Urgent message: Appreciation for the cause of knee pain, along with an understanding of potential nonoperative rehabilitation therapies that could be provided in urgent care, can enhance patient care and improve patient satisfaction while minimizing the need for referral.
Dr. Eva Delgado Martinez MBChB, GP, MScCN and Dr. Ivan Koay MBChB, FRNZCUC, MD
INTRODUCTION
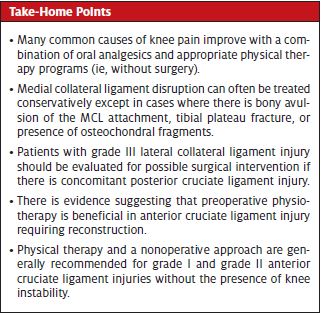
Knee injuries in adults and children are common presentations to urgent care and emergency rooms.1 Rehabilitation of those injuries is essential in aiding patients to return to normal function and activities. Many common causes of knee pain improve with a combination of oral analgesics and appropriate physical therapy programs.
Postinjury, physical therapy aids in the recovery process by facilitating improvements in the effects of pain, range of motion, muscle performance, functional ability, and invariably the patient’s quality of life. Physical therapy has been shown to be crucial in improving short- and long-term outcomes. There remains controversy, however, regarding when physical therapy should be initiated and how certain aspects of the therapy are instituted.2 Optimal clinical outcomes are dependent on a collaborative multidisciplinary approach that involves the primary physician (UC/ED), orthopedic surgeon, physiotherapist, patient, and other healthcare professionals involved in the patient’s care. The use of adjunct treatment such as splints can be considered. However, the effectiveness of knee braces for chronic knee pain is uncertain, and the use of braces should not replace physical therapy3
This article will look at the various types of knee injuries that present to the urgent care clinics and the role of physical therapy as part of the postinjury rehabilitation process or presurgical conditioning to enable patients to have better recovery postprocedure. We will also look at the latest evidence regarding physical therapy for the common knee presentations to UC.
MEDIAL COLLATERAL LIGAMENT INJURY
Most medial collateral ligament (MCL) injuries heal well with conservative treatment. The severity of an MCL sprain helps to determine appropriate treatment. Grade I and II injuries are routinely treated with rehabilitation alone. Many isolated grade III sprains can also be treated solely with rehabilitation, with multiple studies demonstrating the success of nonoperative treatment of MCL tears, including complete tears (Grade III injuries).
Rehabilitation programs focus on restoring quadriceps function, improving knee range of motion and controlling knee edema. In general, most athletes can return to full competition, following a well-guided rehabilitation program, 5 to 7 weeks after injury on average.4 However, it is important to distinguish grade III sprain and sprains associated with additional knee injuries, as treatments are often more complex and rehabilitation alone may not be sufficient.5,6
In MCL sprains with concomitant anterior cruciate ligament (ACL) disruption, the MCL injury can often be treated conservatively with rehabilitation while awaiting definitive treatment of the ACL injury. Bony avulsion of the MCL attachment, tibial plateau fracture, or the presence of osteochondral fragments would alter the treatment for an MCL injury and possibly the approach to rehabilitation.2,5,6
LATERAL COLLATERAL LIGAMENT INJURY
Isolated injury of the lateral collateral ligament (LCL) is uncommon, with grade III tears frequently associated with injury to either one of the cruciate ligaments or the posterolateral complex (PLC). Isolated grade I and grade II injuries are amenable to treatment with physical therapy alone. Grade III injuries or patients with suspected concomitant ACL injury, posterior cruciate ligament (PCL) injury, or PLC injury should be evaluated for possible surgical intervention by the orthopedic specialist. These combination injuries are generally not treated with physical therapy alone, and potentially require an element of surgical intervention to ensure stability of the knee.7
PATELLOFEMORAL PAIN
Exercise-based therapy is the first-line therapy for treating patellofemoral pain (PFP).3,8 Based on evidence from the literature, results are optimal when exercises are performed daily for 6 or more weeks.9 Rehabilitation programs have been shown to reduce PFP-related symptoms at short-term (less than 1 year).10,11 Long-term improvements have proven more difficult to sustain. An exercise program consisting of several simple strength and mobility exercises can prevent the development of anterior knee pain.12 This potentially improves the patient’s quality of life without requiring surgical intervention.
QUADRICEPS AND PATELLA TENDON PAIN
Published evidence about specific rehabilitation protocols for quadriceps tendinopathy is limited. However, general concepts of tendinopathy treatment, especially those drawn for the treatment of patellar tendinopathy, provide a useful guide for treatment.13 Several strapping techniques have been shown to be effective in reducing pain and enhancing active movement, therefore improving the patient’s overall movements.2,14
QUADRICEPS MUSCLE TEARS
Surgical treatment is indicated for complete quadriceps and patellar tendon ruptures and for high-grade partial ruptures.15,16 Other than the previously stated, quadriceps muscle and tendon injuries are generally treated conservatively. Following injury, quadriceps muscles quickly develop some degree of wasting due to muscular atrophy from disuse. Therefore, a progressive rehabilitation program should begin as early as possible after injury to prevent muscle wasting from occurring.16 A dedicated rehabilitation program that allows for continued proprioception and muscular conditioning will allow for speedy recovery in patients, especially those who are keen to return to sporting activities.
MENISCAL INJURY
Meniscal injuries may occur as an isolated condition or in combination with other injuries, such as ACL tear.17 Meniscal tears that have issues with symptoms of locking or giving way of the knee should be considered for referral to an orthopedic surgeon, as these patients may benefit from surgical intervention to alleviate those symptoms3,18 Small intrasubstance and vertical tears that cause infrequent symptoms and do not interfere with general knee function can be managed conservatively with rest, activity restriction, and physical therapy.18 In these cases, proprioceptive and quadricep strengthening programs will enable the patient to return to activities and sports within a timely fashion without any significant sequelae to the injury.
In patients presenting with degenerative tears, rehabilitation is especially appropriate.19 Active rehabilitation has been shown to be as effective as arthroscopy in decreasing pain and improving function in patients with nontraumatic degenerative medial meniscal tears without mechanical symptoms.3,20 Initial treatment for all meniscal injuries is similar, regardless of the cause of the injury with no difference in the treatment approaches for those with acute meniscal injury, degenerative tears, or postoperative rehabilitation after meniscectomy.18
Prolonged knee immobilization in splints and casts should be avoided, as these can lead to muscular atrophy and ultimately delay functional recovery. Progressive weight-bearing and range-of-motion movements are allowed. However, excessive shear forces on the meniscus should be avoided as they can disrupt the healing in all types of injuries.21,22
ILIOTIBIAL BAND SYNDROME
Iliotibial band (ITB) syndrome is a common cause of lateral knee pain in the active and athletic population, especially among runners and cyclists.23 Nonsurgical management is the mainstay of this condition with rest, and activity modification improving pain associated with this condition. Rehabilitation programs for ITB syndrome focus on identifying and correcting strength deficits and discrepancies and mobility defects.23,24 Additionally, foam rolling can be used as a myofascial release tool to break down any soft tissue adhesions within the ITB.23
OSTEOARTHRITIS
Physical therapy and exercise are the foundation of nonsurgical management of osteoarthritis-associated knee pain with no clear lesions or associated abnormalities requiring to be addressed surgically.3,25 Evidence has shown that active management is more effective than passive modalities in decreasing knee pain and improving function. Treatment modalities are focused on exercise-based therapies and targeted weight loss3 Treatment programs that strengthen the quadriceps musculature with either isometric or isotonic-resistive exercise are associated with significant improvement in quadriceps strength, reduction of knee pain, and function.26
There is no evidence that presurgical rehabilitation provides postoperative benefits in patients who have had knee arthroplasty for osteoarthritis.27,28
ANTERIOR CRUCIATE LIGAMENT INJURY
Physical therapy and a nonoperative approach are generally recommended for grade I and grade II anterior cruciate ligament (ACL) injuries without the presence of knee instability. The principles of rehabilitation for patients with partial tears are similar to those used for patients with complete tears. Rehabilitation programs consist of exercises for muscle stretching and strengthening and cardiovascular, proprioceptive, and adaptive training.29 Studies have revealed the ability of partial ACL tears to heal contrary to previous understanding regarding the injury.30
Surgical repair of complete rupture of the ACL is recommended to prevent knee joint instability. In highly active patients engaged in jumping, cutting, and pivoting sports, early anatomic ACL reconstruction is recommended because of the high risk of secondary meniscal and cartilage injuries with delayed surgery. A period of progressive rehabilitation to resolve impairments and improve neuromuscular function may be recommended. For patients who want to return to straight-plane activities, nonoperative treatment with structured, progressive rehabilitation is an acceptable treatment option. However, with persistent functional instability, or when episodes of giving way occur, anatomic ACL reconstruction is indicated.31
Knee extensor strength deficit following ACL reconstruction is a common problem, producing deficits on knee function for sports activities and even during daily activities. Therefore, the recovery of quadriceps muscles strength is one of the most important factors after ACL reconstruction.30 There is evidence to suggest that preoperative physiotherapy rehabilitation is beneficial to patients with ACL injury requiring reconstruction in terms of faster recovery of knee extensor strength and function.30,32 It is also anticipated that possible reinjury could be prevented by having better quadricep strength and function.32
POSTERIOR CRUCIATE LIGAMENT INJURY
In general, nonsurgical treatment has been advocated for patients with isolated grade I or grade II PCL injuries, or those who have grade III injuries with mild symptoms, or who only participate in low-demand activities.33 Surgical treatment is therefore recommended for symptomatic complete PCL injuries or combination injuries to restore joint stability and improve function.34
Rehabilitation may begin when swelling has diminished and pain is well controlled; for many patients that means immediately after presentation. The goal of early rehabilitation is to prevent joint stiffness and encourage recruitment of the quadriceps, which the patient may have difficulty activating due to pain or joint effusion. Full strength and function of the quadriceps are needed for full recovery—thus, the importance of addressing this muscle group early during treatment.33 Dynamic PCL braces can help to keep the tibia in a reduced position during the recovery period by avoiding posterior tibial sag, and are indicated both for nonoperative treatment and postoperative rehabilitation of PCL tears.34
CONCLUSION
There are many causes for knee pain that present to urgent care. Appreciation of the cause of the pain and understanding of the potential nonoperative rehabilitation therapies that are available will help patients’ consultations. The ability for the UC physician to provide basic rehabilitation programs, understand the potential benefits of physical therapy in each of the common causes for knee pain, and when to refer patients for these therapies will enhance patient care and improve patient satisfaction.
REFERENCES
- Ibeachu C, Selfe J, Sutton C, Det P. Knee problems are common in young adults and associated with physical activity and not obesity: the findings of a cross-sectional survey in a university cohort. BMC Musculoskelet Disord. 201918;20(1):116.
- Clark N. The role of physiotherapy in rehabilitation of soft tissue injuries of the knee. Orthop and Trauma. 2015;29(1):48-56
- Jones B, Covey C, Sineath M. Nonsurgical managements of knee pain in adults. Am Fam Physician. 2015;92(10):875-883.
- Wijdicks CA, Griffith CJ, Johansen S, et al. Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg A. 2010;92:1266-1280.
- Andrews K, Lu A, Mckean L, Ebraheim N. Review: medial collateral ligament injuries. J Orthop. 2017;14(4):550-554.
- Laprade RF, Wijdicks CA. The management of injuries to the medial side of the knee. J Orthop Sport Phys Ther 2012;42(3):221-233.
- Ramos LA, Zogbi T, Ferreira E, et al. Treatment and outcomes of lateral collateral ligament injury associated with anterior and posterior cruciate ligament injury at 2-year follow-up. J Orthop. 2019;16(6):489-492.
- Petersen W, Rembitzki I, Liebau C. Patellofemoral pain in athletes. Open Access J Sports Med. 2017;8:143-154.
- Harvie D, O’Leary T, Kumar S. A systematic review of randomized controlled trials on exercise parameters in the treatment of patellofemoral pain: what works? J Multidiscip Healthc. 2011;4:383–339.
- Witvrouw E, Lysens R, Bellemans J, et al. Open versus closed kinetic chain exercises for patellofemoral pain. a prospective, randomised study. Am J Sports Med. 2000;28(5):687-694.
- Crossley K, Bennell K, Green S, et al. Physical therapy for patellofemoral pain: a randomized, double-blinded, placebo-controlled trial. Am J Sports Med. 2002;30(6):857-865.
- Coppack R, Etherington J, Wills A. The effects of exercise for the prevention of overuse anterior knee pain: a randomised controlled trial. Am J Sports Med. 2011;39(5):940-948.
- Crossley K. Anterior Knee pain. In: Brukner P, Khan K, eds. Brukner and Khan´s Clinical Sport Medicine. 4th ed. McGraw-Hill, Australia 2011;708.
- Kary J. Diagnosis and management of quadriceps strains and contusion. Curr Rev Musculoskelet Med. 2010;3(1-4):26-31.
- Ramseier LE, Werner CM, Heinzelmann M. Quadriceps and patellar tendon rupture. Injury. 2006;37(6):516-519.
- Ilan D, Tejwani N, Keschner M, Leibman M. Quadriceps tendon rupture. J Am Acad Orthopaed Surg. 2003;11(3):192-200.
- Morelli V, Braxton TM. Medical, plica, patellar and patellofemoral injuries of the knee. Prim Care Clin Off Pract. 2013;40:357.
- Khalifa A, Abd-Elhares R, Abo-Zeid A, Abd-Elaal A. Rehabilitation options for patients with an isolated meniscal tear, a narrative review. Sports Orthopaed Traumatol. 2020;36(4):364-369.
- Stensrud S, Roos E, Risberg M. A 12-week exercise therapy program in middle-aged patients with degenerative meniscus tears: a case series with 1-year follow-up. Orthop Sports Phys Ther. 2012;42(11):919-931.
- Mordecai S, Al-Hadithy N, Ware H, Grupte C. Treatment of meniscal tears: an evidence based approach. World J Orthop. 2014;(3):233-241.
- Nash C, Mickan S, Del Mar C, Glasziou P. Resting injured limbs delays recovery: a systematic review. Fam Pract. 2004;53(9):706-712.
- Sommerfeldt M, Bouliane M, Otto D, et al. The use of early immobilisation in the management of acute soft-tissue injuries of the knee: results of a survey of emergency physicians, sports medicine physicians and orthopaedic surgeons. Can J Surg. 2015;58(1):48-53.
- Strauss E, Kim S, Calcei J, Park D. Iliotibial band syndrome: evaluation and management. J Am Acad Orthop Surg. 2011;19(12):728-736.
- Khalifa A, Abd-Elhares R, Abo-Zeid A, Abd-Elaal A. A review of treatments for iliotibial band syndrome in the athletic population. J Sports Med. 2013;367169.
- Kon E, Filardo G, Drobnic M, et al. Non-surgical management of early knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):436-449.
- Huang M, Lin Y, Yang R et. al. A comparison of various therapeutic exercises on the functional status of patients with knee osteoarthritis. Sem Arth Rheumatism. 2003;32(6):398-406.
- Mat Eil MS, Sharifudin MA, Shokri AA, Rahman SA. Preoperative physiotherapy and short-term functional outcomes of primary total knee arthroplasty. Singapore Med J. 2016;SMJ-57-138.pdf.
- Cabilan CJ, Hines S, Munday J. The effectiveness of prehabilitation or preoperative exercise for surgical patients: a systematic review. BI Database System Rev Implement Rep. 2015;13(1):146-187.
- Temponi EF, Honório de Carvalho Júnior L, Sonnery-Cottet B, Chambat P. Partial tearing of the anterior cruciate ligament: diagnosis and treatment. Rev Bras Ortop. 2015;50(1):9-15 .
- Kim DY, Hwang JH, Park WH. Effects of 4 weeks preoperative exercise on knee extensor strength after anterior cruciate ligament reconstruction. J Phys Ther Sci. 2015;27:2693-2696.
- Diermeier T, Rothrauff B, Engebretsen L, et al. Treatment after anterior cruciate ligament injury: Panther Symposium ACL Treatment Consensus Group. Orthop J Sports Med. 2020;8(6):2325967120931097.
- Alshewaier S, Yeowell G, Fatoye F. The effectiveness of pre-operative exercise physiotherapy rehabilitation on the outcomes of treatment following anterior cruciate ligament injury: a systematic review. Clin Rehabil. 2017;31(1):34-44.
- Wang D, Graziano J, Williams R, Jones K. Nonoperative treatment of PCL injuries: goals of rehabilitation and the natural history of conservative care. Curr Rev Musculoskelet Med. 2018;11(2):290-297.
- Pache C, Aman Z, Kennedy M, et al. Posterior cruciate ligament: current concepts review. Arch Bone Jt Surg. 2018;6(1):8-18.
Author affiliations: Eva Delgado Martinez MBChB, GP, FRCSIUCM, MScCN. Ivan Koay MBChB, FRNZCUC, MD: Urgent Care Physician; RNZCUC Examiner; Education Faculty for the RCSI Fellowship of Urgent Care Medicine; Head of Faculty na hÉireann Royal New Zealand College of Urgent Care. The authors have no relevant financial relationships with any commercial interests.

