Published on
Urgent Message: This narrative review of non-steroidal anti-inflammatory drugs (NSAIDs) characterizes the specific evidence-based indications, previous studies on dosing and route, and side effects of these medications. It supports NSAIDs as an important class of medications in the management of acute pain in urgent care and emergency settings.
Campbell Belisle Haley, MD; Andy T. Hsueh, MD; Chih-Hsuan Chen, MD; Ariana M. Nelson, MD
Citation: Belisle Haley C, Hsueh AT, Chen CH, Nelson A. NSAIDs in Urgent Care and Emergency Departments: A Narrative Review. J Urgent Care Med. 2024; 18(7): 42-51
Key Words: Non-steroidal anti-inflammatory drugs, pain, extremity injury, headache, renal colic
Abstract
Background/Objective: Non-steroidal anti-inflammatory drugs (NSAIDs) are common medications that are used in a variety of healthcare settings. We aim to analyze the utility of NSAIDs in treating different painful conditions when compared to other alternative medications, their effectiveness between different dosing and routes, as well as the potential side effects of NSAIDs. The goal of this review is to guide urgent care providers in using these medications more effectively.
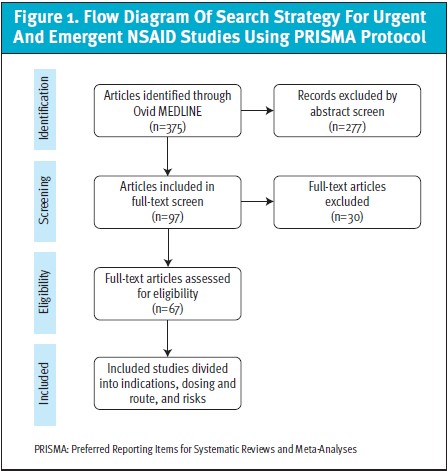
Methods: We searched the MEDLINE database and developed a search term strategy using medical subject headings (MeSH) to capture NSAID-related studies in urgent care or emergency settings. Based on the initial full-text review, chief complaints were simplified into the following categories: trauma/extremity injury; headaches; nontraumatic back pain; abdominal pain (excluding renal colic); renal colic; and pediatric pain.
Results: Sixty-seven studies were included in our narrative review. For traumatic pain, when compared to opioids, NSAIDs are as effective as opioids with less dependence. In comparison with acetaminophen, most studies showed comparable results in pain reduction, and only 1 observational study showed a lower analgesic effect with NSAIDs. In patients with headaches, NSAIDs and antiemetics combined lead to a higher discharge rate and more significant pain relief; however, in a randomized controlled trial (RCT) in children, antiemetics alone have similar results as combined therapy. For renal colic, 2 RCT trials revealed that NSAIDs have a higher analgesic effect than intravenous (IV) opioids or acetaminophen. Moreover, intramuscular (IM) diclofenac was found to be superior to its oral form at 5 minutes post-administration, and there are 5 RCTs showing no more pain relief benefits of ketorolac after doses higher than 10mg. NSAIDs are also associated with a higher risk of failure of colorectal anastomosis, non-variceal gastrointestinal (GI) hemorrhage, and gastroduodenal ulcers.
Conclusion: NSAIDs are safe, effective analgesic options that can be considered alongside acetaminophen for most acute painful conditions. Compared to opioids, NSAIDs have fewer side effects with comparable pain reduction. Single-use and short-term NSAID use is generally safe for patients ranging from geriatric to children over 6 months old; however, side effects of bleeding, surgical anastomotic failure, and anaphylaxis should be considered.
Introduction
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly administered and prescribed pain medications in urgent and emergent settings for numerous conditions and populations.1 They can be safe, efficacious, and opioid-sparing medications in children and adults, and ibuprofen is the single most prescribed medication for pain and inflammation in both groups.2 Typical indications for these medications include migraines, renal colic pain, traumatic and non-traumatic musculoskeletal pain, and acute low back pain.3 In addition to oral medications like ibuprofen, NSAIDs have proven efficacy in intravenous (IV), intramuscular (IM), intranasal, and topical administration. Despite their utility, NSAIDs can lead to adverse drug reactions and have been implicated in increased bleeding, cardiovascular events, and renal injury.5,6 However, these risks need to be balanced with the risks of alternative medications. For example, opioids can cause various central nervous system (CNS) side effects ranging from euphoria to dizziness to cognitive issues, as well as dependence, and opioid prescribing is a contributor to the ongoing opioid epidemic in the United States.7
Given these medications’ utility and potential side effects, urgent care (UC) clinicians must understand the benefits, risks, and potential misconceptions about NSAID administration and prescription. These medications are a mainstay in many healthcare settings for mild to moderate pain and a valuable tool for any UC specialist to alleviate patient discomfort during evaluation.1,7 Despite this, there is a paucity of reviews that are explicitly focused on ambulatory settings, and no studies specifically address the unique setting of UC centers. We aim to characterize the specific evidence-based indications, analyze previous studies on NSAID dosing and route, and compare side effects between these medications and other classes.
We completed a narrative review of MEDLINE using specific search criteria to capture studies of NSAID use in urgent care or emergency departments, indications, and side effects. Overall, we hypothesized numerous uses for these medications. At the same time, there may be misconceptions about the safety and efficacy of NSAIDs compared to acetaminophen, opioids, and other pain medications. This narrative review will help guide urgent care providers in using NSAIDs regularly and effectively to treat their patients’ pain.
Methods
We queried the MEDLINE database on January 24, 2023, to capture studies in this database within the past 10 years. We developed a search strategy using medical subject headings (MeSH) terms to capture urgent care and emergency department studies of NSAID use by including related terms to these care settings and each common NSAID. Duplicate studies were removed, and titles and abstracts were screened using the Rayyan screening application according to specific inclusion and exclusion criteria.8 Types of studies included were randomized controlled trials (RCTs), cohort studies, and systematic reviews with included meta-analyses (SRMA). We considered all studies that compared NSAIDs to other pain medications, assessed the safety of these medications, and compared doses and routes of NSAIDs. Two investigators screened all full-text articles.
Investigators extracted individual study details, including design, setting, primary and secondary outcomes, and the painful complaint. Based on the initial full-text review, the following categories of chief complaint were created to simplify interpretation: trauma/extremity injury; headaches; nontraumatic back pain; abdominal pain (excluding renal colic); and renal colic; and pediatric pain. Data was extracted by one investigator (AH) and verified by a second investigator (CB).
Results
The literature search and abstract screening identified 375 potential studies, and 97 articles were included in full-text screening (Figure 1). Of these, 67 studies were eligible for inclusion in our narrative review. These studies compared the efficacy and safety of NSAIDs and other pain medications, explored specific indications for NSAIDs, and considered side effects and contraindications of NSAIDs.
I. Indications and comparative studies of NSAIDs with other medications
a. Traumatic injury
NSAIDs perform very similarly to opioids and acetaminophen for traumatic pain with fewer side effects than opioids.
One RCT of 411 ED patients with acute extremity pain averaging 8.7 on numeric rating score (NRS) showed no statistical difference in pain reduction at 2 hours between ibuprofen vs 3 different opioid medications combined with acetaminophen (P = 0.53), while a SRMA of 6,128 ED patients with musculoskeletal (MSK) pain also showed no difference in pain reduction with opioids compared to NSAIDs.9,10 Another large RCT (n = 948) of ED patients presenting after motor vehicle collision showed no difference between opioids and NSAIDs in moderate to severe MSK pain at 6 weeks (absolute risk reduction [ARR] = 7.2%; 95% confidence interval [CI]: -5.2, 19.5%), while patients prescribed opioids were more likely to have continued to use of these medications (ARR = 17.5%; 95% CI: 5.8, 29.3%).11 Moreover, in 1 cross-sectional study of 104 ED patients aged 65 and older who were undergoing initiation of analgesic treatment for acute MSK pain, those taking opioids were more likely to have had moderate or severe side effects than those taking only non-opioids (62%, 95% CI = 48% to 74% vs 4%, 95% CI = 1% to 20%) and were also more likely to have discontinued treatment due to side effects like fatigue, nausea and constipation (16%, 95% CI = 8% to 29% vs. 0%, 95% CI = 0% to 13%).12 An observational study comparing ibuprofen and oxycodone in 329 children with isolated fractures found no difference in the mean reduction in pain score (Faces Pain Score-Revised score) on days 1, 2, and 3.13 Lastly, a network meta-analysis of 18 RCTs consisting of 2,656 patients with traumatic MSK pain found that, while no medication class showed a superior analgesic effect than opioids at the 60-minute time point, NSAIDs were the medication class with the highest score for overall effectiveness.14
Conversely, an observational study of 200 patients showed a higher analgesic effect of paracetamol/codeine than ketorolac for fractures and MSK pain (p = 0.044) and a significantly higher effect 2 hours after administration (p = 0.029).15 Another RCT comparing 800 mg ibuprofen to 1g acetaminophen for acute MSK pain found no difference in visual analog scores (VAS) at 1 hour between these treatments (P = 0.59).16 In a similar RCT study (n = 60) comparing oral diclofenac potassium (50 mg) and intravenous acetaminophen (1 g in 500 ml normal saline over 20 minutes), VAS scores between the 2 were assessed and found to have no change (p = 0.11).17 Two more RCT studies (n = 200) each compared 50 mg of IV dexketoprofen to 1 g of IV acetaminophen/paracetamol and found no difference in the VAS score reduction (p = 0.613) for traumatic MSK pain but did show a difference/increased efficacy for dexketoprofen for non-traumatic MSK pain (p = 0.001).18,19
Other modes of administration for NSAID use were also assessed in 2 studies using topical ketoprofen vs placebo for acute ankle sprains.20,21 In both double-blinded RCTs for adults (n = 200) and children (n = 60), VAS pain score reductions were noted to be greater in the topical ketoprofen group vs placebo (16 [9-22], 21 [15-27]a, 20 [13-28] and 35 [29-41]c).20,21 However, a double-blinded study of topical piroxicam vs capsaicin for traumatic pain in the ED showed that the clinical effect of capsaicin was significantly higher (p < 0.01).22
Sublingual use of ketorolac (0.5 mg/kg) vs tramadol (2 mg/kg) was also evaluated in an RCT (n = 131) of pediatric patients with moderate to severe post-traumatic bone pain and found no difference between the two in primary pain reduction at 6 different time intervals up to 120 minutes post-administration.23 Lastly, in an observation study with 824 patients using intranasal NSAIDs vs opioids vs a combination of both, intranasal NSAIDs were found to have a significant change in the maximum pain scores day to day (p < 0.05) with decreased rates of adverse events ( p < 0.001) despite nasal irritation being more common (odds ratio [OR] =3.51, P < 0.0001) and higher satisfaction scores (3.93 vs 2.8).24
b. Headaches
Primary headaches represent a heterogeneous group of disorders. NSAIDs in combination with antiemetics are commonly used to treat migraine headaches. An observational study of 847 cases indicated NSAIDs are the most frequently used class of medications for headaches (81%) compared to antiemetics (43.1%).25 Two studies indicated that combination therapy of NSAIDs with antiemetics led to higher discharge rates than independent administration of each (p < 0.05) and more significant pain relief at 30 minutes (p = 0.025).26,27 However, one RCT of children presenting with headache (n = 53) indicated no difference between metoclopramide alone vs metoclopramide with ketorolac.28 One additional study found dexketoprofen superior to placebo, and a study of 2 tertiary EDs suggested both dopamine antagonists and NSAIDs decreased the need for rescue medications compared to other medications.29,30
An RCT evaluating IV sodium valproate vs IV ibuprofen showed increased pain relief in the sodium valproate group (p < 0.001). A SRMA of 32 trials (n = 321) showed no difference between ketorolac vs meperidine and a phenothiazine agent, but improved pain reduction compared to intranasal sumatriptan.31 Two studies showed no difference in pain outcomes between metoclopramide and ketorolac but indicated more rescue medications were needed for ketorolac.32
c. Atraumatic back pain
Overall, the studies reviewed suggest that NSAIDs perform similarly to opioids for back pain, but with fewer side effects. In an RCT (n = 137) studying the efficacy and safety profile of IV single-dose paracetamol vs dexketoprofen vs morphine in the treatment of lower back pain, there was no significant difference found between all 3 interventions in pain reduction via VAS score.33 There was, however, a higher rate in adverse events in the morphine group.
d. Abdominal pain
Abdominal pain can be caused by a large variety of benign and serious conditions. For non-dyspepsia type abdominal pain, NSAIDs have shown efficacy in several specific and non-specific types of abdominal pain. One systematic review of 12 RCTs (n = 669) found no difference between opioids and NSAIDs in efficacious acute pancreatitis treatment and no significant difference in adverse events.34 Another prospective study of patients with abdominal pain related to pancreatitis showed no difference between acetaminophen, dexketoprofen, and tramadol in pain relief.35 A retrospective cohort study (n = 11,688) found that ketorolac decreased the need for opioids for non-specific abdominal pain compared to haloperidol. Importantly, as NSAIDs are known to produce dyspepsia and upper GI discomfort, this group was not included in this study.36
e. Renal colic
The studies included demonstrated that NSAIDs are more effective than opioids and acetaminophen for renal colic. Five studies assessed the effectiveness of NSAIDs in controlling pain from renal colic. One RCT found that IM diclofenac was equivalent to sterile water injection, while another found that lidocaine nerve block had improved VAS.9,37 Conversely, another RCT found IM diclofenac was more effective in achieving >50% reduction in pain from severe renal colic than IV morphine or IV acetaminophen.38 A similar RCT found that IV dexketoprofen was superior at 30 minutes to IV fentanyl or paracetamol in VAS improvement.39 Finally, a retrospective review indicated NSAIDs and smooth muscle relaxants (ie, alpha-blockers) were the most commonly used medications for renal colic.40
f. Other indications
One double-blinded study showed no difference between ibuprofen, acetaminophen, or a combination of these medications in acute pediatric pain relief at 60 minutes.41 Another study of pediatric and adult patients with viral respiratory infections showed a greater benefit of NSAIDs in the outpatient management of fever and sore throat.42 A randomized equivalence trial showed no difference in pain outcomes or significant adverse events in indomethacin vs prednisolone in gout treatment.43 Another RCT (n = 200) showed no difference in fever reduction or rescue therapy with ibuprofen vs paracetamol.44 Finally, retrospective reviews of sickle cell pain management in the ED showed increased hospitalization with opioids alone vs opioids in combination with NSAIDs (p = 0.0085). Another study indicated more return visits with NSAIDs alone, but no change in opioid prescriptions or readmissions.45,46
II. Dosing and route of administration of NSAIDs
Topical and intramuscular administration of NSAIDs can both be effective, but intramuscular specifically has relatively high rates of local adverse effects. There were 5 studies related to IM injections of NSAIDs in the ED. IM diclofenac was superior to oral diclofenac in achieving 50% reduction in pain at 30 minutes post-administration (absolute risk difference 12.7%).47 Three RCTs compared doses of ketorolac and demonstrated no significant difference in pain relief between 10mg and higher doses (eg, 15mg, 30mg), while higher doses were associated with more burning at the injection site.48–50 One study of 118 patients found an 8.5% incidence of scars, ulcers, and abscesses at the injection site from IM diclofenac.51
Two studies indicated the effectiveness of topical ketoprofen for acute ankle sprains and low back pain in the ED.20,52 In an observational study (n = 28), intranasal ketorolac showed good pain relief, with 32% achieving relief within a median time of 5 minutes.53
Finally, a single-blinded RCT (n = 99) compared scheduled ibuprofen to as-needed dosing and found no difference in pain scores or disability between the groups but slightly higher adverse events in the scheduled group after 4 days of use.54
III. Side effects and contraindications to NSAIDs
a. Post-surgical complications
A case-control study (n=1,503) indicated a reduction in post-operative adverse events with using NSAIDs perioperatively after GI surgery.55 However, 2 additional studies suggest a higher risk of anastomotic failure in colorectal anastomosis with NSAID use and higher odds of reintervention, ED visits, and readmission within 30 days with GI surgery.56,57
b. Gastrointestinal hemorrhage
A cohort study of patients with hemorrhage (n = 517) found that 70.2% of gastrointestinal bleeds were non-variceal and that NSAID use and anticoagulant use were the only independent risk factors for non-variceal bleeds (OR 0.32, 95% CI: 0.13 – 0.83).58 A prospective observational study (n = 67) showed that NSAID use was associated with 31.3% of gastroduodenal ulcers.59 A retrospective study suggested coxib drugs (COX-2 inhibitors) have a lower risk of upper gastrointestinal GI bleeding than other NSAIDs.60
c. Comparison of acetaminophen and ibuprofen side effects in pediatric patients
A systematic review indicated equal safety and tolerability of ibuprofen and paracetamol in children, with ibuprofen showing greater efficacy in treating fever and discomfort.2 Another study of 347 patients found ibuprofen has a lower risk of wheezing as a complication compared with acetaminophen.61 Finally, a retrospective observational study (n = 74,387) found more reported toxic exposure to ibuprofen than acetaminophen among children under 6 years.62 However, acetaminophen overdose unsurprisingly had higher odds of serious, adverse medical outcomes.62
d. Other side effects
One retrospective cohort study (n = 480) suggested there are no increased adverse events (kidney injury, bleeding, transfusion, death) in geriatric patients treated with IV ketorolac.63 A small, retrospective study (n = 117) of cases of drug-induced anaphylaxis suggested that NSAIDs were the most frequent cause.64 Finally, a retrospective study of low-birth-weight neonates receiving prophylactic indomethacin suggested a longer cumulative number of days of mechanical ventilation, supplemental oxygen, and continuous positive airway pressure.65
Discussion
Our study summarizes the pertinent literature on NSAID use in emergency departments and ambulatory settings for acutely painful conditions, which may guide use in UC settings. Many misconceptions remain about the efficacy and safety of NSAIDs compared to other pain medications. Through a systematic process to create a narrative review, our study has explored the efficacy and side effects related to common indications for NSAIDs in urgent or emergent settings. We also examined the route and dosing of these medications to mitigate further risks and improve our understanding of how to dose NSAIDs properly.
The majority of the studies found in this narrative review related to the effectiveness and indications for NSAIDs when compared with other pain medications. Common uses of these medications included traumatic pain, headache, back pain, abdominal pain, fever, and pediatric pain.
Numerous studies compared NSAIDs with opioids for traumatic and musculoskeletal pain, with multiple RCTs and systematic reviews showing no difference in pain relief between these medications acutely but more side effects and continued use with opioids.9–11 Conversely, 1 study showed increased efficacy of opioid/acetaminophen combination compared with ketorolac in fracture pain, and 2 other studies suggested acetaminophen is equally effective while topical capsaicin may be more effective.15,16,22 Overall, given efficacy and side effect profiles, NSAIDs appear preferable over opioid medications, and alternatives such as capsaicin and acetaminophen can also be considered to achieve multimodal analgesia.
Headache was a common indication for NSAID use, and NSAIDs appear to be extremely effective, especially in combination with dopamine antagonist antiemetic medications (eg, metoclopramide).25–27 This review supports NSAID use as first-line for headaches and shows the benefit of these medications compared to non-dopamine antagonists or intravenous fluids.
In atraumatic back pain, a single study showed no difference in pain reduction between acetaminophen, ibuprofen, and morphine with more side effects in the morphine group.33 Given recent RCT data that opioid use in atraumatic low back pain is detrimental to medium-term patient outcomes (OPAL study), NSAIDs are an appropriate choice for first-line treatment in the acute phase of these symptoms, and opioids should be avoided in the routine management of these cases.66 Conversely, a recent Cochrane review indicated there was an improvement in outcomes for patients using NSAIDs for low back pain, but that the magnitude of this improvement was small. 67 Results in renal colic generally favored NSAIDs with 2 other studies demonstrating the superiority of parenteral NSAIDs compared to acetaminophen and opioids.9,37–39
Various other indications were reviewed. NSAIDs were found to have benefits in addition to opioids for sickle cell disease, found equivalent to acetaminophen in pediatric pain, fever, and sore throat, and found equivalent to prednisolone for gout treatment.41–46 These results support the critical role of inclusion of some formulation of an NSAID in the multimodal treatment of nearly all forms of pain. In many cases, these results suggest that an NSAID agent should even be the first line.
This study also reviewed the route and dosing of administering NSAIDs in ED settings. Several studies of ketorolac suggest there is no added analgesic benefit in doses >10 mg.48–50 Importantly, given the frequency with which this medication is used in UC, it’s worth noting that IM ketorolac was associated with a local, often delayed, complication in nearly 10% of patients.51 Despite this, IM diclofenac was somewhat more rapid at achieving a 50% reduction in pain over oral administration.47 Overall, weight-based or pain severity-based dosing of ketorolac is not supported by the evidence in this review, and the side effects of IM injection should be considered when choosing an NSAID. However, IM NSAIDs did show improved pain reduction when compared to oral medications in 1 study,47 and likely still have a role for especially severe pain.
Other routes of administration reviewed included topical and intranasal NSAIDs. Topical ketoprofen was found to be effective in ankle sprains and lower back pain, while intranasal ketorolac showed more rapid and effective pain relief. 20,52,53 These results highlight the viability of topical and intranasal administration of NSAIDs which may be preferable in patients who cannot tolerate oral administration and lack intravenous access. One study looked at the efficacy of scheduled NSAID use compared to as-needed for pediatric ankle sprains and found no significant difference in pain reduction while having a higher rate of reported adverse effects.54 This suggests that the necessity of scheduled dosing should be weighed before recommending this to patients at UC center discharge given the increased risk of adverse effects over pro re nata dosing.
Another aspect of NSAID use studied was the common side effects and contraindications of NSAIDs. These medications are commonly avoided perioperatively out of concern for effects on healing, and 2 studies supported this practice suggesting an increased rate of colocolonic/colorectal anastomoses failure and a slightly increased rate of postoperative complications.56,57 However, these effects appear marginal, and 1 case-control study found that the early use of high-dose NSAIDs was associated with a reduction in overall postoperative adverse events after GI surgery.55 Another study indicated ibuprofen use in post-tonsillectomy leads to fewer ED visits without increasing the risk of hemorrhage.68 Overall, NSAIDs seem to have some effect on postsurgical complications, but that may be limited to GI surgeries and still can be considered as peri-operative pain control.
GI bleeding is another feared complication of NSAID use. This review indicates this caution is warranted as NSAIDs were one of the only independent risk factors for non-variceal upper GI bleeds and were associated with 31.3% of all gastroduodenal ulcers.58,59 COX-2 inhibitors such as celecoxib were found to have a lower association with upper GI bleeds.60 These studies indicate bleeding risk should be assessed before administration of NSAIDs and should be carefully considered in the UC setting before suggesting NSAIDs for pain control at home.
Acetaminophen and ibuprofen are 2 commonly used non-opioid pain medications and are also used as antipyretics in pediatric populations.
Our review found multiple studies assessing differences in efficacy and safety in children. Ibuprofen was found to be equally safe to acetaminophen in children, more effective, and conferred a lower risk of breathing difficulties in another study.2,61 Another large, retrospective study indicated children with toxic exposure to ibuprofen had less chance of a serious medical outcome when compared to acetaminophen.62 Our review suggests that ibuprofen should be considered first line in pediatric patients with pain or fever, and is safe in children over 6 months of age.
Other implications of our review of NSAID toxicity are that ED use of NSAIDs did not increase adverse events in geriatric patients, but NSAIDs are a common cause of drug induced anaphylaxis.63,64 It is important to note that these studies focused on clinical administration of NSAIDs and that serious adverse events were rare. However, NSAIDs are implicated as causal for many adverse effects and even hospitalizations when taken by patients without a clinician’s supervision. This is a critical distinction as administration in the UC setting should be distinguished from what is safe for patients to continue at home.69
This study has multiple limitations, including the narrowed inclusion of only studies conducted in emergent/urgent settings. There are many studies of indications and side effects of NSAIDs performed in other clinical environments that should be considered when deciding to use them in urgent care settings. In addition, a narrative review does not include an analysis of the evidence or meta-analysis, and the studies were quite heterogeneous in their outcomes.
Conclusion
NSAIDs appear to be a safe, effective option that should be considered alongside acetaminophen for most acute painful conditions in the UC setting. NSAIDs generally show equivalent or superior pain relief when compared to opioids with fewer side effects for most indications. NSAIDs show efficacy in headache, back pain, and renal colic treatment. The predominant side effects that should be considered for UC-based administration include GI hemorrhage and anaphylaxis. However, ED use of appropriate doses of NSAIDs for acute pain did not cause significant adverse renal outcomes in geriatric patients. Additionally, alternate routes of administration have also been shown to offer significant pain relief; most notably topical and intranasal NSAIDs appear to be effective alternatives when IV or oral NSAIDs are not accessible or deemed to be safe. This review confirms the important role the NSAID class of medications can play in the acute management of pain in urgent care and emergency department settings.
Manuscript submitted September 9, 2022; accepted February 15, 2024.
References
- Optimizing the Treatment of Acute Pain in the Emergency Department. (2017). Annals of emergency medicine, 70(3), 446–448. https://doi.org/10.1016/j.annemergmed.2017.06.043.
- Kanabar D. J. (2017). A clinical and safety review of paracetamol and ibuprofen in children. Inflammopharmacology, 25(1), 1–9. https://doi.org/10.1007/s10787-016-0302-3.
- Cisewski, D. H., Motov, S. M. (2018). Essential pharmacologic options for acute pain management in the emergency setting. Turkish journal of emergency medicine, 19(1), 1–11. https://doi.org/10.1016/j.tjem.2018.11.003.
- Ghlichloo I, Gerriets V. Nonsteroidal Anti-inflammatory Drugs (NSAIDs) [Updated 2022 May 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023.
- Pirmohamed, M., James, S., Meakin, S., Green, C., Scott, A. K., Walley, T. J., Farrar, K., Park, B. K., Breckenridge, A. M. (2004). Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ (Clinical research ed.), 329(7456), 15–19. https://doi.org/10.1136/bmj.329.7456.15.
- Davis, A., Robson, J. (2016). The dangers of NSAIDs: look both ways. The British journal of general practice : the journal of the Royal College of General Practitioners, 66(645), 172–173. https://doi.org/10.3399/bjgp16X684433.
- Almehlisi, A., Tainter, C. (2019). Emergency department pain management: beyond opioids. Emergency medicine practice, 21(11), 1–24.
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan-a web and mobile app for systematic reviews. Systematic reviews, 5(1), 210. https://doi.org/10.1186/s13643-016-0384-4.
- Moussa, M., Papatsoris, A. G., & Chakra, M. A. (2021). Intradermal sterile water injection versus diclofenac sodium in acute renal colic pain: A randomized controlled trial. The American journal of emergency medicine, 44, 395–400. https://doi.org/10.1016/j.ajem.2020.04.079.
- Jones, C. M. P., Lin, C. C., Jamshidi, M., Abdel Shaheed, C., Maher, C. G., Harris, I. A., Patanwala, A. E., Dinh, M., & Mathieson, S. (2022). Effectiveness of Opioid Analgesic Medicines Prescribed in or at Discharge From Emergency Departments for Musculoskeletal Pain : A Systematic Review and Meta-analysis. Annals of internal medicine, 175(11), 1572–1581. https://doi.org/10.7326/M22-2162.
- Beaudoin, F. L., Gutman, R., Merchant, R. C., Clark, M. A., Swor, R. A., Jones, J. S., Lee, D. C., Peak, D. A., Domeier, R. M., Rathlev, N. K., & McLean, S. A. (2017). Persistent pain after motor vehicle collision: comparative effectiveness of opioids vs nonsteroidal antiinflammatory drugs prescribed from the emergency department-a propensity matched analysis. Pain, 158(2), 289–295. https://doi.org/10.1097/j.pain.0000000000000756.
- Hunold, K. M., Esserman, D. A., Isaacs, C. G., Dickey, R. M., Pereira, G. F., Fillingim, R. B., Sloane, P. D., McLean, S. A., & Platts-Mills, T. F. (2013). Side effects from oral opioids in older adults during the first week of treatment for acute musculoskeletal pain. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine, 20(9), 872–879. https://doi.org/10.1111/acem.12212.
- Ali, S., Manaloor, R., Johnson, D. W., Rosychuk, R. J., LeMay, S., Carleton, B., McGrath, P. J., Drendel, A. L., & Pediatric Emergency Research Canada (2021). An observational cohort study comparing ibuprofen and oxycodone in children with fractures. PloS one, 16(9), e0257021. https://doi.org/10.1371/journal.pone.0257021.
- Yin, X., Wang, X., & He, C. (2021). Comparative efficacy of therapeutics for traumatic musculoskeletal pain in the emergency setting: A network meta-analysis. The American journal of emergency medicine, 46, 424–429. https://doi.org/10.1016/j.ajem.2020.10.038.
- Buccelletti, F., Marsiliani, D., Zuccalà, G., Iacomini, P., Proietti, L., Pola, E., Zirio, G., Genitiempo, M., Marrocco, R., Conti, C., Brunetti, C., Rocchi, L., Merendi, G., D’Aurizio, G., Gilardi, E., & Franceschi, F. (2014). Paracetamol-codeine compared to ketorolac for pain control in the Emergency Department. European review for medical and pharmacological sciences, 18(20), 3139–3143.
- Bondarsky, E. E., Domingo, A. T., Matuza, N. M., Taylor, M. B., Thode, H. C., Jr, & Singer, A. J. (2013). Ibuprofen vs acetaminophen vs their combination in the relief of musculoskeletal pain in the ED: a randomized, controlled trial. The American journal of emergency medicine, 31(9), 1357–1360. https://doi.org/10.1016/j.ajem.2013.06.007.
- Momeni, M., Vahidi, E., Badrizadeh, M., Naderpour, Z., & Saeedi, M. (2019). Oral Diclofenac Potassium Versus Intravenous Acetaminophen in Acute, Isolated, Closed-Limb Trauma. Advanced emergency nursing journal, 41(1), 48–55. https://doi.org/10.1097/TME.0000000000000224.
- Yilmaz, A., Sabirli, R., Ozen, M., Turkcuer, I., Erdur, B., Arikan, C., Demirozogul, E., Sarohan, A., Seyit, M., & Ok, N. (2019). Intravenous paracetamol versus dexketoprofen in acute musculoskeletal trauma in the emergency department: A randomised clinical trial. The American journal of emergency medicine, 37(5), 902–908. https://doi.org/10.1016/j.ajem.2018.08.023.
- Demirozogul, E., Yilmaz, A., Ozen, M., Turkcuer, I., Seyit, M., & Arikan, C. (2019). Intravenous dexketoprofen versus paracetamol in non-traumatic musculoskeletal pain in the emergency department: A randomized clinical trial. The American journal of emergency medicine, 37(12), 2136–2142. https://doi.org/10.1016/j.ajem.2019.01.040.
- Serinken, M., Eken, C., & Elicabuk, H. (2016). Topical Ketoprofen Versus Placebo in Treatment of Acute Ankle Sprain in the Emergency Department. Foot & ankle international, 37(9), 989–993. https://doi.org/10.1177/1071100716650530.
- Serinken, M., Eken, C., Tunay, K., & Golcuk, Y. (2016). Ketoprofen gel improves low back pain in addition to IV dexketoprofen: a randomized placebo-controlled trial. The American journal of emergency medicine, 34(8), 1458–1461. https://doi.org/10.1016/j.ajem.2016.04.028.
- Kocak, A. O., Dogruyol, S., Akbas, I., Menekse, T. S., Gur, S. T. A., Kocak, M. B., Cekmen, B., Orun, S., & Cakir, Z. (2020). Comparison of topical capsaicin and topical piroxicam in the treatment of acute trauma-induced pain: A randomized double-blind trial. The American journal of emergency medicine, 38(9), 1767–1771. https://doi.org/10.1016/j.ajem.2020.05.104.
- Neri, E., Maestro, A., Minen, F., Montico, M., Ronfani, L., Zanon, D., Favret, A., Messi, G., & Barbi, E. (2013). Sublingual ketorolac versus sublingual tramadol for moderate to severe post-traumatic bone pain in children: a double-blind, randomised, controlled trial. Archives of disease in childhood, 98(9), 721–724. https://doi.org/10.1136/archdischild-2012-303527.
- Pollack, C. V., Jr, Diercks, D. B., Thomas, S. H., Shapiro, N. I., Fanikos, J., Mace, S. E., Rafique, Z., & Todd, K. H. (2016). Patient-reported Outcomes from A National, Prospective, Observational Study of Emergency Department Acute Pain Management With an Intranasal Nonsteroidal Anti-inflammatory Drug, Opioids, or Both. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine, 23(3), 331–341. https://doi.org/10.1111/acem.12902.
- Navarro-Pérez, M. P., Ballesta-Martínez, S., Rodríguez-Montolio, J., Bellosta-Diago, E., García-Noaín, J. A., & Santos-Lasaosa, S. (2021). Acute migraine management in the emergency department: experience from a large Spanish tertiary hospital. Internal and emergency medicine, 16(8), 2243–2249. https://doi.org/10.1007/s11739-021-02698-9.
- Yavuz, E., Gulacti, U., Lok, U., & Turgut, K. (2020). Intravenous metoclopramide versus dexketoprofen trometamol versus metoclopramide+ dexketoprofen trometamol in acute migraine attack in the emergency department: A randomized double-blind controlled trial. The American journal of emergency medicine, 38(11), 2254–2258. https://doi.org/10.1016/j.ajem.2020.04.038.
- Aravamuthan, B. R., Mar, S. S., & Williams, K. G. (2017). Factors Associated With Discharge After Initial Emergency Treatment of Pediatric Migraine. Pediatric emergency care, 33(9), 620–629. https://doi.org/10.1097/PEC.0000000000000533.
- Richer, L. P., Ali, S., Johnson, D. W., Rosychuk, R. J., Newton, A. S., & Rowe, B. H. (2022). A randomized trial of ketorolac and metoclopramide for migraine in the emergency department. Headache, 62(6), 681–689. https://doi.org/10.1111/head.14307.
- Gungor, F., Akyol, K. C., Kesapli, M., Celik, A., Karaca, A., Bozdemir, M. N., & Eken, C. (2016). Intravenous dexketoprofen vs placebo for migraine attack in the emergency department: A randomized, placebo-controlled trial. Cephalalgia : an international journal of headache, 36(2), 179–184. https://doi.org/10.1177/0333102415584604.
- Wells, S., Stiell, I. G., Vishnyakova, E., Lun, R., Nemnom, M. J., & Perry, J. J. (2021). Optimal management strategies for primary headache in the emergency department. CJEM, 23(6), 802–811. https://doi.org/10.1007/s43678-021-00173-0.
- Taggart, E., Doran, S., Kokotillo, A., Campbell, S., Villa-Roel, C., & Rowe, B. H. (2013). Ketorolac in the treatment of acute migraine: a systematic review. Headache, 53(2), 277–287. https://doi.org/10.1111/head.12009.
- Soltani, K. M., Motamed, H., Eslami, K., Majdinasab, N., & Kouti, L. (2021). Randomised trial of IV metoclopramide vs IV ketorolac in treatment of acute primary headaches. The American journal of emergency medicine, 50, 376–380. https://doi.org/10.1016/j.ajem.2021.08.023.
- Eken, C., Serinken, M., Elicabuk, H., Uyanik, E., & Erdal, M. (2014). Intravenous paracetamol versus dexketoprofen versus morphine in acute mechanical low back pain in the emergency department: a randomised double-blind controlled trial. Emergency medicine journal : EMJ, 31(3), 177–181. https://doi.org/10.1136/emermed-2012-201670.
- Cai, W., Liu, F., Wen, Y., Han, C., Prasad, M., Xia, Q., Singh, V. K., Sutton, R., & Huang, W. (2021). Pain Management in Acute Pancreatitis: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Frontiers in medicine, 8, 782151. https://doi.org/10.3389/fmed.2021.782151.
- Gülen, B., Dur, A., Serinken, M., Karcıoğlu, Ö., & Sönmez, E. (2016). Pain treatment in patients with acute pancreatitis: A randomized controlled trial. The Turkish journal of gastroenterology : the official journal of Turkish Society of Gastroenterology, 27(2), 192–196. https://doi.org/10.5152/tjg.2015.150398.
- Heard, K., Bebarta, V. S., Hoppe, J. A., & Monte, A. A. (2020). Does administration of haloperidol or ketorolac decrease opioid administration for abdominal pain patients? A retrospective study. The American journal of emergency medicine, 38(3), 517–520. https://doi.org/10.1016/j.ajem.2019.05.038.
- Seyhan, A. U., & Yılmaz, E. (2021). Treatment of Renal Colic by Nerve Blockade with Lidocaine Versus Intravenous Dexketoprofen. Journal of the College of Physicians and Surgeons–Pakistan : JCPSP, 31(8), 921–925. https://doi.org/10.29271/jcpsp.2021.08.921.
- Pathan, S. A., Mitra, B., Straney, L. D., Afzal, M. S., Anjum, S., Shukla, D., Morley, K., Al Hilli, S. A., Al Rumaihi, K., Thomas, S. H., & Cameron, P. A. (2016). Delivering safe and effective analgesia for management of renal colic in the emergency department: a double-blind, multigroup, randomised controlled trial. Lancet (London, England), 387(10032), 1999–2007. https://doi.org/10.1016/S0140-6736(16)00652-8.
- Al, B., Sunar, M. M., Zengin, S., Sabak, M., Bogan, M., Can, B., Kul, S., Murat Oktay, M., & Eren, S. H. (2018). Comparison of IV dexketoprofen trometamol, fentanyl, and paracetamol in the treatment of renal colic in the ED: A randomized controlled trial. The American journal of emergency medicine, 36(4), 571–576. https://doi.org/10.1016/j.ajem.2017.09.019.
- Shrestha, R., Bista, Y., & Khan, A. (2017). Current Diagnostic Approach and Initial Treatment Patterns for Renal Colic in Emergency Department. Journal of Nepal Health Research Council, 15(1), 38–43. https://doi.org/10.3126/jnhrc.v15i1.18012.
- Motov, S., Butt, M., Masoudi, A., Palacios, W., Fassassi, C., Drapkin, J., Likourezos, A., Hossain, R., Brady, J., Rothberger, N., Flom, P., Zerzan, J., & Marshall, J. (2020). Comparison of Oral Ibuprofen and Acetaminophen with Either Analgesic Alone for Pediatric Emergency Department Patients with Acute Pain. The Journal of emergency medicine, 58(5), 725–732. https://doi.org/10.1016/j.jemermed.2020.02.010.
- Azh, N., Barzkar, F., Motamed-Gorji, N., Pourvali-Talatappeh, P., Moradi, Y., Vesal Azad, R., Ranjbar, M., & Baradaran, H. R. (2022). Nonsteroidal anti-inflammatory drugs in acute viral respiratory tract infections: An updated systematic review. Pharmacology research & perspectives, 10(2), e00925. https://doi.org/10.1002/prp2.925.
- Rainer, T. H., Cheng, C. H., Janssens, H. J., Man, C. Y., Tam, L. S., Choi, Y. F., Yau, W. H., Lee, K. H., & Graham, C. A. (2016). Oral Prednisolone in the Treatment of Acute Gout: A Pragmatic, Multicenter, Double-Blind, Randomized Trial. Annals of internal medicine, 164(7), 464–471. https://doi.org/10.7326/M14-2070.
- Can, Ö., Kıyan, G. S., & Yalçınlı, S. (2021). Comparison of intravenous ibuprofen and paracetamol in the treatment of fever: A randomized double-blind study. The American journal of emergency medicine, 46, 102–106. https://doi.org/10.1016/j.ajem.2021.02.057.
- Okorji, L. M., Muntz, D. S., & Liem, R. I. (2017). Opioid prescription practices at discharge and 30-day returns in children with sickle cell disease and pain. Pediatric blood & cancer, 64(5), 10.1002/pbc.26319. https://doi.org/10.1002/pbc.26319.
- Cacciotti, C., Vaiselbuh, S., & Romanos-Sirakis, E. (2017). Pain Management for Sickle Cell Disease in the Pediatric Emergency Department: Medications and Hospitalization Trends. Clinical pediatrics, 56(12), 1109–1114. https://doi.org/10.1177/0009922816674521.
- Qureshi, I., Pathan, S. A., Qureshi, R. S., & Thomas, S. H. (2019). Intramuscular versus oral diclofenac for acute pain in adults with acute musculoskeletal injuries presenting to the ED setting: a prospective, double-blind, double-dummy, randomised controlled trial. Emergency medicine journal : EMJ, 36(7), 401–406. https://doi.org/10.1136/emermed-2018-208214.
- Turner, N. J., Long, D. A., Bongiorno, J. R., Katoski, T. P., Jin, L. M., Horsch, J. P., & Ahern, B. J. (2021). Comparing two doses of intramuscular ketorolac for treatment of acute musculoskeletal pain in a military emergency department. The American journal of emergency medicine, 50, 142–147. https://doi.org/10.1016/j.ajem.2021.07.054.
- Eidinejad, L., Bahreini, M., Ahmadi, A., Yazdchi, M., Thiruganasambandamoorthy, V., & Mirfazaelian, H. (2021). Comparison of intravenous ketorolac at three doses for treating renal colic in the emergency department: A noninferiority randomized controlled trial. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine, 28(7), 768–775. https://doi.org/10.1111/acem.14202.
- Shanechi, M., Eke, O., & Gottlieb, M. (2018). Comparison of ketorolac dosing in an emergency department setting. CJEM, 20(S2), S74–S77. https://doi.org/10.1017/cem.2017.431.
- Tarloff, D., Lamacraft, G., & Joubert, G. (2017). The prevalence of skin scars in patients previously given intramuscular diclofenac injections attending the Pain Clinic at Universitas Academic Hospital, Bloemfontein, South Africa. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde, 107(2), 101–105. https://doi.org/10.7196/SAMJ.2017.v107i2.12012.
- Serinken, M., Eken, C., Tünay, K., & Gölcük, Y. (2020). Topical Ketoprofen Versus Placebo in Children Presenting With Ankle Sprain to the Emergency Department: A Randomized Controlled Study. Pediatric emergency care, 36(8), e447–e450. https://doi.org/10.1097/PEC.0000000000001595.
- Gaul, E., Barbour, T., Nowacki, A. S., & Mace, S. E. (2022). Intranasal Ketorolac for Acute Pain in Adult Emergency Department Patients. Western journal of nursing research, 44(11), 1047–1056. https://doi.org/10.1177/01939459211030336.
- Lim, R., Sangha, G., Lepore, N., Bartlett, K. M., Seabrook, J. A., & Rieder, M. (2020). Comparison of Regularly Scheduled Ibuprofen Versus “Pro Re Nata” for Ankle Sprains in Children Treated in the Emergency Department: A Randomized Controlled Trial. Pediatric emergency care, 36(12), 559–563. https://doi.org/10.1097/PEC.0000000000002282.
- STARSurg Collaborative (2014). Impact of postoperative non-steroidal anti-inflammatory drugs on adverse events after gastrointestinal surgery. The British journal of surgery, 101(11), 1413–1423. https://doi.org/10.1002/bjs.9614.
- Haddad, N. N., Bruns, B. R., Enniss, T. M., Turay, D., Sakran, J. V., Fathalizadeh, A., Arnold, K., Murry, J. S., Carrick, M. M., Hernandez, M. C., Lauerman, M. H., Choudhry, A. J., Morris, D. S., Diaz, J. J., Phelan, H. A., Zielinski, M. D., & NSAIDs SHAPES Workgroup (2017). Perioperative use of nonsteroidal anti-inflammatory drugs and the risk of anastomotic failure in emergency general surgery. The journal of trauma and acute care surgery, 83(4), 657–661. https://doi.org/10.1097/TA.0000000000001583.
- Kotagal, M., Hakkarainen, T. W., Simianu, V. V., Beck, S. J., Alfonso-Cristancho, R., & Flum, D. R. (2016). Ketorolac Use and Postoperative Complications in Gastrointestinal Surgery. Annals of surgery, 263(1), 71–75. https://doi.org/10.1097/SLA.0000000000001260.
- Matei, D., Groza, I., Furnea, B., Puie, L., Levi, C., Chiru, A., Cruciat, C., Mester, G., Vesa, S. C., & Tantau, M. (2013). Predictors of variceal or nonvariceal source of upper gastrointestinal bleeding. An etiology predictive score established and validated in a tertiary referral center. Journal of gastrointestinal and liver diseases : JGLD, 22(4), 379–384.
- Begovic, G., & Selmani, R. (2015). Etiological Factors in Urgent Gastroduodenal Ulcer. Prilozi (Makedonska akademija na naukite i umetnostite. Oddelenie za medicinski nauki), 36(2), 203–210. https://doi.org/10.1515/prilozi-2015-0068.
- Hallas, J., & Pottegård, A. (2017). Performance of the High-dimensional Propensity Score in a Nordic Healthcare Model. Basic & clinical pharmacology & toxicology, 120(3), 312–317. https://doi.org/10.1111/bcpt.12716.
- Matok, I., Elizur, A., Perlman, A., Ganor, S., Levine, H., & Kozer, E. (2017). Association of Acetaminophen and Ibuprofen Use With Wheezing in Children With Acute Febrile Illness. The Annals of pharmacotherapy, 51(3), 239–244. https://doi.org/10.1177/1060028016678006.
- Rakowsky, S., Spiller, H. A., Casavant, M. J., Chounthirath, T., Hodges, N. L., Kim, E. H., & Smith, G. A. (2018). Antipyretic Medication Exposures Among Young Children Reported to US Poison Centers, 2000-2015. Clinical pediatrics, 57(3), 266–276. https://doi.org/10.1177/0009922817698124.
- Anderson, G. L., Mattson, A. E., Brown, C. S., Cabrera, D., Mara, K. C., & Bellolio, M. F. (2020). Safety of parenteral ketorolac use for analgesia in geriatric emergency department patients. The American journal of emergency medicine, 38(4), 727–730. https://doi.org/10.1016/j.ajem.2019.06.009.
- Aun, M. V., Blanca, M., Garro, L. S., Ribeiro, M. R., Kalil, J., Motta, A. A., Castells, M., & Giavina-Bianchi, P. (2014). Nonsteroidal anti-inflammatory drugs are major causes of drug-induced anaphylaxis. The journal of allergy and clinical immunology. In practice, 2(4), 414–420. https://doi.org/10.1016/j.jaip.2014.03.014.
- Mondal, T., Chaudhuri, D., Li, B., Shivananda, S., & Dutta, S. (2014). Prophylactic indomethacin worsens short-term respiratory outcomes in extremely low-birth-weight infants. American journal of perinatology, 31(1), 61–67. https://doi.org/10.1055/s-0033-1334449.
- Williamson, E., Sanchez Santos, M. T., Morris, A., Garrett, A., Conway, O., Boniface, G., Fairbank, J., & Lamb, S. E. (2021). The Prevalence of Back and Leg Pain and the Cross-sectional Association With Adverse Health Outcomes in Community Dwelling Older Adults in England. Spine, 46(1), 54–61. https://doi.org/10.1097/BRS.0000000000003719.
- van der Gaag WH, Roelofs PD, Enthoven WT, van Tulder MW, Koes BW. Non-steroidal anti-inflammatory drugs for acute low back pain. Cochrane Database Syst Rev. 2020 Apr 16;4(4):CD013581. doi: 10.1002/14651858.CD013581.
- Mast, G., Henderson, K., & Carr, M. M. (2020). The Effect of Ibuprofen Dosing Interval on Post-Tonsillectomy Outcomes in Children: A Quality Improvement Study. The Annals of otology, rhinology, and laryngology, 129(12), 1210–1214. https://doi.org/10.1177/0003489420934843.
- Rahme, E., Joseph, L., Kong, S. X., Watson, D. J., & LeLorier, J. (2001). Cost of prescribed NSAID-related gastrointestinal adverse events in elderly patients. British journal of clinical pharmacology, 52(2), 185–192. https://doi.org/10.1046/j.1365-2125.2001.00348.x.
Author Affiliations: Campbell Belisle Haley, MD, Department of Emergency Medicine, University of California, Irvine Medical Center, Orange, California. Andy T. Hsueh, MD, Department of Emergency Medicine, University of California, Irvine Medical Center, Orange, California. Chih-Hsuan Chen, MD, College of Medicine, Kaohsiung Medical University, Kaohsiung City, Taiwan. Ariana M. Nelson, MD, Department of Anesthesiology, Division of Pain Medicine, University of California, Irvine Medical Center, Orange, California.
Read More
- Management Of Patients On Low-Dose Naltrexone: A Clinical Review For Urgent Care Providers
- More Than A Simple Headache: Using The SNNOOP10 Criteria To Screen For Life-Threatening Headache Presentations
- Case Report Of Renal Cell Carcinoma Presenting To Urgent Care With Indolent Back Pain: A Wolf In Sheep’s Clothing
