Published on
Urgent message: As the cause of approximately 10 million office visits in the United States annually, vulvovaginitis remains a common but important complaint seen in the urgent care setting.
Jansen Tiongson, MD, Samuel Keim, MD, and Peter Rosen, MD
Although numerous etiologies account for vulvovaginitis, the vast majority of cases are due to bacterial vaginosis (BV), trichomoniasis, and vulvovaginal candidiasis (VVC). BV causes 40% to 50% of all cases, while candidiasis and trichomoniasis account for 20% to 25% and 15%-20%, respectively. Other notable causes, such as atrophic/contact vaginitis and sexually transmitted diseases, are beyond the scope of this review. This article presents a review of practical concepts of evaluation and management along with supportive data from current literature about the three main causes.
Pathophysiology
The moist vaginal environment promotes the growth of various organisms. However, a balance between different organisms ordinarily prevents the growth of pathogens.
Lactobacillus, the predominant bacteria found in the vagina, produces glycogen that is broken down to form lactic and acetic acids, thus favoring the growth of normal flora over pathogens by maintaining a pH of 4-5.
Normal flora produce normal vaginal secretions that range from being watery thin to a whitish thick dis- charge. The disruption of the normal balance in the microflora of the vagina leads to the symptomology ascribed to vulvovaginitis.
Women often present with varying signs and symptoms, including vaginal dis- charge, malodor, irritation, and itch. Often, urgent care physicians can narrow down the differential diagnosis (Table 1) based on the descriptions provided by patients. Systemic illnesses, antibiotic use, diet, immuno suppression, and sexual practices can disrupt the normal balance in the vaginal flora, and often precipitate vulvovaginitis.
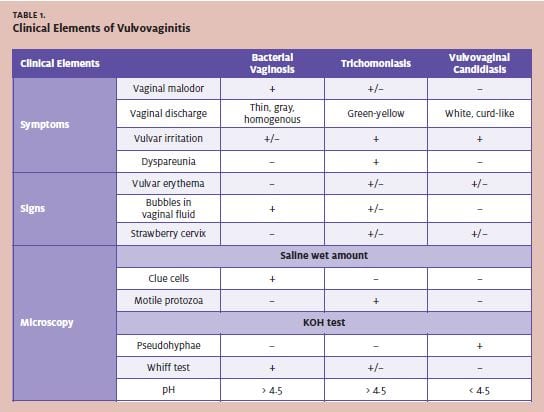
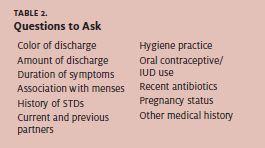
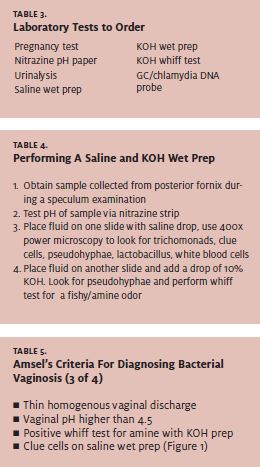
Table 2 outlines the general questions to ask during a history and physical examination, while Table 3 lists laboratory tests most helpful to diagnose the specific etiology of vulvovaginitis. Table 4 describes how to perform the wet preparation and 10% potassium hydroxide (KOH) tests. Note that the wet mount is 80%-90% sensitive for diagnosing BV, 62% for trichomoniasis, and 22% for VVC. 5
Bacterial Vaginosis
Epidemiology Bacterial vaginosis, caused by the overgrowth of Gardnerella vaginalis, Mycoplasma hominis, and other pathogenic bacteria with deprivation of Lactobacillus, affects nearly 5% of college women and 60% of those with sexually transmitted diseases. There is an increased prevalence among divorced women over the age of 30.1 Many risk factors predispose a patient to BV. For example, an increased number of sexual partners in the prior three months, along with a history of STDs, compound the risk of developing BV.3
Furthermore, habits such as vaginal douching at least once a week are associated with increased risk, suggesting that daily habits play an important role in the development of BV. Oral contraceptives and IUDs not only diminish the risk of pregnancy but provide protective factors against BV.2,3 BV occurs more often in black Caribbean women and among women of lower socioeconomic status.4
Presentation and Diagnosis
The diagnosis of BV has been classically defined by Amsel’s clinical criteria (Table 5). Amsel’s criteria include both clinical signs and symptoms and laboratory findings. These criteria have been shown to be 92% sensitive in diagnosing BV. Vaginal pH has the highest sensitivity while a positive whiff test is most specific, although a false positive can be seen with trichomoniasis.5
Anderson, et al report that the presence of a malodorous vaginal discharge indicates high likelihood of BV, while its absence essentially rules out the diagnosis. Furthermore, moderate- to copious thin gray homogenous discharge increases the likelihood ratio (LR) from to 14, while normal-to-mild whitish discharge lowers the LR of BV to 11.
The study also points out the following percentages of having BV per symptomology:
- 64% with thin gray homogenous vaginal discharge
- 53% changes in discharge compared to normal
- 32% pruritus
Finally, the absence or scant presence of Lactobacillus in addition to the presence of clue cells under microscopy raises the likelihood of BV, while normal levels of the normal flora significantly drop the LR to 0.021 (Table 1).
Treatment
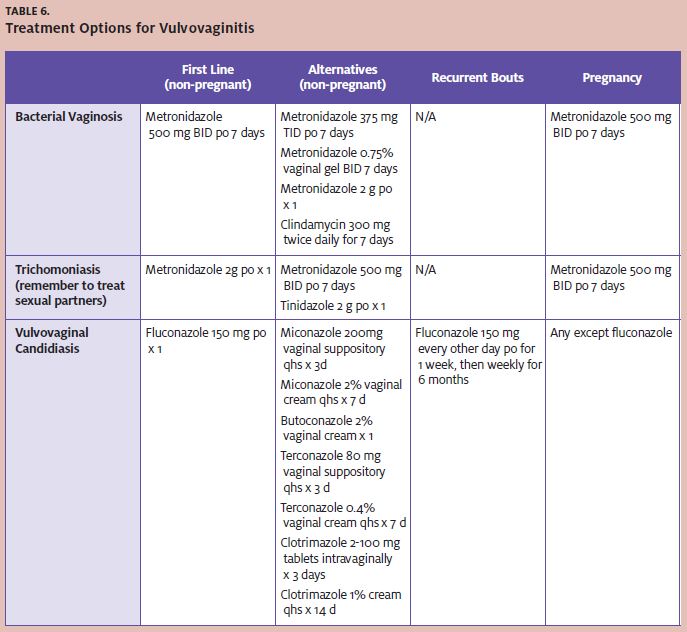
The World Health Organization recommends metronidazole as the first-line therapy for the treatment of BV (Table 6). Metronidazole 500 mg twice daily for seven days has been the common therapy. Some have recommended a one-time 2 g dose of metronidazole. A ran- domized clinical trial reported in 2000, however, showed that the one-time 2 g regimen is only 75% efficacious compared with the week-long 500 mg regimen, which has an efficacy rate of 85%-90%.
Finally, the alternative dosing of 375 mg three times daily has the same efficiency as the 500 mg dose, with fewer of the gastrointestinal side effects commonly associated with the use of metronidazole.
However, the compliance of a three times vs. twice daily regimen may not be as good rupture of membranes, spontaneous abortions, chorioamnioni- tis, post-partum endometritis and post-Caesarean section wound infection. As mentioned above, 500 mg orally twice daily for seven days of metronidazole has been recommended for the treatment of BV in pregnancy. At present, metronidazole is considered safe to use during pregnancy. While there may be a possible association of premature birth and con- genital hydrocephalus, a consensus has not been determined to show the link between metronidazole and complications in pregnancy.8-10
Vulvovaginal Candidiasis
Epidemiology
As the second most common cause of vulvovaginitis, vulvovaginal candidiasis (VVC) affects nearly every three out of four women sometime during their lifetime. Furthermore, nearly 10% of women will experience repeated attacks without any obvious precipitating factors. Ninety percent of cases are due to Candida albicans, but other Candida species, such as glabrata and tropicalis, have been implicated with VVC. Major risk factors in the development of VVC include previous history of VVC, recent utilization of broad-spectrum antibiotics, diabetes mellitus, AIDS, and the use of immunosuppressive therapies.11,12
Presentation and Diagnosis
Much like other causes of vulvovaginitis, VVC patients present with a vaginal discharge, which in candidiasis is often described as cheesy, curd-like, and thick (Table 1). The occurrence of such a discharge makes it more likely to be VVC when compared to a watery discharge. Furthermore, the presence of vulvar itching increases the likelihood of VVC (LR of 1.4-3.3), compared with its absence.
In contrast to trichomoniasis and BV, the presence of malodor decreases the probability of diagnosis of VVC (LR 0.35). Lack of odor is consistent with candidiasis. Also, unlike the other causes of vulvovaginitis, women often can self-diagnose VVC due to its classical symptomology, which shows the greatest likelihood (LR 3.5) of having VVC based on history alone in studies reviewed.
Physical examination findings often include an erythematous vulva and vagina and a normal cervix upon speculum examination. The presence of both the erythema and curd-like discharge supports the diagnosis of VVC.1
With the utilization of wet saline and KOH prep, the diagnosis of VVC can be rapid and accurate under microscopy. The presence of the branching pseudohyphae, along with a normal pH of 4-5 with nitrazine paper, has a sensitivity of 38%-83%. The absence of pseudohyphae on microscopy, therefore, does not exclude the diagnosis. Often, VVC is diagnosed clinically. A Gram’s stain and Sabouraud’s agar culture both reach nearly 100% in sensitivity, but the logistic impracticality of these tests often negates their utilization in the urgent care setting.13
Treatment
A single dose of oral 150 mg fluconazole is clinically and microbiologically efficacious in the treatment of VVC (Table 6). Fluconazole is also the recommended therapy for recurrent attacks in the following regimen: 150 mg every other day for three doses followed by weekly 150 mg doses for six months. This therapy is effective in more than 80% of women who experience recurrent bouts of VVC.14
Alternatively, numerous intravaginal topical agents are available both over the counter and by prescription. These agents include imidazoles (clotrimazole, miconazole, and terconazole) and nystatin. A recent Cochrane database systematic review study reports that no statistical difference exists between the cure rates when com- paring oral versus an intravaginal topical agent. However, the study also notes that oral administration remains the preferred route in non-pregnant women due to safety, cost, and patient treatment preference. Pregnant patients are advised to use the topical agents for seven days rather than oral medication, as the imidazole topical agents have been shown to have a cure rate of 85%-100% in pregnancy while oral drugs such as fluconazole can be associated with GI intolerance, rash, and headache.15 Despite repeated use in some patients, utilization of fluconazole and the various imidazoles (clotrimazole, miconazole, and ketoconazole), fungal resistance is rare with only 3.7%-5.7% resistance shown in a study published in 2005.16 Boric acid suppositories may be as effective oral itraconazole in treating both acute and recurrent disease.17
Trichomonas Vulvovaginitis
Epidemiology
With nearly 120-180 million women affected annually worldwide, trichomoniasis remains a common cause of vulvovaginitis.18,19 Classified as an STD, Tri- chomonas vaginalis typically is a coinfection with other venereal disease, especially gonorrhea and chlamydia.
Laboratory testing for other STDs, therefore, remains part of the recommended workup in vulvovaginitis. Furthermore, its status as an STD increases its occurrence among premenopausal women, with a prevalence of 2.3% and 4% in 18-24-year-olds and 4% in those 25 and older. This disease can go undetected for months, and while the efficacy of treatment remains high, re-infection remains very common.
Unlike other major causes of vulvovaginitis, the prevalence of trichomoniasis seems to be associated with ethnicity: prevalence is highest in blacks (6.9%) and lowest among Caucasians (1.2%).20,21
Presentation and Diagnosis
Like the other major causes of vulvovaginitis, trichomoniasis often presents with a vaginal discharge (Table 1). It is often described as a yellow-gray-green-frothy secretion with an unpleasant odor. Having a yellowish dis- charge, as opposed to other colors, makes trichomoniasis 14 times more likely to be the diagnosis. Similarly, only 10% will present with frothy discharge. However, a recent study showed that only 42% of infected women presented with the discharge noted above. Other symptoms suggesting trichomoniasis include malodor and symptoms worse after menses. Unfortunately, 50% of women will not present with malodor, but in the cases that do, the whiff test performed under KOH prep can be a false positive.
With regard to physical examination, the most specific sign of trichomoniasis is colpitis macularis, or strawberry cervix. Described as punctuated hemorrhages with occasional vesicles or papules, this finding is rarely detected without colposcopy, and is seen in only 22%- 37% of women.1
Laboratory examinations include pH testing and wet saline/KOH preparations. Speculum samples will pres- ent with a pH >4.5 as well as findings of flagellated organisms under a wet saline mount. The sample should be read under a slide within 20 minutes of preparation to avoid deterioration of the protozoa. This method of confirming Trichomonas is only 40%-60% sensitive; thus, the absence of the protozoa under microscopy does not necessarily rule out the disease.
More sensitive and specific to diagnosing trichomoniasis is the latex agglutination test. A Trichomonas antibody or antigen, attached to latex beads, is mixed with the speculum sample. If the protozoan reacts with the latex bead complex, then an agglutination reaction occurs. Results are available within 10 minutes to an hour. This test is 98.8% sensitive and 92.1% specific compared with a wet mount preparation.
However, the cost and availability of this examination limits its use in the urgent care setting. For better sensitivity and specificity, a XenoStrip-Tv for T vaginalis test can be performed. However, this test is limited due to length, and its utilization in the urgent care set- ting is presently impractical.22
Treatment
The Centers for Disease Control and Prevention recommends a single dose of 2 g of metronidazole (Table 6). Unlike the treatment for BV, this regimen has a greater cure rate—90%-95%—compared with the week-long treatment of either 250 mg TID or 375 mg BID of metronidazole. The use of a single-dose therapy in the treatment of trichomoniasis increases compliance, and still provides cures. Treatment of the partner with the same regimen is recommended, although further re- search should focus on developing effective partner treatment strategy.18
Although the association of preterm labor and premature rupture of membranes is significantly lower than that seen with BV, treatment with metronidazole effectively eliminates such risks during pregnancy in relation to trichomoniasis.23
Of note, although resistance to metronidazole still remains uncommon, other azoles such as tinidazole and clotrimazole cream when used topically in a seven-day course have been proven to be effective alternatives.24
Summary
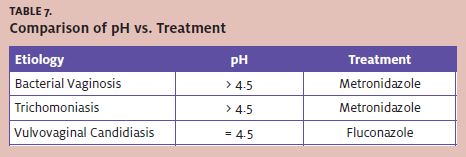
Vulvovaginitis is common in the urgent care setting. Affected patients will present with varying degrees of vaginal discharges and odors. After a history and physical examination, adjunctive tests such as wet preparations, microscopy, pH, and whiff tests can easily aid in differentiating between the three main etiologies of vulvovaginitis. Although laboratory tests can confirm the diagnosis, the clinical signs and symptoms are often accurate enough for diagnosis. One simple strategy is shown in Table 7.
Special considerations must be taken with pregnant patients. When treated appropriately, vulvovaginitis of- ten resolves without any sequelae in the majority of women.
A similar efficacy can be expected with the 0.75% metronidazole vaginal gel used twice daily. The gel eliminates BV at a rate of 83.7% after a two-week course. Fewer GI symptoms are reported with the use of the gel. A patient’s menstruation status does not change the effectiveness of the treatment. The vaginal gel, therefore, is an attractive alternative for treatment of BV.6 The oral week-long formulation is still highly recommended in pregnant patients.7 Clindamycin 300 mg twice daily for seven days can also be used alternatively for those intolerant of metronidazole.


