Q: The Centers for Medicare and Medicaid Services (CMS) started issuing new Medicare cards to beneficiaries in April of this year. What do I need to know about these changes to limit disruption to my patients and medical practice?
A: CMS is required to issue new Medicare cards as a part of the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015, which mandates that CMS remove Social Security Numbers (SSN) from all Medicare cards by April of 2019. The primary reason behind the change is to combat identity theft by removing SSNs from the cards. CMS is replacing SSN-based health insurance claim numbers (HICN) with Medicare beneficiary identifiers (MBI) on the new Medicare cards, which is what medical practices will use moving forward for all Medicare transactions, such as billing and checking eligibility and claim statuses. Every Medicare beneficiary will receive a new Medicare card with a unique MBI that is confidential and protected personal information.
Like HICNs, which can have up to 11 characters, MBIs also have 11 characters. However, unlike HICNs, which are based on SSNs, they are randomly generated and nonintelligent, so they don’t have any hidden or special meaning. MBIs include numbers and uppercase letters; however, if you enter the letters in as lowercase, CMS’s system will automatically convert them to uppercase.
For example, MBI number 1EG4-TE5-MK73 is created using the following format:
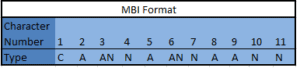
C – numeric 1 through 9; N – numeric 0 through 9; AN – either A or N; A – alphabetic character (A…Z); excluding (S, L, O, I, B, Z).
The total number of possible SSNs is less than 30 billion, but the total number of possible MBI numbers will go to over 10 trillion.
CMS started mailing the new cards out to Medicare beneficiaries in April of 2018 and will continue to mail them out in waves through April 2019. See Table 1 for the mailing schedule.
Table 1: New Medicare Cards Mailing Schedule
| Wave | States Included | Cards Mailing |
| Newly eligible people with Medicare | All ─ nationwide | April 2018─ongoing |
| 1 | Delaware, District of Columbia, Maryland, Pennsylvania, Virginia, West Virginia | April─June 2018 |
| 2 | Alaska, American Samoa, California, Guam, Hawaii, Northern Mariana Islands, Oregon | April─June 2018 |
| 3 | Arkansas, Illinois, Indiana, Iowa, Kansas, Minnesota, Nebraska, North Dakota, Oklahoma, South Dakota, Wisconsin | After June 2018 |
| 4 | Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Rhode Island, Vermont | After June 2018 |
| 5 | Alabama, Florida, Georgia, North Carolina, South Carolina | After June 2018 |
| 6 | Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Texas, Utah, Washington, Wyoming | After June 2018 |
| 7 | Kentucky, Louisiana, Michigan, Mississippi, Missouri, Ohio, Puerto Rico, Tennessee, Virgin Islands | After June 2018 |
Source: Centers for Medicare and Medicaid Services. New Medicare card mailing strategy. Available at https://www.cms.gov/Medicare/New-Medicare-Card/NMC-Mailing-Strategy.pdf. Accessed May 2, 2018.
You can use either the HICN or the MBI during the transition period, which is April 1, 2018 through December 31, 2019. CMS says it is monitoring the use of HICNs and MBIs during this time to see how many practices are ready to transition to only MBIs by January 1, 2020. The plan is to have medical practices submit claims using only MBIs regardless of the date they performed services by January 1, 2020. However, there are a few fee-for-service claim exceptions:
- Appeals – You can use either the HICN or MBI for claims appeals and related forms
- Claim status queries – You can use either the HICN or the MBI to check the status of a claim if the earliest date of service on the claim is before January 1, 2020. Use the MBI if you’re checking on the status of a claim with a date of service after January 1, 2020
Nothing about your patients’ Medicare benefits is changing, but to ensure there is minimal disruption of services, we recommend you train your front desk staff to ask patients if they have received their new Medicare cards if they present with the old ones. Work with your front desk to develop a process to track patients who present with old Medicare cards, including documentation of the discussion your front desk staff had with patients and a way to flag patient accounts so your front desk remembers to ask them for the new card again the next time the patient visits your center. Working closely with your staff and having a strong process in place will ensure both you and your patients experience minimal disruption through this transition.
Source: Centers for Medicare and Medicaid Services. (2018). New Medicare cards. Available at https://www.cms.gov/Medicare/New-Medicare-Card/index.html#target. Accessed May 2, 2018.
