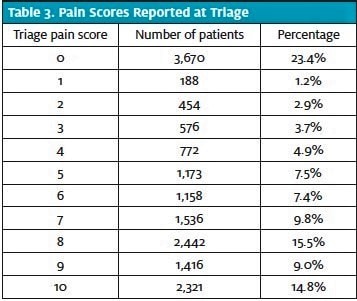
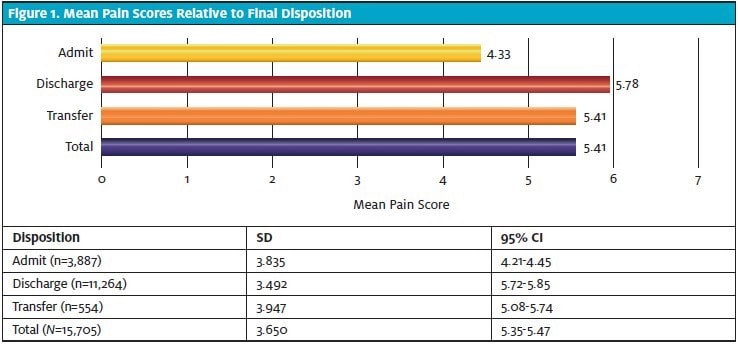
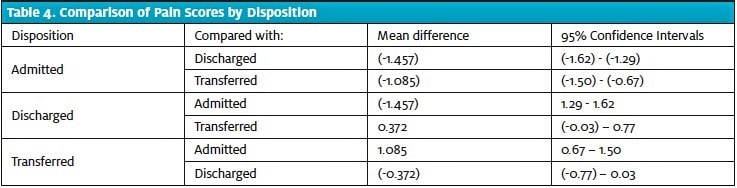
The mean pain score was found to be lowest in the admitted group (4.33; 95% CI 4.21-4.45), and highest in the discharged group (5.78; 95% CI 5.72-5.85). There were statistically significantly lower triage pain scores in patients who were admitted compared with those who were discharged and those who were transferred (Table 4). Pain scores were also lower in transferred patients than in discharged patients, although this difference fell just short of statistical significance.
DISCUSSION
Pain scale ratings are based on the Numeric Rating Scale (NRS) which quantifies each patient’s level of pain on a scale of 0-10.3 The goal of this study was to determine if a higher pain scale rating predicted the final disposition of admission or transfer, indicating a higher acuity.
The pendulum has swung wildly over the last few decades in relation to the approach to pain management in the ED. Oligoanalgesia in the ED was first suggested to be a widespread problem in the 1980s,12 and was talked and written about extensively throughout the 1990s, 2000s, and into the early 2010s.[6,13-15] Around that time, the prevalence of oligoanalgesia began to come into question.16 And with the advent of the opioid epidemic in the U.S. over the last 5-10 years, the emphasis of the conversation has shifted from undertreatment of pain in the ED to overtreatment with opioids.17-19
While embraced enthusiastically by some, the emphasis on the impact of ED analgesic prescribing has been met with skepticism by others. In 2018, Axeen and colleagues reported a 471% increase in the amount of opioids prescribed from 1996 to 2012. However, ED prescriptions accounted for only 4.4% of the opioids prescribed, down from 7.4% in 1996,20 suggesting a modest impact on the epidemic from ED prescribing.
Pain is one of the most common reasons for patients to present to the ED for treatment.22 Thoughtful practitioners can come to very different conclusions on how best to stem the tide of the opioid epidemic while agreeing that providing analgesia, whether with opioid, nonopioid, or nonpharmacologic therapies, is an important aspect of delivering quality, compassionate emergency care. Evidence suggests that ED providers still err on the side of prescribing analgesics for their patients in pain; Singer, et al reported in 2008 that among patients who reported pain in the ED (76.6% in our study), only 51% desired analgesics. Of those who desired them, 81% received them, in addition to 34% of patients who didn’t desire them.14
The intent of adding pain as a fifth vital sign is to emphasize the importance of its recognition and treatment. However, there is also potential for unintended negative consequences. Including a measure that is not proven to reflect disease severity among a group of measures that have reflected disease severity could lead to an overemphasis on the urgency of addressing pain relative to addressing a critical and emergent measure such as hypotension. Conversely, it could lead to a negative effect on the perceived urgency of other vital sign abnormalities if they are lumped together with the pain score.
Examples of this in medicine abound, from defining sepsis based on the nonspecific Systemic Inflammatory Response Syndrome (SIRS) criteria21 that led some practitioners to de-emphasize the importance of “sepsis” due to the number of nonsick patients caught by the excessively wide net of the SIRS criteria, to composite endpoints in trials that include outcomes ranging from death to the inconsequential. The traditional teaching of “vital signs are vital” may prove unreliable if one of the vital signs does not correlate with disease severity or patient outcomes. In addition, referring to pain as a vital sign insinuates a need for prompt action, which could be perceived as a need for opioid analgesics. Considering Singer’s data above, the ongoing opioid crisis, and the side-effect profile of opioids, being overly aggressive based on the emphasis of pain as a vital sign is likely to cause at least some level of harm, possibly more than the intended benefit.
An abnormality in vital signs (temperature, heart rate, respiratory rate and blood pressure) correlates with a fourfold increase in the probability of admission.7 The results of this study did not yield the same results for the pain score, and our search of the literature found no evidence to indicate correlation with disease severity or outcomes. In this study, patients who were discharged had the highest mean pain score, while those who were admitted had the lowest. Thus, a higher pain score did not indicate a higher likelihood of admission or transfer. Instead, a higher pain score was associated with a higher likelihood of discharge and, counterintuitively, lower disease severity.
4.1 Limitations
There are several limitations to this study. While there is emphasis on attempts to place an objective measure on pain, it is well known that pain is a subjective experience, and two patients with an identical condition are likely to score their pain differently. In our retrospective data collection, we did not quantify/account for those with multiple visits or psychiatric-related complaints. We also did not account for those who had self-medicated or received analgesics per EMS prior to arrival, or those who were on chronic analgesic therapy at home. In addition, the data were analyzed using a one-way ANOVA, which is most reliable when data fit a standard normal distribution; however, the pain data approximated, but was not perfectly normally distributed.
While our study focused on admission rates in assessing disease severity, there are multiple other outcomes that could be used as markers of disease severity.
We also did not account for variances in pain scores among patients with similar presentations. For example, patients with fractures may rate their pain more highly than patients with chest pain, which would not necessarily make them more likely to be admitted or to suffer a bad outcome. However, it is possible that the severity of pain among patients presenting specifically with chest pain or specifically with fractures could reflect disease severity. In addition, patients with certain high-risk complaints such as altered mental status would be more likely to be admitted or transferred, and would also be more likely to be excluded than discharged patients due to the inability to record their pain score.
Furthermore, this study was conducted at a single facility in a rural community with one of the highest rates of opioid abuse in the U.S., which sees a limited number of trauma patients and a disproportionately large number of patients who are uninsured. It is also possible that older people, who presented in slightly higher numbers in our population than the national average, may have a higher frequency of admission due to multiple comorbidities, but may report a lower level of pain due to cultural and generational norms. Similarly, the community in which the study was conducted is disproportionately Caucasian. These factors may limit the external validity of our findings. We could not account for treatment variability among providers and the possible subsequent effect on disposition. We also did not account for patients who may have “bounced back” on this visit or at a later time with a higher acuity.
CONCLUSION
In this study, self-reported pain, unlike traditional vital signs, does not appear to predict more serious illness or to predict emergency department disposition.
References
- Vital Signs, Anthropometric Data, and Pain. In: LeBlond RF, Brown DD, Suneja M, Szot JF, eds. DeGowin’s Diagnostic Examination. 10th New York, NY: McGraw-Hill; 2014.
- Campbell J. APS 1995 Presidential Address. Pain Forum. 1996;5:85-88.
- Pain: The Fifth Vital Sign. Department of Veterans Affairs. October 2000. Available at: http://www.va.gov/PAINMANAGEMENT/docs/Pain_As_the_5th_Vital_Sign_Toolkit.pdf. Accessed March 7, 2020.
- The Joint Commission. Clarification of the pain management standard. joint commission perspectives. 2014;34:11.
- The American Pain Society 2006. Pain: Current Understanding of Assessment, Management, and Treatments. Available at: http://americanpainsociety.org/uploads/education/npc.pdf.
- Decosterd I, Hugli O, Tamches E, et al. Oligoanalgesia in the emergency department: short-term beneficial effects of an educational program on acute pain. Ann Emerg Med. 2007;50:462-471.
- Mehmood A, He S, Zafar W, et al. How vital are the vital signs? A multi-center observational study from emergency departments of Pakistan. BMC Emerg Med. 2015;15(Suppl2):S10.
- Fieselmann J, Hendryx M, Helms C, et al. Respiratory rate predicts cardiopulmonary arrest for internal medicine inpatients. J Gen Intern Med. 1993;8:354-360.
- Goldhill D, McNarry A, Mandersloot G, et al. A physiologically-based early warning score for ward patients: the association between score and outcome. Anaesthesia. 2005;60:547-553.
- Barfod C, Lauritzen M, Danker J, et al. Abnormal vital signs are strong predictors for intensive care unit admission and in-hospital mortality in adults triaged in the emergency department – a prospective cohort study. Scand J Trauma Resusc Emerg Med. 2012;20:28.
- Rui P, Kang K. National Hospital Ambulatory Medical Care Survey: 2015 Emergency Department Summary Tables. Available at: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2015_ed_web_tables.pdf. Accessed March 7, 2020.
- Wilson JE, Pendleton JM. Oligoanalgesia in the emergency department. Am J Emerg Med. 1989;7:620-623.
- Knox HT. Are patients in the emergency department adequately treated for pain? Medscape. January 23, 2009. Available at: https://www.medscape.com/viewarticle/586872. Accessed March 7, 2020.
- Singer AJ, Garra G, Choban JK, et al. Triage pain scores and the desire for and use of analgesics. Ann Emerg Med. 2008;52:689-695.
- Albrecht E, Taffe P, Yersin B, et al. Undertreatment of acute pain (oligoanalgesia) and medical practice variation in prehospital analgesia of adult trauma patients: a 10 yr retrospective study. Br J Anaesth. 2013;110:96-106.
- Green SM. there is oligo-evidence for oligoanalgesia. Ann Emerg Med. 2012;60:212-214.
- Bukata R. Opiate misuse vs. oligoanalgesia. Medium. Available at: https://medium.com/@emabstracts/opiate-misuse-vs-oligoanalgesia-30ed47936ba2. Accessed March 7, 2020.
- Baruch J, Springs S. Opioids and pain in the emergency department: a narrative crisis. Medl Humanit. 2018;44:213-216.
- Perrone J, Nelson LS, Yealy DM. Choosing analgesics wisely: what we know (and still need to know) about long-term consequences of opioids. Ann Emerg Med. 2015;65:500-502.
- Axeen S, Seabury SA, Menchine M. Emergency department contribution to the prescription opioid epidemic. Ann Emerg Med. 2018;71:659-667.
- Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801-810.
- Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2017 Emergency Department Summary Tables. Available at: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2017_ed_web_tables-508.pdf. Accessed March 7, 2020.
Mark Pruitt, DO and Ya Wen, DO are graduates of the Adena Health System Residency Program. Michael Pallaci, DO is program director and core faculty, Emergency Medicine Residency, ARMC, at Adena Health System. Godwin Dogbey, PhD is CORE biostatistician, CORE Research Office, Ohio University Heritage College of Osteopathic Medicine. The authors have no relevant financial relationships with any commercial interests.
