Published on
Urgent message: Evaluation and treatment of injuries of the cheek, ear, nose, lips and tongue are explored to help urgent care clinicians more confidently manage these presentations.
TOYIN FAPOHUNDA-ADEKOLA MD, MBA
In Part 1 of this series, we covered the evaluation and management of scalp, brow, and eyelid lacerations. In Part 2, we will explore injuries of the cheek, ear, nose, lips and tongue. As previously discussed, careful evaluation of neurovascular function and appreciation of techniques that contribute to adequate cosmesis is necessary for ensuring the best results. Basic wound repair skills and application of standard anatomic rule-sets is all that’s required for most facial lacerations. The urgent care clinician should be able to manage the vast majority of these presentations with only occasional referral. However, clinical judgment, patient or parental anxiety, and an assessment of risk or liability are always required and should prompt referral to a higher level of care whenever necessary.
In this article, the second of a two-part series, we will examine the approach to lacerations of the cheek, ear, nose, lips, and tongue.
Cheek Laceration
Patients with lacerations of the cheek are quite commonly seen in the urgent care setting and their injuries usually are associated with animal bites and contact sports. Radiographs are recommended to search for foreign bodies such as tooth fragments and to evaluate for associated zygomatic or orbital fractures.1 Careful examination and testing for injury to the facial nerve and its branches also is necessary. The simple act of elevating the eyebrows can be used to test for the temporalis branch of the facial nerve whereas asking the patient to sniff tests the zygomatic branch. Asking the patient to smile and frown tests the buccal and mandibular branches of the facial nerve and shrugging tests the functioning of the cervical branch.
Wound closure preparation and technique. Anesthesia for small cheek lacerations can be done through direct infusion whereas regional blocks may be necessary for larger wounds. Infra-orbital blocks provide coverage of the superior and medial cheek and are preferable for through-and-through lacerations of the cheek that require closure layer by layer, from the intra-oral mucosa toward the skin. In such situations, a regional block prevents distortion of the tissue and, in multilayer lacerations, provides the longer-acting anesthesia necessary to allow a physician the time to suture each layer.
Mucosal lacerations of less than 3 to 5 cm do not require closure, as they will heal by themselves.2 For larger wounds, closure of the oral mucosa should be done with monofilament 5-0 absorbable suture, which should be followed by copious irrigation of the external wound to remove debris and bacteria that otherwise would contaminate the wound. The external cheek can then be closed with 6-0 monofilament sutures. Large external lacerations, complex bite wounds, or lacerations running perpendicular to the lines of tension should be considered for referral. Care for bite wounds to the cheek follows the same principle as for cheek lacerations of any etiology in regard to irrigation and prep for closure. Although prospective data are lacking, general consensus suggests that bite wounds to the cheek are appropriately managed with primary closure within 24 hours of injury, provided there are no signs of acute infection. As discussed previously, empiric antibiotics are generally not necessary but should be considered for deep tissue injuries, bites from cats and dogs or potentially rabid vermin, or for patients who are immunocompromised.
After care and follow up. Patients with cheek lacerations should be instructed to cleanse their wounds daily with soap and water. In most cases, prophylactic antibiotics are not necessary, but if required, coverage should be based on the type of bacteria that are most common in each situation (e.g., Pasteurella multocida in dog/cat bites; Staphylococcus aureus in human bites).
Ear Laceration
Ear lacerations usually are a result of blunt trauma to the head. Therefore, the most important initial consideration is assessment of potential for serious brain injury by checking the patient for altered level of consciousness, impaired breathing, or signs of basilar skull fractures Deficits in cranial nerves VI, VII, and VIII in the setting of blunt head trauma are red flags for basilar skull fracture and should be referred urgently. Once these signs have been ruled out, specific evaluation begins with a focus on the location of the laceration, amount of cartilage involved, and depth of injury. Basilar and middle ear trauma should also be assessed via otoscope and considered in patients who exhibit nystagmus, retro-auricular bruising or hematoma (Battle sign), hemotypanum, otorrhea (both clear or bloody) or ataxia.
Contraindications to ear laceration repairs include evidence of basilar skull fractures, infection, total auricular avulsion, extension of a laceration into the auditory canal or hearing loss caused by the injury. In these situations, the patient should be immediately referred to an otolaryngologist, surgeon, or to the emergency department if basilar fractures are suspected.
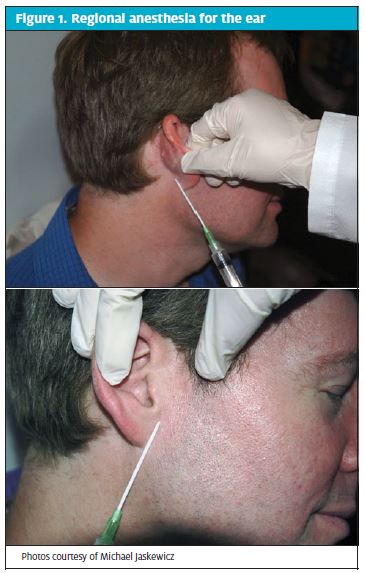
Wound closure preparation and technique. For ear lacerations, the preferred anesthesia is local infiltration of lidocaine without epinephrine because epinephrine can cause vasoconstriction and disruption of the blood supply can damage the cartilage. A regional block is preferable for extensive lacerations.
To administer a regional block, enter at a point just below the ear. Move posteriorly and inject 5 mL of lidocaine (0.7 mL/kg) as the needle is being withdrawn. Without removing the needle, redirect the needle anteriorly (in a vertical V shape) and inject another 5 mL. Next, insert the needle at a point just above the ear and repeat the previous steps to anesthetize an area in an inverted V shape (Figure 1).
Wound closure preparation and technique. Once anesthesia for an ear laceration has been achieved, irrigate the wound with normal saline without unintentionally debriding tissue needed to close the laceration. Suture choice should be dependent on the tissue being closed.
For skin closure, 5-0 or 6-0 non-absorbable sutures should be used in single interrupted fashion. Split earlobes, one of the most common ear lacerations seen in the urgent care setting, require both subcutaneous closure with absorbable suture and skin closure with nonabsorbable single interrupted sutures.
Complex lacerations, which expose or extend through the cartilage, should be carefully repaired with attention paid to properly approximating the cartilage and ensuring that the cartilage is covered by skin to prevent deformities. Because the skin overlying the cartilage is thin, the sutures should incorporate the two layers. Sutures should never be buried in the cartilage. All subcutaneous stitches should be buried in the perichondrium using 5-0 absorbable suture and with special care to gently approximate the cartilage without damaging or tearing this fragile tissue.
Debridement of cartilage is also not recommended unless the laceration involves infection or the edges are severely deformed or jagged. In those situations, debridement should be kept to a minimum to prevent notching and preserve cosmesis.
After care and follow up. Tetanus prophylaxis should be provided as indicated.
Antibiotics are not required for most ear lacerations. The exceptions are for lacerations caused by a human or animal bite, those in which contamination is obvious or suspected, or lacerations in patients who are immunodeficient or who have poor vascularity. Patients treated for ear lacerations should be counseled on signs of infection and told to gently clean their wounds once a day but with strict water precautions. They should be instructed to return for re-evaluation in 24 to 48 hours and nonabsorbable sutures should be removed in 7 to 10 days.
Prevention and management of auricular hematoma.
Auricular hematomas tend to occur from blunt force trauma and are usually seen in athletes such as wrestlers and football players who present for urgent care with injuries sustained during a match (Figure 2).
With auricular hematomas, pressure caused by accumulation of blood within the space between the cartilage and perichondrium deprives the cartilage of its blood supply, leading to necrosis. If the blood is not properly drained, the consequence is deformity of the cartilage, otherwise known as cauliflower ear.
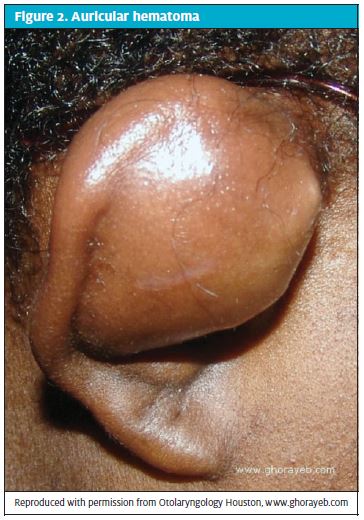
Depending on an urgent care provider’s comfort level, needle aspiration can be used to drain auricular hematomas less than 2 cm that have been present less than 48 hours. However, patients who present with hematomas that occurred more than 7 days previously should be referred to an otolaryngologist for treatment.2
Pressure dressings tend to be the most effective way to prevent auricular hematomas in patients with ear lacerations. To apply a pressure dressing, first provide support for the ear by creating a “bed” from 4×4 sponges cut in the contoured shape of the ear. Then fill the space within the helix with petrolatum gauze and mold it over the antitragus, antihelix, and external canal. Place gauze sponges over the whole ear, followed by a 3- or 4-inch gauze bandage wrapped around the head for compression. This can be further tightened by applying gauze tie anterior to the ear.3
Management of perichondritis and chondritis. Infection and inflammation of the perichondrium (perichondritis) and auricular cartilage (chondritis), respectively, are other complications of ear laceration. These conditions are easily diagnosed based on symptoms including redness, warmth, and fluctuance. Prompt drainage is required for treatment of perichondritis and chondritis to prevent permanent deformity of the cartilage and, subsequently, the ear. In most of the cases, the bacteria responsible is pseudomonas and antibiotic treatment with fluoroquinolones or penicillin is required.
Nose Laceration
The nose is composed of both bony and cartilaginous components and injuries to it are common and often seen as a result of physical assaults and unintentional sports-related traumas. Taking a proper patient history is important in patients with nose lacerations because the mode of injury is a vital detail suggestive of other systems that should be assessed. For example, significant blunt force trauma, as with an assault by a baseball bat, require an extensive ocular, neurologic, and dental examination, along with evaluation for more significant facial bone injuries.
Examination of the patient with a nose laceration should include both internal and external inspection, with concentration on possible obstruction and breathing difficulties. Signs of basilar fracture, which requires immediate neurosurgical consultation, include the emission of clear fluid from the nares, hemotympanum, “raccoon eyes” sign, or “Battle’s sign” (ecchymosis around mastoid). Delayed closure and prompt consultation are required for displaced fractures of the nasal bone associated with laceration (open fracture).
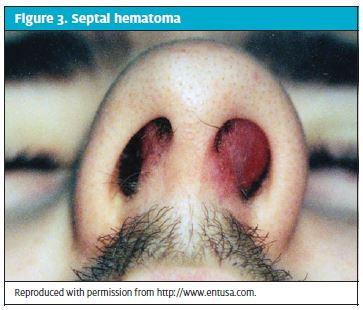
Management of septal hematomas. As with auricular hematomas, septal hematomas can occur in patients with nasal lacerations. Appearing as a dark blue or purple tender mass at the septum, a septal hematoma increases the risk of cartilage damage and subsequent deformity and it may signal the presence of a basilar fracture (Figure 3). The appropriate treatment is drainage and examination of fluid, followed by pressure packing with a nasal tampon. Keep in mind that because all tampon insertions increase the risk of toxic shock syndrome, empirical antibiotics (preferably amoxicillin/clavulanic acid) should be given. For small hematomas, drainage and close monitoring may be sufficient.
Wound closure preparation and technique. When anesthetizing the nose, direct infiltration with lidocaine without epinephrine is usually sufficient. If a nasal block is even a consideration, the appropriateness of the case for urgent care should be re-evaluated.
After proper anesthesia is achieved, irrigation should be done with normal saline with or without povidoneiodine. Debridement should be kept to the utmost minimum, as nasal tissue is not elastic and heals poorly from any deformation. Skin tags or flaps can be tacked down with interrupted sutures or steri-strips.2 Non-absorbable 6-0 sutures should be used, taken in small shallow bites, as nasal tissue tends to invert and cannot hold tension. Sutures with high tension should be removed and replaced with deep absorbable 5-0/6-0 sutures first before superficial ones are placed. Nasal lacerations usually involve multiple layers (i.e., skin, mucosa, and cartilage). Closing the skin and mucosa with the closest approximation as possible is important to prevent notching and deformity. Suturing cartilage is unnecessary because its coverage by skin and mucosa ensures healing.2 However, if the cartilage cannot be completely covered, the risk of chondritis and deformity is increased and referral to an otolaryngologist or to a plastic surgeon is recommended.
After care and follow up. Patients with nasal lacerations may be self-conscious about the appearance of their wound but dressings generally are not required. For superficial wounds, empirical antibiotics are usually unnecessary because the nose’s high vascularity protects against infections.
Lip Laceration
Etiologies of lip laceration are many, ranging from assault to falls. Because the lip is rich in vascularity, lacerations tend to bleed profusely and they are a very common presentation in the urgent care setting.
Indications for repair of lip laceration include a wound larger than 0.25 cm and/or one that gapes at rest.4 Macerated wounds, associated facial bone fracture, suspected injury to the orbicularis muscle, large areas of missing lip tissue or wounds left unrepaired for more than 12 hours all necessitate management by a plastic surgeon.4
In patients whose lacerations can be repaired, perform a complete exploration for foreign bodies and a dental check for missing or broken teeth. If there are any teeth missing, a facial x-ray should be considered to rule out embedment.
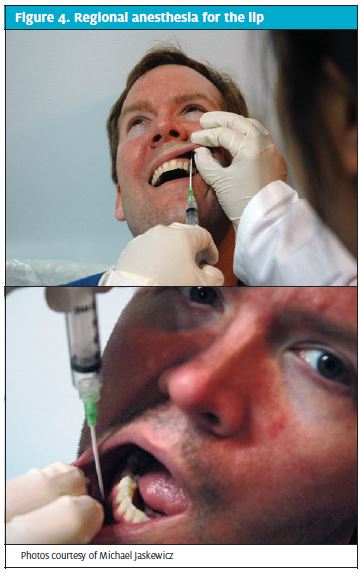
Wound closure, preparation and technique. Because direct infiltration of anesthetics into the lip can distort the tissue, regional blocks should be used for anesthesia in lip laceration (Figure 4). An infraorbital block (deposition of anesthesia into the anterior margin of the maxillary canine) can be used for lacerations that involve the upper lip. For injury of the lower lip, a mental block (with lower lip retraction, inject inferior to the second bicuspid in the gingival-buccal margin) can be used. The anesthetic of choice is plain lidocaine but for external lacerations with profuse bleeding, epinephrine can be added to gain hemodynamic control. Once complete anesthesia is achieved, irrigation with saline should follow.
If there are skin flaps present, care should be taken not to mistakenly debride tissue. For the repair, nonabsorbable sutures (preferably 4-0 or 5-0) generally can be used. However, for a lacerations that extend to deep muscle, closure of each layer individually is required and buried absorbable sutures should be used for the muscle and inner mucosa (Figure 5).
Special considerations: Frenulum, Vermillion borders, philtrum. The vermilion border is an important anatomical structure and a distortion in it of as little as 1 mm can create a “step off” that is visible to the naked eye.2 Because of this, the vermillion border should be approximated
first and repaired before any other part of the lip is closed. Suturing of the vermillion border should be done with 6-0 non-absorbable materials and, if the laceration extends into the oral mucosa, 5-0 absorbable sutures can be used. Not all lip and oral lacerations need repair; lacerations and avulsions of the frenulum, for example, tend to heal on their own and need no further management.
The philtrum is another location of anatomic importance. This cosmetically sensitive area represents the vertical cleft between the nose and upper lip. Patients who have lacerations in this area should be referred to a plastic surgeon because any distortion in the tissue can cause significant cosmetic disproportion.
After care and follow up. Oral antibiotics (usually penicillins) are required following closure of a lip laceration that extends into the deep mucosa. Patients who have superficial lacerations should be counseled to follow a regular cleansing protocol and advised on warning signs of infection. A follow-up visit should be schedule in 24 to 48 hours.
Tongue Laceration
The tongue is important to both digestion and speech. Proper repair of a tongue laceration is imperative to preserve speech, ensure the function of swallowing, and prevent infection. Many tongue lacerations do not require repair but it is important to recognize those that do. Indications for repair of tongue laceration include large (>1 cm) gaping wounds with edges that don’t approximate when at rest, involvement of muscle, uncontrolled profuse bleeding, or “through and through” injuries.
Wound closure preparation and repair technique. Patients with tongue lacerations should be examined for debris and tooth fragments, especially if they have broken or missing teeth. Following examination, irrigation with normal saline should be done, with debridement of any noticeable necrotic tissue.
Lidocaine is the anesthetic of choice for tongue repair. Topical application of a gauze soaked with lidocaine 4% is appropriate, as is local infiltration with lidocaine 1% with or without epinephrine. For larger lacerations, a lingual block may be necessary.
Suturing of the tongue or any part of the oral cavity can be quite difficult, requiring a patient’s mouth to be held in an unnatural and, therefore, uncomfortable position. To facilitate optimal positioning and ease for both patient and physician, mouth gags and bite blocks can be used to keep the mouth open. To keep the tongue protruding, gauze sponges can be used. With the tongue fully anesthetized, a single suture also can be passed through the tongue and held in extension.

Repair of tongue lacerations should be performed with absorbable sutures. Chromic gut 4-0 or 5-0 is preferable because it is less sharp than other materials, such as nylon. To prevent the knots from being untied by the natural movements of the tongue, sutures should be placed in square knot “bites” that are wide and deep enough to close all layers with a single stitch.
Antibiotics are indicated for patients with heavily contaminated tongue lacerations for which debridement is suboptimal, when debridement is delayed for more than 24 hours, for wounds associated with jaw fractures and that require open reduction, in immunocompromised patients, and for wounds caused by human or animal bites.5 Clindamycin or penicillin is an optimal antibiotic because it covers both the anaerobic and Gram-positive bacteria of the oral cavity.
After care and follow up. On discharge, patients with tongue lacerations should be instructed to gently swish and spit with mouthwash and avoid eating or drinking until anesthesia has worn off and their sensation has returned. They should be counseled to eat a soft diet to ensure healing and to suck on ice chips or apply anything cold to help prevent swelling.
Conclusion
Facial lacerations can create a significant amount of anxiety for patients and clinicians alike. Good cosmesis and healing depend on an understanding of facial anatomy and the principles of repair. The evaluation and treatment of these injuries in the urgent care setting is appropriate in most circumstances, and the techniques used for repair are not new to the urgent care clinician. This two-part series explored the indications and procedures for urgent care management as well as reasons for referral to specialty care. With this clinical review, the clinician should be able to more confidently evaluate facial injuries and better determine the optimal clinical management and disposition.
References
- Flores MT, Andersson L, Andreasen JO, et al. Guidelines for the management of traumatic dental injuries. I. Fractures and luxations of permanent teeth. Dental Traumatology. 2007;23(2):66-71.
- Trott AT. (2012). Wounds and lacerations: emergency care and closure. Elsevier Health Sciences.
- Taub PJ., Patel PK, Buchman SR, Cohen MN. Ferraro’s Fundamentals of Maxillofacial Surgery. Springer.cf
- Colyar MR, Ehrhardt CR. Ambulatory care procedures for the nurse practitioner. FA Davis. 2003.
- Armstrong BD. Lacerations of the mouth. Emerg Med Clin North Am. 2000;18:471–480.
