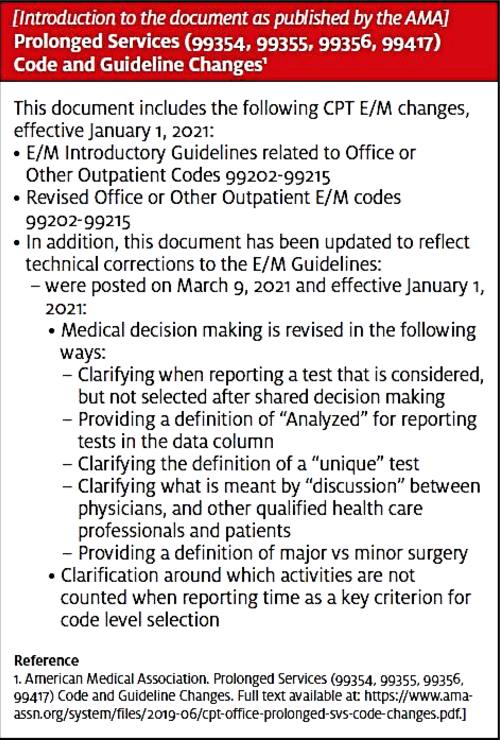
On March 9, 2021, the American Medical Association updated the new evaluation and management (E/M) coding guidelines with technical corrections. These clarifications apply to the office visit codes 99202–99215 and are retroactive to January 1, 2021.
In the past few months there has been industry confusion over whether a test can be counted under the data element for the E/M level when the practice is also billing for the test. The AMA has answered this question with further guidance.
Which In-House Tests Should Be Counted?
The Services Reported Separately section and definitions were revised. Documentation now supports counting the order of each unique laboratory test under Category 1: Tests and documents regardless of who is billing the service.
The professional component of a test is defined as the physician’s interpretation of the results with preparation of a separate distinctly identifiable signed written report. The professional component is part of the global CPT code or may be reported with modifier 26 when that is the only portion of the test performed.
According to the corrections, tests with a professional component (eg, radiology) that is reported by the practice would not be counted under the data element. However, tests without a professional component (eg, laboratory) would be counted.
This guidance may also support counting the order of a test when only the technical component of that test is billed. Usually this is with a TC modifier, but there are some codes (eg, ECGs) in the medicine section that have unique CPT codes for each component of the test when performed separately.
The AMA further clarified that pulse oximetry is not considered a test and would not be counted.
When Should Tests Be Counted?
The visit for which visit a test should be counted as a data element was explained further by the AMA.
Basically, tests can be counted under Category 1: Tests and documents only once regardless of when the test results are analyzed.
A test ordered/reviewed during a visit is counted as one unique test for the level of that visit.
A test ordered/reviewed outside of a visit is counted as one unique test for the level of the next visit.
You cannot count an order of a test in one visit and the results of this test in a subsequent visit.
Can Tests Considered Be Counted?
Finally, the AMA added that tests considered but not selected may be counted as an order under Category 1: Tests and documents. To quote the guidelines verbatim:
“Ordering a test may include those considered, but not selected after shared decision making. For example, a patient may request diagnostic imaging that is not necessary for their condition and discussion of the lack of benefit may be required. Alternatively, a test may normally be performed, but due to the risk for a specific patient it is not ordered. These considerations must be documented.”
As a reminder, a unique test is represented by a CPT code regardless of the number of times it is billed. For example, multiple ECGs would be counted as one order. A clinical laboratory panel would be counted as a single test as it is one unique CPT code.
Additional Clarification Regarding Risk
The AMA emphasized that the Number and Complexity of Problems Addressed at the Encounter element relates to risk from the condition while the Risk of Complications and/or Morbidity or Mortality of Patient Management relates to the management selected. The two are distinct elements that may not always correlate.
This supports using the differential diagnosis, not the final diagnosis, when determining if the presenting condition has a high risk of morbidity without treatment. While a patient may present with symptoms that may cause a high risk of morbidity, the final diagnosis may not be highly morbid. It’s the differential diagnosis, however, that determines the clinician’s medical decision-making (MDM).
Based on these corrected guidelines and observations from our audits, practices need to continue to educate their providers on how best to document what they are considering for each of the elements of MDM.
- Number and Complexity of Problems Addressed should be based on the risk of the presenting condition, not the final diagnosis.
- Amount and/or Complexity of Data to Be Reviewed and Analyzed may include tests considered but not selected (eg, patient declines).
- Risk of Complication and/or Morbidity or Mortality of Patient Management should include management options considered but also not selected.
The challenge continues as providers struggle to put everything they are considering in a succinct note to get credit for their work.
The entire document, CPT Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99417) Code and Guideline Changes, is available at https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf.