Published on
Urgent Message: Pediatric emergency medicine researchers have an opportunity to enhance collaboration with general emergency medicine and acute care clinicians to bridge the gap between research and dissemination of evidence-based care recommendations.
Bashar S. Shihabuddin, MD, MS, FAAP, FACEP; Jessica Fritter, MACPR, ACRP-CP; Charmaine B. Lo, PhD MPH; Rachel Stanley MD, MHSA; Michael Weinstock, MD
Citation: Shihabuddin B, Fritter J, Lo C, Stanley R, Weinstock M. Pediatric Knowledge Needs Assessment: A Pilot Study. J Urgent Care Med. 2023;18 (3); 40-43
Abstract
Objectives: We conducted a pilot pediatric knowledge needs assessment survey of providers at a general academic emergency department (ED) within the catchment area of an academic, tertiary care children’s hospital.
Methods: We developed a 22-question electronic survey that was validated by combined emergency medicine and pediatric emergency medicine faculty members at the regional children’s hospital. Three reminders were sent to the respondent pool at 2, 4, and 8 weeks after the initial survey. Reponses were analyzed using descriptive statistics.
Results: A total of 18 surveys were completed. Most respondents were trainees with less than 5 years’ experience working in emergency medicine. The most frequently used methods to access information reported by all respondents were websites with a medical or health focus, spending on average 1-5 hours weekly gathering that information. Faculty were more likely to use a laptop or desktop computer to access that information, while trainees were more likely to use a smartphone. All respondents reported that accessible evidence-based clinical practice guidelines and information regarding novel diagnostics and therapeutics in pediatrics were the most relevant items to enhance their clinical practice. Information on pediatric trauma, sepsis, and neurological emergencies were rated as the highest priorities for clinical care in their practice.
Conclusion: Our findings can guide future knowledge needs assessments to develop dissemination and implementation efforts of evidence-based guidelines in the acute care of children in general EDs.
Introduction
The majority of emergency department (ED) visits by children in the United States are to local community EDs.1 Previous studies have shown that community EDs often lack the proper equipment and specialized personnel to care for pediatric patients.2 Most patients referred to the emergency department from the urgent care are discharged, and the odds of nonacute transfer is lower in a pediatric urgent care than a general urgent care.3 The care children receive in community urgent cares and EDs may not be supported by the latest evidence.4
There is a gap between the generation of evidence-based recommendations for pediatric emergency and acute care and its implementation.5 Greater collaboration efforts between pediatric emergency medicine (PEM) researchers and general emergency medicine (EM) and acute care clinicians may help bridge the gap between research and dissemination of evidence-based care recommendations. Establishing the knowledge needs of providers that would impact patient care, as well as the methods to address those needs, would guide dissemination and implementation efforts of PEM researchers.
Our aim was to assess the knowledge needs of general practice EM providers with an ultimate goal that this assessment could lead to interventions that might enhance care of pediatric patients provided by nonpediatric emergency medicine trained clinicians. We also sought to use the data with the hopes of better understanding about how the participants engage with medical reference resources to determine the optimum method to deliver this PEM-specific knowledge. We planned and conducted a collaborative needs assessment pilot project between an academic quaternary care pediatric ED and an academic ED located in a rural area.
Methods
This was a survey study of clinicians at an academic regional medical center serving a rural community located 40 miles south of a quaternary care dedicated pediatric hospital. The survey was developed by the authors, based on previous work by the Canadian Translating Emergency Knowledge of Kids (TREKK) network, which has an established track record of successful dissemination and implementation in pediatric emergency care.6 The survey was adapted to practice elements relevant in the United States (ie, differences in graduate medical education and practice settings). The survey questions were validated by three faculty members board certified in general and pediatric emergency medicine.
Selection of Participants
The study was approved by the Institutional Review Board, with stipulation for verbal consent from survey participants. The survey was circulated electronically to 41 emergency medicine providers including attending physicians, advanced practice providers, and resident physicians. Three reminders were sent to the respondent pool at 2, 4, and 8 weeks after the initial survey.
Data Analysis
Reponses were analyzed using descriptive statistics.
Results
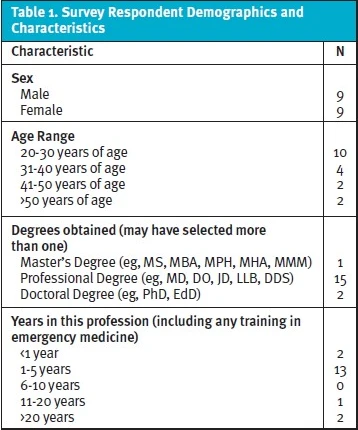
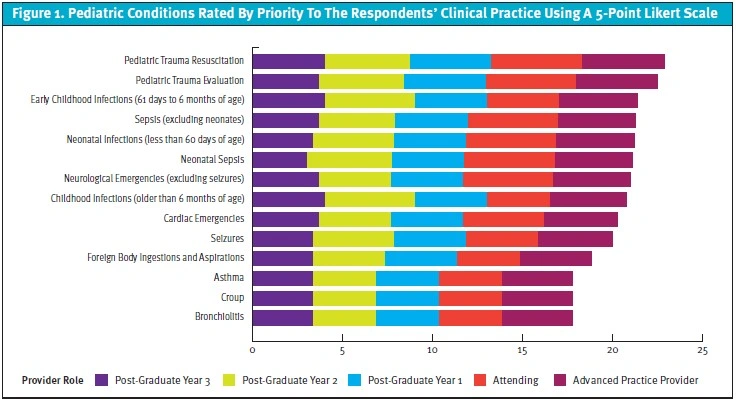
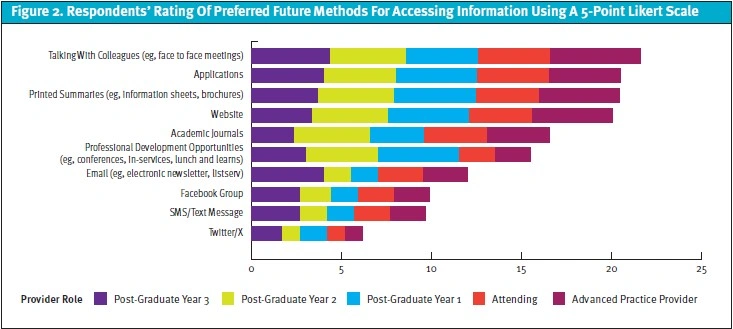
A total of 20 surveys (48.8%) were initiated, 18 surveys (44%) were completed, and 2 surveys were partially completed. Only complete survey responses were included in the final analysis. The demographics of the respondents are listed in Table 1. The respondents included 13 with an osteopathic doctorate, 11 respondents were resident trainees, and most respondents had less than 5 years’ experience working in emergency medicine. All respondents reported currently using websites with a medical or health focus as the most frequent method to find information to care for children in the ED, spending 1-5 hours weekly gathering that information. Faculty were more likely to use a laptop or desktop computer to access information, while trainees were more likely to use a smartphone. All respondents found that accessible evidence-based clinical practice guidelines and information regarding novel diagnostics and therapeutics as the most relevant items to enhance their clinical practice. Respondents identified information on the emergency care of infants below 1 year of age as most relevant to their practice. Information on pediatric trauma, sepsis and early childhood infections were rated as the highest priorities for clinical care (Figure 1). Most respondents preferred mobile applications and formal discussions with colleagues for future access to updated information (Figure 2).
Discussion
General emergency medicine practitioners provide most of the initial emergency and acute care to children in the United States and need to have comfort with rapidly accessing relevant resources for the provision of acute care for pediatric patients.1 Research conducted solely in pediatric EDs lacks practical relevance as general EM practitioners in nonpediatric specialty EDs face a different challenges within their clinical environments. Collaboration between EM practitioners and PEM researchers is necessary to determine how to implement evidence-based guidelines and practice within the context of the most commonly encountered clinical scenario (ie, in a general ED).
Gerber et al. found that the rate of head computed tomography (CT) in pediatric head injuries was not significantly impacted after the Pediatric Emergency Care Applied Research Network (PECARN) risk stratification guidelines were published.7 Similarly, Hess et al. conducted a cluster randomized trial in seven geographically diverse EDs found that the use of the PECARN guidelines increased parent knowledge, decreased decisional conflict, and increased involvement in decision-making, but did not significantly reduce the head CT rate.8 Doran et al found an exceeding low rate of positive CT scan in patients presenting to the urgent care with head injuries and were then transferred to the ED.9 Unfortunately, we are not aware of a head injury clinical decision pathway specific to urgent care patients. These studies suggest that even now, the divide between PEM researchers and community practitioners remains substantial.
Respondents in our cohort were specifically interested in resources on pediatric trauma, sepsis, and neurological conditions. These conditions result in significant mortality and morbidity in pediatric patients and are high-priority research areas. Resources on the care of infants below 1 year of age were rated as highly impactful to clinical practice in our study, which aligns with priorities identified by the American College of Emergency Physicians for pediatric readiness in general EDs.10 Previous studies have found variation in the care infants receive in general emergency departments compared to pediatric EDs, and decreasing comfort among EM practitioners caring for children with decreasing age.11,12 Therefore, increasing dissemination of evidence-based care guidelines would harmonize the care infants receive, regardless of the setting.
The different preferences for accessing medical information emphasizes the need for developing different strategies for dissemination of research findings and recommendations. A possible solution is developing websites linked to mobile applications, so they can be accessed either on a computer or smartphone. Accessing mobile applications may enhance the speed with which this information is recovered, often while the clinician is engaged in patient care, which has the potential to change the trajectory of that child’s care and recovery. Another option would be to incorporate guidelines and clinical decision tools into electronic health records, which would facilitate rapid access by clinicians.
Limitations
Our study had notable limitations that warrant discussion. This was a single-center pilot study with a small sample size and low response rate, and most of the respondents were trainees. The trainees had a wide range of prior training and may not be a representative sample. The residents did rotations in a pediatric ED, and answers may have been different for physicians without this experience. The site of the study was an academic ED, so our findings may not translate to all community EDs. Future knowledge needs assessments would ideally include EDs in multiple geographic and practice settings and nonphysician clinicians (eg, nurse practitioners and physician assistants). Additionally, it is unclear as to how this data might apply to acute care practitioners caring for children in urgent care settings.
Conclusion
Assessments regarding how providers seek knowledge and apply evidence-based guidelines for pediatric emergency care can inform how resources are created and made available. Our findings can guide future research on knowledge needs assessment to promote the dissemination and implementation of evidence-based practices in the acute care of children in all emergency settings.
Manuscript submitted February 3, 2023; accepted October 24, 2023.
Author Affiliations: Bashar S. Shihabuddin, MD, MS, FAAP, FACEP, Nationwide Children’s Hospital, Columbus, Ohio. Jessica Fritter, MACPR, ACRP-CP, College of Nursing, The Ohio State University, Columbus, Ohio. Charmaine B. Lo, PhD MPH, Nationwide Children’s Hospital, Columbus, Ohio. Rachel Stanley MD, MHSA, Nationwide Children’s Hospital, Columbus, Ohio. Michael Weinstock, MD, Adena Health System, Wexner Medical Center at The Ohio State University, Columbus, Ohio, The Journal of Urgent Care Medicine.
Download the article PDF: Pediatric Knowledge Needs Assessment: A Pilot Study

