Urgent message: Medical histories can help inform diagnosis, but clinicians must ensure their decisions are not swayed by erroneous historical elements or cognitive biases.
Candace Walkley, MD and Kyle Swanson, OMS-3
INTRODUCTION
Staphylococcus aureus and Streptococcus pyogenes may cause acute and inflammatory infections of the soft tissue in immunocompetent patients. However, patients with indolent and progressive lymphocutaneous infections should be evaluated for atypical bacterial and fungal pathogens.
CASE PRESENTATION
In March 2021, a 57-year-old healthy and immune-competent female presented to an urgent care provider complaining of a tender rash on her right hand. She reported that 3 weeks prior, she received multiple punctures to the hands while clearing dead plants from her yard following a harsh winter freeze. Within 1 week, she developed a red, tender, nonsuppurative, nodular lesion on the dorsum of the metacarpophalangeal joint of the long finger on her right hand. She was diagnosed with a staphylococcal infection and empirically prescribed 10 days of doxycycline. She did not improve and, soon after, developed multiple erythematous and nonsuppurative nodules on her right forearm and hand, proximal to the initial hand lesion.
Two months later, the patient presented to urgent care for persistent lesions on her right forearm after developing a painless swelling of her right elbow. She was diagnosed with a staphylococcal infection and empirically treated with 10 more days of doxycycline.
Two months after the second urgent care visit, she developed additional skin lesions and worsening of the elbow swelling. She presented again, whereupon the provider ascertained that she owned cows, dogs, and cats and was a horse trainer who traveled with horses on transatlantic flights to and from Belgium. Without further evaluation, she was diagnosed with brucellosis and empirically prescribed 45 days of doxycycline and rifampin.
One week later, without improvement, she presented as a self-referral to the authors, one of whom is trained in infectious disease, for a second opinion. Aside from her right hand, arm, and elbow complaints, her review of systems was negative.
Exam revealed an afebrile and well-appearing patient with numerous right hand and forearm erythematous and flesh-colored, nonsuppurative, nodular lesions along the lymphatics and a significant swelling of the right olecranon bursa with mild overlying, nontender erythema (see Figure 1 and Figure 2). Complete blood count and comprehensive metabolic profile were normal. Chest and right elbow radiographs were negative for pulmonary or osseous involvement. Punch biopsies from the nodular skin lesions on the right forearm revealed granulomatous reaction suggestive of infectious etiology. Periodic acid Schiff and Fite’s acid-fast stains were unrevealing. Fungal culture of the tissue was negative after 4 weeks.
Based on the patient’s history, clinical features, and histopathology, she was diagnosed with lymphocutaneous sporotrichosis with involvement of the right olecranon bursa and treated with itraconazole.


Differential Diagnosis
In 2014, the Infectious Diseases Society of America (IDSA) issued guidelines on the diagnosis and management of skin and soft tissue infections (SSTIs).1 The recommendations include dividing soft tissue infections into purulent and nonpurulent presentations, recognizing that when purulence is a presenting feature, generally S aureus is the culprit. In individuals who are systemically ill with a purulent infection, the recommendation is to treat methicillin-resistant S aureus using either an intravenous antibiotic (vancomycin, daptomycin, linezolid, telavancin, or ceftaroline) or oral doxycycline or trimethoprim-sulfamethoxazole.
In individuals with a nonpurulent presentation, the recommendation is to focus on treating S pyogenes using penicillin (if known group A streptococcal infection) or a cephalosporin.
The most important feature of this patient’s case is her indolent lymphocutaneous presentation. Moreover, the clinical decline while taking doxycycline excludes S aureus and S pyogenes as etiologies, especially since a prolonged and gradual clinical course is distinctly atypical for infection with these organisms.
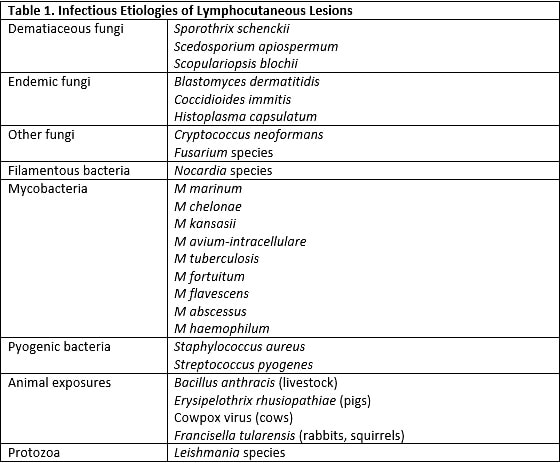
The differential diagnosis of an immune-competent patient with progressive, indolent, nonpurulent lymphocutaneous nodules after exposure to detritus is limited to endemic and dematiaceous fungi (eg, Blastomyces, Scedosporium, and Sporothrix species.), filamentous bacteria (Nocardia), and atypical mycobacteria (see Table 1). Exposure to farm animals should broaden the differential to include anthrax, tularemia, erysipeloid, and cowpox, but these infections cause a more acute presentation with different features.2
DISCUSSION OF DIAGNOSTIC ERROR AND SPOROTHRIX SCHENCKII
We present a classic case of sporotrichosis that was misdiagnosed because of a focus on the patient’s history of exposure to animals and a failure to recognize the indolent nature of cutaneous fungal infections.
Sporothrix schenckii is a fungus found commonly in soil and plant matter. Infection follows inoculation of the skin through abrasion or penetration while working with plants or soil. Sporotrichosis, or “rose gardener’s disease,” most commonly presents as a lymphocutaneous eruption with an erythematous, subcutaneous nodule at the site of inoculation. When untreated, the infection progresses indolently and proximally, causing nodules along the lymphatics. The most common extracutaneous presentation is arthritis following hematogenous dissemination and, ultimately, possible progressive joint damage if untreated.3
Sporotrichosis is a rare infection that many providers do not include in their initial differential diagnosis of skin lesions. In stable and immune-competent patients with recent skin punctures, the initial diagnosis of bacterial soft tissue infection and empiric treatment with doxycycline for staphylococcal and streptococcal species are reasonable. However, lack of resolution and continued indolent spread of skin lesions call for a reevaluation of possible etiologies.
This patient’s final visit to urgent care resulted in treatment for brucellosis despite a lack of suggestive symptoms and was based solely on the historical animal exposures. Failure to reexamine the differential diagnosis and the recurrent prescription of an inappropriate antibiotic resulted in dissemination of the infection to the bursa of the elbow. Unfortunately, osteoarticular involvement makes the infection more complex and difficult to treat.
Practitioners should be aware of common cognitive biases that may impact clinical reasoning, including anchoring bias, defined as a repeated focusing on a single piece of information despite contradictory evidence. Anchoring on this patient having a red, tender nodule on the right hand without considering the lack of fever and purulent drainage, the history of the lesion, and the lesion’s lack of response to empiric treatment for common bacterial pathogens led repeatedly to the incorrect diagnosis of a pyogenic soft tissue infection. Furthermore, the transition of the working diagnosis to brucellosis was based on new information regarding animal exposures and undervalued the puncture wound as a likely site of inoculation. Anchoring to new information and disregarding the previous history of potential infection via direct inoculation led to the initiation of aggressive treatment for a rare and unlikely disease despite the patient demonstrating the classic presentation of another more likely condition.
Awareness of the pitfalls in clinical reasoning, such as the presence of cognitive biases, can reduce negative outcomes by imploring us to carefully consider our decision-making. Metacognition involves clinicians evaluating their thought processes in real time, reflecting on previous decisions, and improvement in future practice.
This case highlights the importance of having a thorough differential when assessing patients in urgent care settings to avoid unnecessary treatments and appropriately manage infections in a timely manner.
CASE RESOLUTION After 8 months of itraconazole treatment, the patient demonstrated slow resolution of lymphocutaneous lesions and substantial improvement in the right olecranon bursitis (see Figure 3, Figure 4, and Figure 5).



CONCLUSION
A high degree of clinical suspicion is necessary when developing a differential diagnosis for soft tissue injuries in the urgent care setting. Classifying soft tissue lesions based on the acuity of their clinical presentation can help providers more accurately determine infectious etiologies. Sporotrichosis is the most common cause of indolent lymphangitis and should be considered in any patient with a history of penetrating wounds while working with soil or plant debris. When a patient treated for pyogenic infectious lymphangitis returns without improvement or is worse, it is important for clinicians to broaden the differential diagnosis to include uncommon etiologies that better fit the patient’s presentation.
REFERENCES
- Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59(2):e10-e52.
- Tirado-Sánchez A, Bonifaz A. Nodular lymphangitis (Sporotrichoid lymphocutaneous infections). Clues to differential diagnosis. J Fungi (Basel). 2018;4(2):56.
- Orofino-Costa R, de Macedo PM, Rodrigues AM, Bernardes-Engemann AR. Sporotrichosis: an update on epidemiology, etiopathogenesis, laboratory and clinical therapeutics. An Bras Dermatol. 2017;92(5):606-620.
RECOMMENDED READING
Saposnik G, Redelmeier D, Ruff CC, Tobler PN. Cognitive biases associated with medical decisions: a systematic review. BMC Med Inform Decis Mak. 2016;16(1):138.
Additional JUCM Articles on Skin Lesions
- A Blistering Rash In An Otherwise Healthy 9-Year-Old Boy
- Kaposi Sarcoma Presenting In The Urgent Care Setting As A Single Mass Lesion Of The Foot
- Reducing Morbidity And Mortality Due To MRSA In The Urgent Care Setting
(Full written consent was obtained from the patient for publication of her case, including photographs.)
Author affiliations: Candace Walkley, MD, Sam Houston State University. Kyle Swanson, OMS-3, Sam Houston State University.
