Urgent message: The urgent care provider’s most critical role in heat illness is to identify risk factors and the cause, to cool and hydrate the patient, assess for complications, and educate the patient in the hope of preventing a more serious exposure.
Bridget Dyer, MD, Samuel Keim, MD, and Peter Rosen, MD
Heat illness occurs when external heat conditions and internal heat production overwhelm the ability of the body to dissipate heat. Evaporation of sweat is the most effective way to dissipate heat; when the humidity is high, evaporation is compromised. Calculations that are based on both temperature and humidity, such as the heat index, are a more robust way of determining heat stress than ambient temperature alone.1 Elevated humidity can cause even moderate temperatures to be dangerous, especially to persons at high risk.
Internal heat production depends on both the level of exertion and the physiologic characteristics of the patient. In the average adult, exertion can raise the basal metabolic rate from 100 kcal/hr to more than 1000 kcal/hr, 70% to 100% of which is released as heat.2
Physiology
As the core temperature exceeds the hypothalamic set point, heat avoidance behavior is induced, and both sympathetic and parasympathetic tones are augmented.
Increased sympathetic tone increases cardiac output, supporting cutaneous and skeletal muscle vasodilatation, allowing for radiation of heat, delivering plasma for sweat and oxygen for exertion, with contraction of splanchnic circulation.
Parasympathetic tone modulates sweating, increasing to 2.5 liters per hour in an acclimated person during strenuous exercise.3 Heat shock proteins (HSP) act as molecular chaperones that prevent denaturing of other proteins at higher temperatures. Initial heat stress triggers increase HSP expression, which protects cells from a second heat exposure.4
Any process or comorbidity that interferes with cardiac output, vasodilatation, sweating or sweat evaporation, electrolyte balance, or normal behavioral response can impair temperature homeostasis.
Acclimatization requires one hour daily of moderate exercise for 10 to 14 days in conditions of heat stress.5 Acclimatized persons have increased sweat gland numbers, sweat volume, and salt reabsorption, leading to enhanced ability to dissipate heat by evaporation, reduced hyponatremia, and increased total body water (TBW). Increased TBW allows increased cardiac output.
Dehydration causes a reduction in available cardiac output, and greatly reduces the benefits of acclimitization.3
Epidemiology
Heat illnesses are a growing concern. It is estimated that there are 60,000 presentations for heat-related illness a year in the U.S., with an average of 688 deaths per year.6,7 This figure does not include the deaths of undocumented migrants crossing the border between the U.S. and Mexico, which between 2002 and 2003 was estimated to be 409 persons, just for the border section between Yuma, AZ and El Paso, TX.8
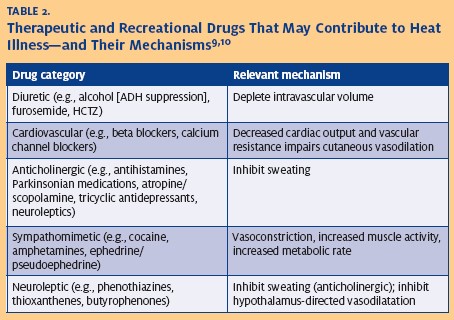
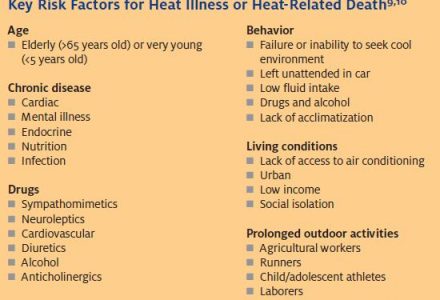
Several populations have increased risk of heat illness (Table 1). The elderly and the very young, patients with comorbidities, patients taking medications or drugs that interfere with heat homeostasis (Table 2), and persons with limited cognitive ability, low socioeconomic status, and mental illness are at elevated risk. Relatively young adults such as athletes, laborers, and border crossers are susceptible during high exertional states, even in moderate temperatures.
Diagnosis and Management
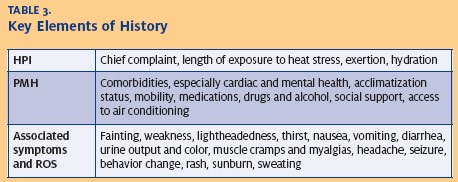
Key elements of the history include exposure, acclimatization status, comorbidities, drug and alcohol history, and a medication history (Table 3). Knowledge of patients’ social resources is crucial for disposition decisions and preventative counseling.
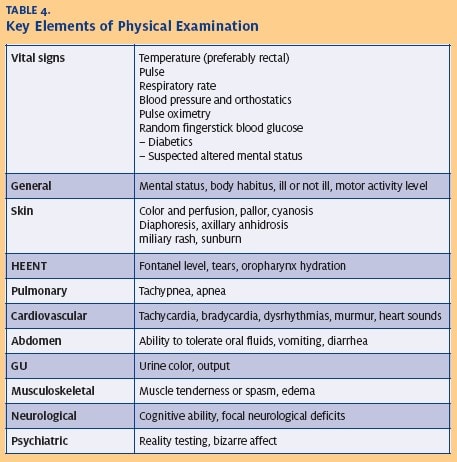
The physical examination should focus on vital signs, general appearance and mental status, hydration status, skin condition, and the cardiovascular and nervous systems. Vital signs, including orthostatics to assess volume status, help sort patients into those with relatively minor versus major heat illnesses.
Skin conditions, including heat rash and sunburn, interfere with sweating and evaporative heat losses.11
Anhidrosis should be assessed in the axilla, as forehead sweating is an unreliable marker.5
Hydration can be assessed from pulse and blood pressure, fontanel, oropharynx mucous membranes, lacrimation, sweating, active vomiting or diarrhea, and urine color and output.
Cardiovascular examination should focus on murmurs, especially in exertion-related syncope,and heart failure signs. In exertional heat illness, it is important to assess for muscle tenderness, considering rhabdomyolysis.
Altered mental status or an abnormal neurologic examination should prompt immediate transfer to a higher level of care, even if the patient’s temperature is normal (Table 4).
Heat Syndromes
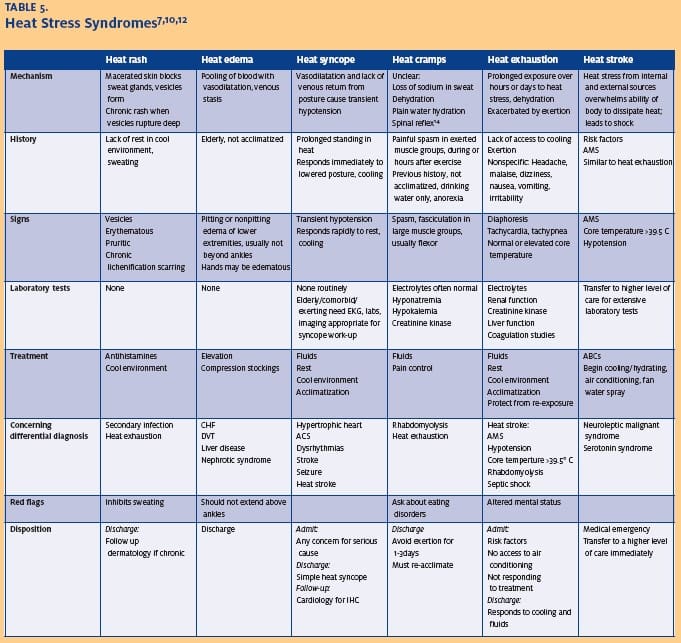
There are several common entities seen in urgent care centers related to heat exposure, ranging from minor annoyances to higher risk for significant morbidity. These include heat rash, heat edema and heat syncope, heat cramps, and heat exhaustion (Table 5).
Heat Rash
Heat rash, also known as prickly heat, lichen tropicus, and miliaria rubra, occurs when sweat ducts are blocked by dead skin. Tiny vesicles form as sweat accumulates under the skin, resulting in pruritis. Chronic vesicles can rupture into the surrounding tissue, causing skin thickening and scarring. Secondary Staphylococcus and Streptococcus infections can occur.
Treatment includes antihistamines for pruritis, cool baths, and time in a cool environment. Chronic heat rash will need dermatologic follow-up for treatment with salicylate gels to avoid scarring.7
Heat Edema
Heat edema occurs mostly in older individuals who are adjusting to an increased heat strain. Vasodilatation, in combination with relative venous stasis, causes blood pooling. No dehydration or salt imbalance is usually present, and diuretics are not warranted. This must be distinguished from more worrisome causes, including deep vein thrombosis (DVT), nephrotic syndrome, liver failure, and congestive heart failure. Heat edema is a benign condition that is self-limiting, and may be treated with elevation and compression stockings. Follow-up with a primary care provider is recommended in seven to 10 days (or sooner if the condition does not improve with conservative measures).
Heat Syncope
Heat syncope occurs when peripheral vasodilatation and impedance to venous return caused by posture combine to lower the blood pressure enough to interrupt cerebral blood flow. Classically, military personnel standing at attention with locked knees are at risk.
Persons usually recover promptly with lowered head, elevated lower extremities, and a cooler environment.
Differential diagnosis for syncope includes concerning entitities such as idiopathic hypertrophic cardiomyopathy, dysrhythmias, acute coronary syndrome, and cerebral vascular accident.
In a young, non-exerting, otherwise healthy individual who responds to appropriate therapy, disposition may include discharge home. However, advanced age, comorbidities, and a history of exertion at time of syncope require further testing. In young patients with exertional syncope, restriction on activity level pending a referral to a cardiologist for further work-up is appropriate.
Aggressive search for serious disease must be made in older patients and patients with comorbidities, and admission or transfer to a higher level of care is appropriate.
Heat Cramps
Heat cramps are defined as motor unit hyperactivity in major muscle groups, usually thigh or leg, during or several hours after prolonged exertion under heat stress.
The exact mechanism is not clear. It was originally thought that hyponatremia due to excess sweating and hydrating with water caused heat cramps. However, heat cramps can occur before any rehydration has taken place, and many patients with heat cramps have no electrolyte or serum osmolarity derangements. A spinal reflex caused by overexertion has also been proposed as a mechanism.13
The two most useful prophylactic steps to prevent heat cramps are heat acclimatization and consuming adequate water during exercise. Relative muscle dehydration appears before the subject experiences thirst, so the advice should be to consume water at regular intervals during exercise even if the athlete does not feel thirsty.
Treatment for heat cramps includes rehydration with an oral salt solution or IV normal saline, as well as pain control, which may require narcotics. Electrolytes should be checked and replaced as needed, and creatinine kinase levels measured to rule out rhabdomyolysis. Typically, heat cramps respond rapidly to treatment, rarely lasting for more than 15 minutes during a flare-up. They can produce agonizing spasms during a flare-up, and can recur several times over the next 24 to 48 hours. During the recovery period, the patient should avoid exertion since the spasms can be triggered by a normal muscular contraction.
Unfortunately, they can be triggered during sleep, and awaken the patient with severe pain. The painful contractions are usually in the flexor muscles, and hyperextension of the involved muscle may overcome the spasm. When they involve the hamstring flexors, extension of the hip and knee are useful, as is standing up, and slow mild pacing.
Icing the involved muscles may provide the patient with pain relief, and mild analgesics are useful when the cramps subside.
In the elderly patient who is perhaps already on a diuretic agent for hypertension, the cramps are worsened by any potassium imbalance. Many of these patients will obtain relief from potassium oral supplementation even when the serum electrolyte level of potassium is normal.
Heat Exhaustion
Heat exhaustion is generally a result of prolonged exertion or prolonged exposure to a higher heat index than normal. Symptoms are nonspecific, and can include any of the above syndromes, as well as lightheadedness, malaise, fatigue, headache, nausea, vomiting, decreased urine output, and thirst.
Dehydration and electrolyte abnormalities are common but not necessary to the diagnosis, and patients with a history of exertion need to have rhabdomyolysis excluded.
Patients with heat exhaustion need to be in a cool, air conditioned environment, and inappropriate extra clothing should be removed. Hydration can usually be accomplished with oral salt solution or normal saline, with electrolyte correction as necessary. Patients should respond to cooling and hydration; any patient with persistent symptoms or comorbidities should be admitted to the hospital.
Prudent discharge requires that the patient have access to a cool, air conditioned environment for the next 48 to 72 hours, especially for those with risk factors for heat illness. Elderly patients, patients with limited mobility, and mentally ill or retarded patients need a caretaker or family member to check on them at least twice a day during periods of higher than normal heat or humidity. Close follow-u p should be arranged. Workers and athletes likewise require 48 to 72 hours of decreased activity in a cool environment, and must re-acclimate.
Heat Stroke
Heat stroke needs to be considered in patients with core temperatures above 39.5 ºC, anhidrosis, or any alteration in mental status. These patients must be immediately transferred to a higher level of care. This is a true life-threatening emergency.
Prevention
All patients with heat illness are at higher risk for relapse in the short term and for recurrence in the long term. It is important to avoid re-exposure for two to three days, as heat shock proteins and body water composition take time to equilibrate. Athletes and laborers will need to re-acclimatize after a period of rest, and cannot immediately resume their previous level of exertion. It is appropriate to counsel all patients regarding heat illnesses during the summer months, regardless of their presenting complaint.
During the course of weather episodes in which the daily high temperature might exceed 90º F, or 80º F (32 ºC or 27ºC, respectively) with high humidity, urgent care physicians can reduce the burden of heat illness with brief counseling, educational handouts, and posters.Excellent patient information sources are available.14,15
Patients should be counseled to hydrate liberally, unless specifically contraindicated. Inactive individuals need four liters of fluids or more daily during heat waves, and the exerting adult may need up to 10 liters daily.
Thirst is an unreliable indication of hydration status, as it is mainly stimulated by hypernatremia, and hydration must often be scheduled. Exerting adults should drink 250 mL of fluid every 15 to 20 minutes during exercise, and children should drink 150 mL. It is often impossible to hydrate enough during exercise, and hydration must begin before activity and continue afterwards.
Thirst is stimulated by eating; hydration at meals in addition to during activities is necessary. Electrolyte solution is generally unnecessary for people consuming a normal diet, and has only been shown to increase exercise tolerance during the first three days of acclimitization. 3 However, if the taste is more tolerable, especially to children, this may encourage hydration. Patients not consuming a normal diet, exerting heavily for prolonged periods of time, or with gastroenteritis will benefit from electrolyte solutions, and there should be no hesitation to use intravenous fluids.
Air conditioning for as little as three hours per day is the only intervention known to be protective against heat stroke during heat waves.16 For this reason, some urban areas have heat wave response plans that include heat shelters, such as malls. Fans have not been shown to be protective.17
Exertion should, if possible, occur in the early morning or late afternoon or evening, avoiding activity during the heat of the day. Outdoor laborers should be given regular rest and hydration breaks; an air conditioned rest area is protective against heat illness and maximizes exercise tolerance.
Summary
Heat illness has an unknown incidence, but heat stroke is the second largest cause of environmental or weather caused mortality—more than hurricanes, tornados, and lightning combined, second only to hypothermia.18 It is preventable through public health measures, education, and early intervention.
Most presentations of heat illness can be quickly and adequately treated by the urgent care provider, and serious morbidity and mortality can be avoided by attending to risk factors, excluding serious diagnoses, preventing complications, and promptly recognizing severe disease. Preventative education remains an important part of the urgent care provider’s role.
References
1. Heat Index Chart. www.nws.noaa.gov/om/heat/index.shtml. 2007.
2. Keim SM, Guisto JA, Sullivan JB, Jr. Environmental Thermal Stress. Ann Agric Environ Med. 2002;9(1):1-15.
3. Sawka MN, Montain SJ. Fluid and Electrolyte Supplementation for Exercise Heat Stress. Am J Clin Nutr. 2000;72(2 Suppl):564S-572S.
4. Bouchama A, Knochel JP. Heat Stroke. N Engl J Med. 2002;346(25):1978-1988.
5. Yaqub B, Al Deeb S. Heat Strokes: Aetiopathogenesis, Neurological Characteristics, Treatment and Outcome. J Neurol Sci. 1998;156(2):144-151.
6. Heat-related Deaths–United States, 1999-2003. MMWR Morb Mortal Wkly Rep. 2006;55(29):796-798.
7. Walker JS, Hogan DE. Heat Emergencies. In: Tintinalli JE, Kelen GD, Stapczynski JS, eds. Emergency Medicine: A Comprehensive Study Guide. 6th ed. New York: McGraw-Hill, Medical Pub. Division; 2004:1183-1190.
8. Sapkota S, Kohl HW, 3rd, Gilchrist J, et al. Unauthorized Border Crossings and Migrant Deaths: Arizona, New Mexico, and El Paso, Texas, 2002-2003. Am J Public Health. 2006;96(7):1282-1287.
9. Tintinalli JE, Kelen GD, Stapczynski JS. Emergency Medicine: A Comprehensive Study Guide. 6th ed. New York: McGraw-Hill, Medical Pub. Division; 2004.
10. Glazer JL. Management of Heatstroke and Heat Exhaustion. Am Fam Physician. 2005;71(11):2133-2140.
11. Pandolf KB, Griffin TB, Munro EH, et al. Persistence of Impaired Heat Tolerance From Artificially Induced Miliaria Rubra. Am J Physiol. 1980;239(3):R226-232.
12. Wexler RK. Evaluation and Treatment of Heat-Related Illnesses. Am Fam Physician. 2002;65(11):2307-2314.
13. Noakes TD. Fluid and Electrolyte Disturbances in Heat Illness. Int J Sports Med. 1998;19 Suppl 2:S146-S149.
14. Naughton MP, Henderson A, Mirabelli MC, et al. Heat-related Mortality During a 1999 Heat Wave in Chicago. Am J Prev Med. 2002;22(4):221-227.
15. Bernard SM, McGeehin MA. Municipal Heat Wave Response Plans. Am J Public Health. 2004;94(9):1520-1522.
16. Heat-related Illnesses and Deaths–United States, 1994-1995. MMWR Morb Mortal WklyRep. 1995;44(25):465-468.
17. Martinez M, Devenport L, Saussy J, et al. Drug-associated Heat Stroke. South Med J. 2002;95(8):799-802.
18. Heat Wave—A Major Summer Killer. NOAA National Weather Service, www.nws.noaa.gov/om/heat/heat_wave.shtml. Accessed August 9, 2007.