Urgent message: Recognizing the need for workup and referral in patients, even if their symptoms are relatively common, is crucial for optimal outcomes
Introduction
Abdominal symptoms can be attributed to a wide array of causes. When etiology is not immediately apparent, searching for signs and symptoms the patient may not have reported—or even be aware of—may be the first steps toward timely diagnosis and treatment. In this case, the abdominal symptoms were ultimately due to an extremely rare condition that required surgical treatment.
Case Presentation
A 62-year-old male presented to an urgent care facility with complaint of abdominal cramping, nausea, and vomiting intermittently for years, with gradual worsening over the past 2 to 3 months. Approximately a half hour to an hour after consuming liquids or solids, the patient would become nauseated and have nonbloody, nonbilious emesis with occasional bloody streaks. Accompanying symptoms include weight loss (approximately 50 pounds over 3-4 months), heartburn, and intermittent dysphagia to solids. The patient is a nonsmoker and nonalcoholic. Past medical history includes nonischemic cardiomyopathy/congestive heart failure (LVEF 15%-20% with grade II diastolic dysfunction), hypertension, diabetes, hyperlipidemia, GERD, and depression. He denied abdominal surgeries and family history of malignancy. He has never had a colonoscopy. Of note, he was seen 2 weeks prior with similar symptoms, had a negative laboratory work-up, and was sent home with promethazine PO/suppository prescriptions with strict ER precautions.
Physical Examination
On physical examination, vitals were stable. Patient was diaphoretic, his oropharynx was dry, and he exhibited skin tenting. Abdominal exam was remarkable for normoactive bowel sounds and diffuse abdominal tenderness without rebound, guarding, or peritoneal signs. The remainder of exam was unremarkable.
Differential Diagnosis
The differential diagnoses of intractable vomiting include, but are not limited to, small bowel obstruction, with most common causes being adhesions or hernia obstruction; diabetic gastroparesis; nonulcer dyspepsia; cyclic vomiting syndrome; hiatal hernia; infectious etiology; or psychogenic/somatization. Additionally, pseudo-obstruction should be considered when there is a metabolic or electrolyte disturbance. In cases where weight loss or loose stool is present, malignancy and inflammatory bowel disease should also be included in the differential diagnosis.
Urgent Care Work-up
Patient was started on intravenous fluids due to obvious dehydration, as well as antiemetics due to his complaint of nausea. Complete metabolic panel and complete blood count were ordered, with results pertinent for leukocytosis (30 x 109 per L) with left shift (absolute neutrophil count 26,000) and mildly elevated Cr (1.4). Abdominal x-ray was obtained.
Management and Outcome
Patient was sent to the emergency department, where a CT scan showed dilated bowel loops, a dilated gastric lumen, and pneumobilia suggestive of a type of gallstone ileus called Bouveret syndrome (Figure 1).
Figure 1. Abdominal x-ray upright shows paucity of gas in small bowel obstruction and pneumobilia (upper left) along with retention of contents secondary to gastric outlet obstruction (right).
Surgery was consulted for gallstone ileus with distal jejunal obstruction (Figure 2, Figure 3). Patient was reexamined by the surgery team, who noted abdominal distension and guarding. A nasogastric tube was placed, and patient was taken to the operating room with a preoperative diagnosis of gallstone ileus, gastric outlet obstruction, jejunal partial obstruction, and cholecystoduodenal fistula.
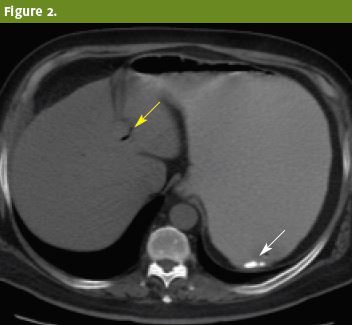
Figure 2. Upright view and computed tomography of the abdomen after administration of positive oral contrast show a dilated gastric lumen and retention of contents secondary to gastric outlet obstruction (solid arrow). Paucity of gas in the small bowel and pneumobilia (hollow arrows) are common findings in Bouveret syndrome.
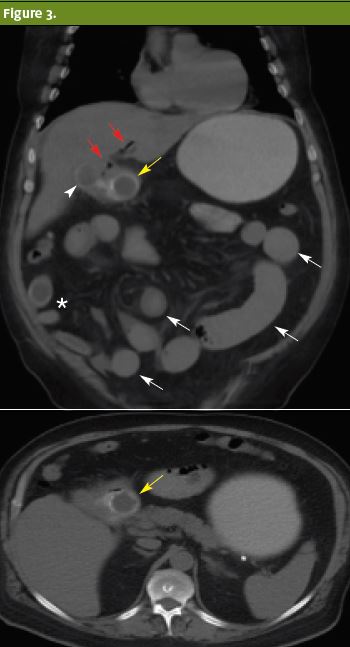
Figure 3. Isotropic coronal (a) and axial (b) noncontrast CT of the abdomen. Multiple hypodense calculi with egg-shell calcifications are visualized in the gallbladder (arrowhead), duodenum (white hollow arrows) and small bowel (asterisk). A duodenal biliary calculus (hollow arrow), pneumobilia (black arrows) and dilated bowel loops (white solid arrows) are consistent with the Rigler’s triad.
Patient underwent exploratory laparotomy, lysis of adhesions, drainage of intra-abdominal abscess, cholecystectomy, and primary repair of 2.5 cm duodenal fistula. He was found to have acute-on-chronic cholecystitis. Two flat JP drains were placed in the right upper quadrant, in the area of the gallbladder fossa, as well as along the edge of the duodenal repair. Patient was taken to the surgical intensive care unit postoperatively, started on ciprofloxacin and metronidazole and on octreotide to minimize any volume loaded through the duodenum, with nasogastric suction for 5 days. He was transferred to the general floor on post-op day 4, NGT and JP drain removed on post-op day 5, and discharged on post-op day 6.
Discussion
Of all mechanical bowel obstruction cases, gallstone ileus is one of the rarest forms. It is caused by a gallstone entering the bowel and causing an obstruction. Gallstone ileus is a complication of gallstones in only 0.5% of patients with gallstone disease1; it occurs in <0.1% of all mechanical obstruction cases in the United States. 2 It is, however, a more common cause of nonstrangulating mechanical small bowel obstruction, accounting for 1%-4% in all patients and up to 25% in the elderly.1 This case featured a rare but insidious cause of gallstone ileus called Bouveret syndrome, which has been identified in a little over 300 cases in literature since its first description in 1654.2,3 Bouveret syndrome is caused by the passage of a large gallstone through a biliodigestive fistula and into the duodenum or pylorus, resulting in gastric outlet obstruction.4
Gallstone ileus and Bouveret syndrome are more common in women than in men (3.5 females to 1 male3), with a long history of cholelithiasis, repeated episodes of acute cholecystitis, stones >2-8cm, and age >60 years.8 Even though gallstones most commonly impact at the terminal ileum and ileocecal valve due to their narrow lumen and potentially less active peristalsis,7 they can cause impaction in any part of the bowel,2 such as the duodenum in Bouveret syndrome.
The presentation of Gallstone ileus and Bouveret syndrome is typically nonspecific, and often with waxing and waning symptoms of nausea, vomiting, abdominal distension, and pain.10 Usually, the symptoms begin 5-7 days prior to medical consultation, and it has been reported that 43%-48% are preceded by a history of recent biliary colic bouts, jaundice, or acute cholecystitis.11 Importantly, the intensity of the pain often does not correlate with the underlying anatomic alteration.11 Laboratory studies are also nonspecific, as only one-third of patients present with jaundice and/or alteration of hepatic enzymes.12
The abdominal radiograph is the mainstay of imaging in small-bowel obstruction. The most frequent findings of Rigler’s triad are as follows: 14
- pneumobilia
- bowel obstruction
- aberrant gallstone
An aberrant gallstone is present in only 40%-50% of cases.14 Ultrasound can be used, but difficulties of locating stones and distortion by bowel gas makes ultrasound suboptimal.10 Unfortunately, abdominal plain radiography is usually of low diagnostic value in those with Bouveret syndrome because it is diagnostic in only 21% of these cases.13 CT is the imaging modality of choice2 in Bouveret syndrome, with an overall sensitivity, specificity, and diagnostic accuracy of 93%, 100%, and 99% respectively.14 Therefore, if there is a clinical suspicion for the diagnosis but negative x-ray findings, a CT scan should be performed.
The gallstones that result in obstruction are usually >2.5 cm2, as those smaller than ≤2.5 cm typically pass through spontaneously and are managed conservatively.10 The consensus is that a general surgeon should be consulted for each case to assess whether conservative or surgical management should be pursued.
Given the advanced age and extensive comorbidities with which the typical patient usually presents, many have adopted the stance that endoscopic or percutaneous approaches such as laser or extracorporeal shockwave lithotripsy should always be attempted prior to surgery.15 However, endoscopic strategies usually fail, and approximately 91% of patients require surgical treatment.15,16 Because of the limited number of reported cases, the optimal surgical method of treatment has been the subject of ongoing debate.2
Despite advances in diagnosis and management, mortality remains high, ranging from 12% to 27%, partially because of nonspecific symptoms, unremarkable biochemical investigations,1 high misdiagnosis rate, and delayed discovery.4 Therefore, gallstone ileus must not be forgotten as a potential diagnosis in such cases.
Anisha Turner, MD and Nathan Martin, MD
AUTHOR ID: Anisha Turner, MD, is a third-year resident in the Emergency Medicine/Family Medicine program at Louisiana State University Medical Center – Shreveport, LA. Nathan Martin, MD practices Family Medicine and Emergency Medicine at University Health in Shreveport, LA.
Citation: Turner A, Martin N. A rar but insidious cause of abdominal pain. J Urgent Care Medicine. February 2017. Available at: https://www.jucm.com/rare-insidious-cause-abdominal-pain/.
References
- Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg. 1994; 60(6):441-446.
- Halabi WJ, Kang CY, Ketana N, et al. Surgery for gallstone ileus: a nationwide comparison of trends and outcomes. Ann Surg. 2014;259(2):329-335.
- Mavroeidis VK, Matthioudakis DI, Economou NK, et al. Bouveret syndrome—the rarest variant of gallstone ileus: a case report and literature review. Case Rep Surg. 2013;2013:839370.
- Lobo DN, Jobling JC, Balfour TW. Gallstone ileus: diagnostic pitfalls and therapeutic successes. J Clin Gastroenterol. 2000;30(1):72–76.
- Iñíguez A, Butte HM, Zúñiga JM, et al. Síndrome de Bouveret: Resolución endóscopica y quirúrgica de cuatro casos clínicos. Revista Médica de Chile. 2008;136:163–168.
- Sánchez Sanchez MR, Caamaño FB, Villarreal CG, et al. Síndrome de Bouveret. A propósito de un caso. Revista Clínica Española. 2003;203:399–400.
- Gupta M, Goyal S, Singal R, et al. Gallstone ileus and jejunal perforation along with gangrenous bowel in a young patient: a case report. N Am J Med Sci. 2010;2(9):442–443.
- Iancu C, Bodea R, Al Hajjar N, et al. Bouveret syndrome associated with acute gangrenous cholecystitis. J Gastrointestinal and Liver Diseases. 2008;17(1):87–90.
- Masannat YA, Caplin S, Brown T. A rare complication of a common disease: Bouveret syndrome, a case report. World J Gastroenterol. 2006;12(16):2620–2621.
- Dai XZ, Li GQ, Zhang F, et al. Gallstone ileus: case report and literature review. World J Gastroenterol. 2013;19(33):5586-5589.
- Gonzalez RG, Fuertes MDA, Diez SR, et al. A rare case of gastrointestinal obstruction: Bouveret syndrome. J Gastrointest Dig Syst. 2015;5(2).
- Trubek S, Bhama JK, Lamki N. Radiological findings in Bouveret’s syndrome. Emerg Radiol. 2001;8(6):335-337.
- Yu CY, Lin CC, Shyu RY, et al. Value of CT in the diagnosis and management of gallstone ileus. World J Gastroenterol. 2005;11(14):2142–2147.
- Wittenburg H, Mossner J, Caca K. Endoscopic treatment of duodenal obstruction due to a gallstone (“Bouveret’s syndrome”). Ann Hepatol. 2005;4(2):132-134
- Nickel F, Müller-Eschner M, Chu J, et al. Bouveret’s syndrome: presentation of two cases with review of the literature and development of a surgical treatment strategy. BMC Surgery. 2013;13:33.
- Nderitu P, Wiik A, Siddiqui M, et al. Gallstone ileus presenting with cholelith emesis and an incidental benign ovarian fibroma: a case report. J Current Surg. 2015;5(1):137-139.
- Doko M, Zovak M, Kopljar M, et al. Comparison of surgical treatments of gallstone ileus: preliminary report. World J Surg. 2003;27(4):400-404.
- Brennan GB, Rosenberg RD, Arora S. Bouveret syndrome. Radiographics. 2004;24(4):1171-1175.
Shalowitz JI. Gallstone emesis. Am J Gastroenterol. 1989;8

