Urgent message: Hours of operation changes may have more effect on leveling patient arrival volumes in a pediatric urgent care compared with an online queueing system alone.
Aimy Patel, MD; Jennifer Johnson, MD; Brian R. Lee, PhD, MPH; Amanda Montalbano, MD, MPH
Citation: Patel A, Johnson J, Lee BR, Montalbano A. More timely care: effect of online queuing vs change in hours of operation on hourly arrival volumes. a practice management reflection. J Urgent Care Med. 2021;15(9):25-30.
Introduction
Customer experience is tied to the perception of waiting in all industries, healthcare being one of them. Maister shared a simple formula that explained a consumer’s satisfaction level can be the difference between their expectation and their perception of the value of the delivered service.1 He hypothesized that consumers perceive wait as more than just time spent, but also is impacted by the uncertainty of the duration of the wait, unfair prioritization of being attended to in a timely manner, unexplained waits, or simply the boredom of unoccupied waiting time. As technology advanced, online queue management systems began to emerge and became a solution to improving consumer’s satisfaction level, either adjusting expectations or improving the perception of waiting by providing more transparency. This system was translated for use in the healthcare model, specifically the urgent care setting.
In a walk-in patient care model, such as urgent care, challenges arise when boluses of patients arrive, resulting in a longer-than-average wait time. The prolonged waits that occur when this happens lead to a secondary problem of providing realistic expectations of wait time that result in decreased patient experience scores, especially in the timeliness category.
As explained above, beyond the added minutes of waiting, the anxiety of “wasted” time is compounded in an acute care setting. When those evaluating the experience reflect on whether their expectation of urgent medical attention was met, the gap can be pronounced if the care being sought was for their child. With over two-thirds of pediatric urgent cares across the nation now using some form of online queue management,2 we wondered, could an online queueing system overcome the parental expectations of expedited acute care for their child ? Was this technology the solution for matching demand to capacity, or could there be another intervention to better address this problem?
We implemented two interventions to level-load our patient arrival volumes, then retrospectively reviewed our data to answer this clinical practice question: How can a pediatric urgent care manage arrival volumes to match clinical capacity and improve patient experience?
Setting and Background
Children’s Mercy Kansas City is a freestanding independent pediatric health organization which has grown from one pediatric urgent care to four in the last 8 years. The freestanding pediatric urgent care centers serve the greater Kansas City metro area and one rural location. Staffing is 36 pediatric physicians within the Division of Urgent Care and 12 advanced practice nurse practitioners (NP), either pediatric or family practice NPs. At the start of the study period in July 2017, hours of operation were noon to 10 pm daily. Patient volumes increased 700% since opening the first urgent care center and by 2019 the annual census was 97,445 patient visits. With this growth, there was a decrease in patient experience scores regarding timeliness of care provided.
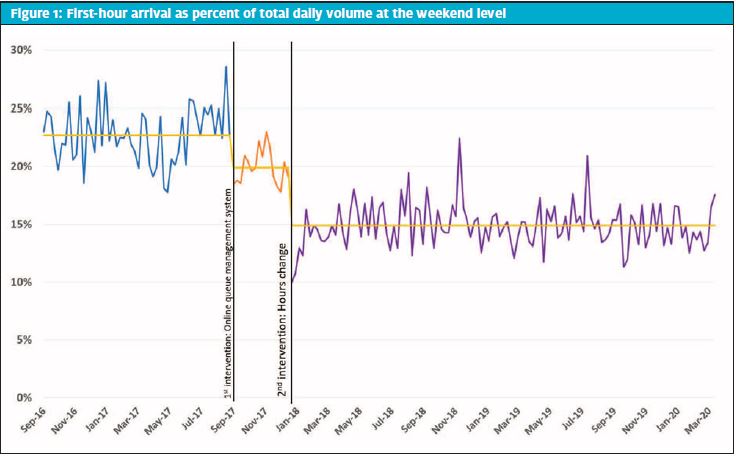
Upon further study of patient throughput, there was a recognized pattern that the largest daily volume of patients (20%–25%) presented in the first hour on the weekends. This would result in long wait times and longer lengths of stay on the weekends, including for chief complaints that typically would not require more than a 15–20 minute visit.
Two interventions
In the fiscal year 2018, our Division of Urgent Care implemented two different interventions across the then three metropolitan sites. The first was the implementation of an online queuing system in September 2017. This involved several key stakeholders, including the Division Director of Urgent Care, the Manager of Patient and Family Engagement, and the Senior Director of Nursing and Emergency Services with the approval of Strategy, Marketing, and Information Technology (IT). Ultimately the implementation also involved Information Systems (IS), Legal, and Access Representatives.
Eight online queuing systems were identified and researched. Analysis of the different programs consisted of online research followed by user experience phone conversations. The features that our institution looked at included online sign-in capability, proactive communication, customizable reporting, reservation capability, and a visible queue. Additional factors that influenced decision making included: cost/budgetary constraints, company culture, availability of technical support resources, ability to customize offerings, user interface preferences, and marketing support. The adoption of the final online queueing system allowed patients to save their spot in line from the comforts of their home and arrive 15 minutes prior to their reservation time.
The second intervention was a change in hours of operation on the weekends. The standard daily hours of operation were noon to 10 pm. Historical arrival data demonstrated that the highest volumes of patients were on the weekends, with the largest percentage arriving at noon upon opening and low arrival numbers after 8 pm. Starting January 6, 2018, we remained open 10 hours a day, but on the weekends adjusted to open 2 hours earlier, operating 10 am–8 pm.
Key stakeholders were the Division Director of Urgent Care and the Senior Director of Nursing and Emergency Services. Weekend UC parents were polled; over 65% desired a change in our hours of operation to open 2 hours earlier. We also discussed this potential change with private pediatric practices within the Children’s Health Network in Kansas City and none voiced any concerns over the urgent care change in hours. Only one private pediatric group consistently provided weekend or holiday walk-in care. Ancillary services supporting UC also expressed support for the change in hours.
A survey of all UC staff (providers, nurses, lab, radiology, environmental services, access representatives, security, respiratory therapy, and social work) showed 75% were in support of the hours change, as well. In comparison to other urgent cares in our service area, most opened prior to noon and none were open beyond 8 pm; therefore, the new hours would more closely align with our competitors.
What We Measured
- First hour arrival volumes: The main outcome measure was the first hour arrival volume presented as a percent of total daily volume (TDV) to account for seasonal variability. The numerator was the sum of the first hour volumes on Saturday and Sunday for each weekend. The denominator was the total volume for each weekend.
- Hourly arrival volumes: Variation in hourly arrival volumes for each hour of a shift for the weekend as a percentage of TDV for each hour.
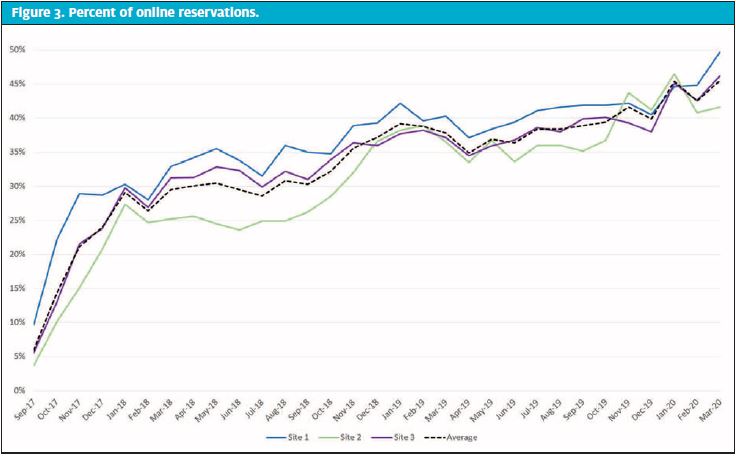
- Percent online reservations: Percentage of patients that used our online queuing system each month.
- Experience scores in two domains from a validated national patient- and family experience survey:3-5
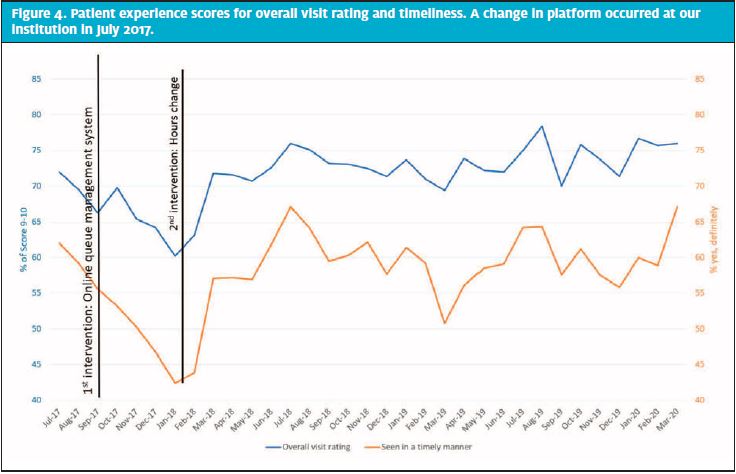
- Overall rating: percent of survey respondents that responded with an overall “rating of visit” a 9 or 10 on a 11-point scale, reported monthly.
- Perception of timeliness: percent of respondents choosing “yes, definitely” on a 4-point Likert scale to their child being seen in a timely manner, reported monthly.
What We Found
We evaluated arrival volume data for 12 months prior to the interventions, 3 months after the first intervention, and 6 months after the second intervention. We have since added data for an additional 21 months to monitor maintenance.
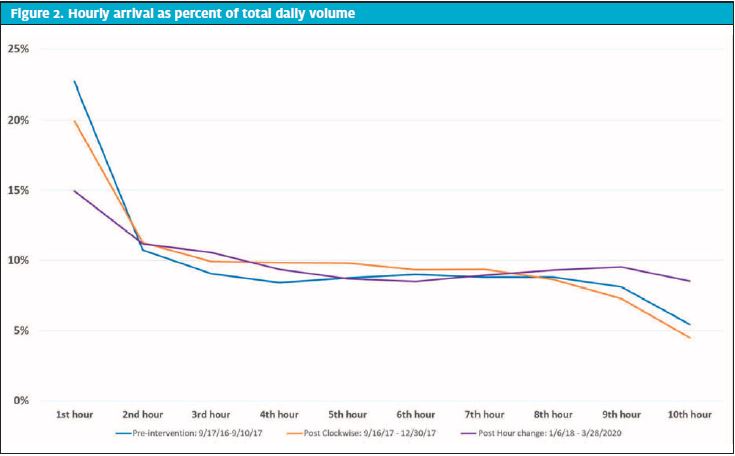
The first intervention (introduction of the online queuing system) decreased the percentage of first hour patient arrival volumes from an average of 22.7% to 19.9%. The second intervention (the change in our hours of operation) decreased the percentage of patient arrival volumes in the first hour of operation to an average of 14.3% after 6 months, and 14.9% for the full 27 months evaluated (Figure 1). Individual hourly arrival volumes continued to demonstrate a considerable range even after the implementation of the online queuing system (hourly arrival volumes varied 5%─23% vs 5%─20%, pre- and post-queueing system intervention, respectively). However, the change in hours of operation did show a tightening in the variation of the hourly arrival volumes to 9%─14% of total daily volume (Figure 2).
The percent of total encounters using the online queuing system increased from a range of 5% to 15% per urgent care site in the first month up to 55% in the most recent month (Figure 3). Overall rating of visit measured by patient experience surveys showed an initial decline for overall rating and timeliness after the introduction of the online queueing system (Figure 4). However, it was typical for overall rating and timeliness to decline over the flu season. It was our hope that the intervention of online queuing would stave off the typical dip. While we did not see that happen immediately after the intervention, these scores rebounded and maintained a sustained increase after the change hours of operation, which may have been due to the increase in use of the online queueing system. Moreover, the late influenza season that hit in March 2019 did not show as precipitous of a decline in either metric. These scores were followed on a monthly average, not specific to the weekend scores; however, using the monthly average increased the overall sample size to reflect a truer average experience for patients and families.
The patient experience survey also captured qualitative feedback (“What else would you like to tell us about your experience?”). After the introduction of the online queueing system, there was immediate positive feedback via the comments, such as “Online check-in was great”, “I loved the ability to reserve a time slot!”, and “I liked the check-in process where you could have your spot held for you so you could come back.” We also saw comments regarding inaccurate long projected wait times—that while the families were happy they didn’t have to wait they wished the times could be more accurate to help them make a triage decision of where to seek care. These types of comments dissipated as we improved our velocity estimations and familiarity with the online queueing platform.
Conclusion
An online queuing system decreased our first hour arrival volumes only slightly. It was widely accepted and popular with our patient families as gleaned from the increasing use of the system and from comments received on our patient experience surveys. However, it did not level our hourly arrival volumes as we had hoped.
The change in hours of operation after instituting the online queuing system did show a larger decrease in the first hour arrival volumes as well as less variation in volume of patients that arrived hourly. Therefore, the hours of operation change helped not only to better meet demand upon opening, but also to level load our patient flow throughout the day compared with the online queuing. These interventions were not taken lightly, and we were able to engage customers, staff, and community members in the process to obtain the best uptake and results.
Online queue management systems have been a game changer for our urgent care patient population. This system has allowed the urgent care service line to manage the psychology of waiting during a high-anxiety situation of requiring acute care needs for a child. It allowed flexibility for families to pick the time that works best for them, thereby allowing them to occupy their time elsewhere and decrease the “waste in waiting” on site. For families that walk in, the system provides a wait time to provide transparency to the length of wait which in turn can appropriately set their expectations. However, with urgent care not being a 24/7 service, the pent-up demand at opening could not be overcome with an online queueing system alone. The additional intervention of an hours-of-operation change helped us further provide care when families were ready to seek care.
Limitations
While this is the first published report specific to operational changes in a pediatric urgent care setting, the findings may not be generalizable to the general urgent care setting. The retrospective nature of evaluating the interventions reflects the short time frame between our two interventions. There is the possibility that the online queuing system alone might have had more of an effect on our first hour arrival volumes and level loading our patients over time, if it were able to be monitored for a longer period prior to initiating a change in hours of operation. However, the benefit of both interventions has proven to remain successful with long-term monitoring.
References
- Maister DH. The Psychology of Waiting Lines. 1985. Available at: http://www.columbia.edu/~ww2040/4615S13/Psychology_of_Waiting_Lines.pdf. Accessed May 12, 2021.
- Montalbano A. Unpublished data.
- Co JPT, Sternberg SB, Homer CJ. Measuring patient and family experiences of health care for children. Acad Pediatr. 2011;11(3 Suppl):S59-67.
- Jenkinson C, Coulter A, Bruster S, et al. Patients’ experiences and satisfaction with health care: results of a questionnaire study of specific aspects of care. Qual Saf Health Care. 2002;11(4):335-339.
- Jenkinson C, Coulter A, Reeves R, et al. Properties of the Picker Patient Experience questionnaire in a randomized controlled trial of long versus short form survey instruments. J Public Heal Med. 2003;25(3):197-201.
Author affiliations: Aimy Patel, MD, Division of Urgent Care, Children’s Mercy Kansas City; Department of Pediatrics, University of Missouri-Kansas City School of Medicine. Jennifer Johnson, MD, Division of Urgent Care, Children’s Mercy Kansas City; Department of Pediatrics, University of Missouri-Kansas City School of Medicine. Brian R Lee, PhD, MPH, Health Services and Outcomes Research, Children’s Mercy Kansas City. Amanda Montalbano, MD, MPH, Division of Urgent Care, Children’s Mercy Kansas City; Department of Pediatrics, University of Missouri-Kansas City School of Medicine. The authors have no relevant financial relationships with any commercial interests.
