Urgent Message: Patients discharged from an urgent care clinic with tachycardia were found to have significantly higher odds of return visits to the urgent care and emergency department as well as higher odds of being admitted to the hospital within 7 days compared to non-tachycardic patients.
Vitoria Regina Nunes Maia, MD; Ryan Loh, PhD; Michael Weinstock, MD; Lindsey E. Fish, MD
Citation: Maia VRN, Loh R, Weinstock M, Fish L. Return Visits and Hospitalization Rates of Adult Patients Discharged with Tachycardia After an Urgent Care Visit: A Retrospective Cohort Study. J Urgent Care Med. 2024; 18 (9):37-41
Abstract
Introduction: Adult patients discharged from the emergency department (ED) with tachycardia have been shown to be at short-term risk of increased morbidity and mortality. We aimed to identify if a similar association exists in adult patients discharged with tachycardia from an urgent care (UC) clinic.
Methods: We conducted a retrospective cohort study of all adult visits where the patient was discharged from a single site urgent care clinic from 2016-2022. In the study, 106,676 adult patient visits were included. Patients were divided into 2 groups: tachycardic (last recorded heart rate ≥100 beats per minute [BPM]) and non-tachycardic (last recorded heart rate of <100 BPM). Primary outcomes were return visit to the urgent care or ED within 7 days of discharge and hospital admission within 7 days discharge.
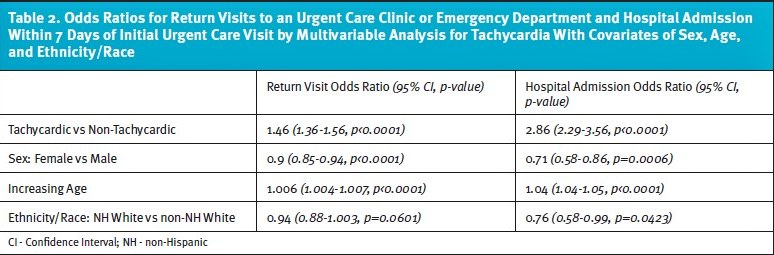
Results: Statistically significant differences were noted between the tachycardic and non-tachycardic groups for return visits to urgent care or ED (11.67% vs 8.5%, p<0.0001) and hospital admissions (0.91% vs 0.38%, p<0.0001). This corresponded to 1.46 greater odds that tachycardic patients would have a return visit to either urgent care or the ED within 7 days of discharge compared to non-tachycardic patients. The odds ratio (OR) for hospital admission within 7 days was 2.86 when comparing tachycardic to non-tachycardic patients.
Discussion: Patients discharged from the urgent care clinic with a heart rate >100 BPM had significantly higher odds of returning to either the UC or ED and being admitted to the hospital within 7 days of discharge from the index urgent care visit.
Introduction
Heart rate (HR) is used in the risk stratification criteria of many acute-care guidelines utilized in urgent care (UC) clinic settings based on evidence extrapolated from research conducted among emergency department (ED) patients. Examples of how HR is used to risk stratify patients for various life-threatening conditions include the Systemic Inflammatory Response Syndrome score/sepsis criteria, Pneumonia Severity Index score, and Pulmonary Embolism Rule-Out Criteria score.1-7 Each of these criteria utilize an upper limit HR, which, if a patient exceeds, results in a “point” going towards a higher overall risk associated with the condition of concern.
Tachycardia in patients age 18 and older is defined as a heart rate greater than 100 beats per minute (BPM). There are many forms of tachycardia, and tachycardia can result from a heterogenous mix of underlying etiologies including arrhythmias, myocarditis, acute coronary syndrome, pulmonary emboli, hypoxemia, hypoglycemia, dehydration/hypovolemia, sepsis, anemia, medication and stimulant use, alcohol withdrawal, anxiety, pain, and fever.8
Being discharged from the ED with abnormal vital signs has been associated with increased short-term morbidity and mortality, with 1 study correlating it with higher rates of unanticipated death at 7 days.9 Vital signs, including HR, are highly dynamic and vary continuously throughout each day and phase of life, with the threshold for being “abnormal” ill-defined. However, it is of great clinical utility to have an easily assessable biomarker if it can be used to identify patients at risk for serious adverse outcomes. 10-11 Additional ED-based studies have demonstrated that tachycardia was the most common abnormal vital sign among adults who experienced an unanticipated death within 7 days after an ED visit.12-13
Given the concerning association between ED discharge of tachycardic patients and increased short-term morbidity and mortality in adult patients, we aimed to identify if a similar correlation existed in adult patients discharged with tachycardia from a urgent care clinic. Such an association would be especially valuable in the urgent care setting as vital signs are among the few objective pieces of clinical data available to UC clinicians. Additionally, the UC setting represents an increasingly common site of care for patients with undifferentiated symptoms; clinicians in this setting are often forced to evaluate patients with great rapidity. Therefore, any quickly available objective data point that might suggest that a patient is at increased risk of a short-term adverse outcome would be valuable for the assurance of UC patient safety.
Methods
Project methodology was reviewed by the Denver Health and Hospital Authority Quality Improvement Committee, authorized by the Colorado Multiple Institutional Review Board at the University of Colorado, Denver, and given a waiver after being determined non-human subject research.
This is a retrospective cohort study utilizing the electronic health record data (EHR) at our single site UC center, the Federico F. Peña Southwest Urgent Care Clinic (PUCC). PUCC is a Federally Qualified Health Center located in a largely Hispanic neighborhood affiliated with Denver Health and Hospital Authority (DHHA). DHHA is an urban safety-net health system, serving one-third of the population of Denver, comprised of a safety-net hospital, 10 federally qualified community health centers, and 19 school-based clinics.
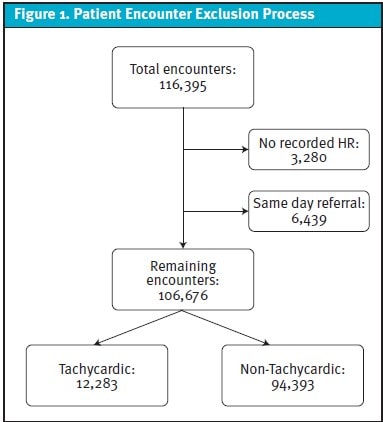
Primary analysis included adult patients (age 18 and older) who presented to PUCC between the dates of April 18, 2016 (date clinic opened), and December 31, 2022. We excluded patient encounters for whom no HR was recorded in the EHR and encounters for patients who were referred immediately to an ED by the urgent care provider. The remaining encounters represented patients who were discharged home, and those were divided into 2 groups: those with a last recorded heart rate of ≥100 bpm (“tachycardic”) and those with a last recorded HR <100 bpm (“non-tachycardic”) (Figure 1). Predetermined primary outcomes for each of these groups included a combined outcome of return visit to either a urgent care clinic or ED within the DHHA system within 7 days and hospital admission at DHHA within 7 days. The predetermined secondary outcome was death within 7 days, which was assess based on Colorado public health records and EHR data collaboration as described by Simpson et. al.14
Statistical analyses were performed using encounter-based data, which meant that multiple visits by the same patient were all treated as discrete, separate encounters. To account for repeated visits, generalized estimating equations were used with logit link function to model each individual patient visit, while accounting for the correlation of outcomes in the same patient. Univariate chi-squared values are reported for each of the demographic variables in the final model. Demographic variables included for analysis were sex, age, and ethnicity/race and were based on the information gathered during the first encounter in the included period.
Results
In total, there were 106,676 included UC encounters during the study period, which occurred among 45,862 unique patients. Demographic characteristics between the tachycardic and non-tachycardic patient encounter groups were not statistically analyzed (Table 1). When holding all other factors constant, there were significant differences between the tachycardic and non-tachycardic groups for the odds of return visits to either a urgent care clinic or ED within 7 days (11.67% vs 8.5%) and hospital admission within 7 days (0.91% vs 0.38%). There were only 11 deaths within 7 days of urgent care discharge among the entire cohort (1 in the tachycardic group [0.01%] and 10 in the non-tachycardic group [0.01%]). Given the extreme rarity of this outcome, statistics were not analyzed on this outcome.
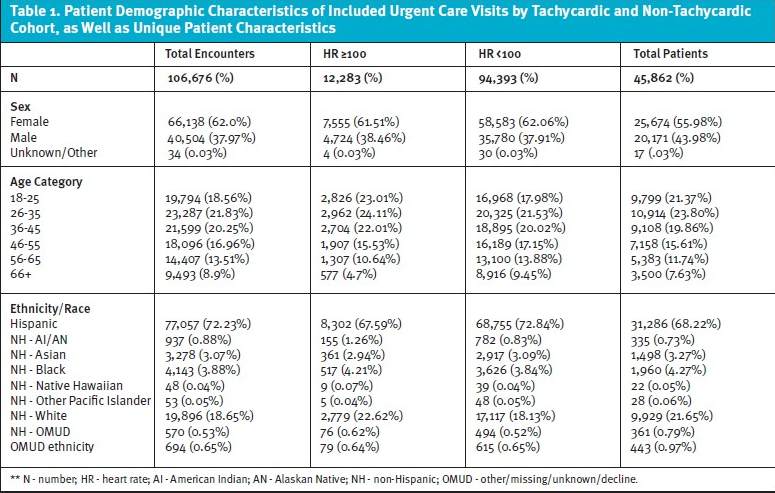
In the multivariable analysis controlling for the effects of sex, age, and ethnicity/race to examine return visits to either an urgent care or ED within 7 days of the initial urgent care visit, the odds that a tachycardic patient would return was 1.46 times higher (OR=1.46 [95% CI, 1.36 – 1.56], p<0.0001) than the odds a non-tachycardic patient would return. In the multivariable analysis controlling for the effects of sex, age, and ethnicity/race, examining hospital admissions within 7 days of the initial urgent care visit, the odds that a tachycardic patient would be admitted were 2.86 times higher (OR=2.86 [95% CI, 2.29 – 3.56], p<0.0001) than non-tachycardic patients. Individual odds ratios for the covariates of sex, age and ethnicity/race were also calculated (Table 2).
Discussion
Among the over 100,000 adult patient encounters reviewed from our urgent care clinic, we found that patients who were discharged from the urgent care with tachycardia had increased rates of return visits to urgent care and ED settings as well as increased rates of hospital admission within the subsequent week. The number of deaths among this cohort of patients was too few to determine if there was a significant difference in risk of death among patients in each group. Further studies, ideally larger and multicenter, are needed to determine if any association exists between tachycardia at discharge from urgent care and mortality given how rare of an occurrence short-term mortality is following a urgent care visit. Our finding of increased odds of return visit and hospital admission is consistent with previous studies showing increased risk of return visits, morbidity, and death in patients discharged from an ED setting with abnormal vital signs.9-13
While not the primary covariates of interest, the demographic covariates included in our analyses did significantly affect the odds of the primary outcomes occurring. Both male sex and increasing patient age were significantly associated with increased odds of both UC or ED revisit and hospital admission. Non-Hispanic White patients had the lowest relative odds of admission within 7 days and a trend toward lower rates of revisit compared with the other ethnicities/races. Increasing age and Hispanic ethnicity have previously been shown in the ED literature to correlate to increased return visits, whereas male sex has a lower rate of return visits in the ED literature.15-17
This study sought to determine if a similar association existed between adverse clinical outcomes and the presence of tachycardia at discharge from the urgent care clinic. The potential clinical implications of these findings are significant. First, this suggests clinical utility for UC providers to be attentive to the HR of patients and, in the cases of tachycardia, repeat the measurement to determine if the HR is remaining persistently elevated. Persistent tachycardia and/or tachycardia upon discharge appears to be a risk factor for increased short-term healthcare utilization, a finding that has also been demonstrated in studies of discharged ED patients.18-20 Increased rates of return visits to urgent care clinics and EDs, as well as hospital admissions, may additionally increase the financial burden to both patients and the healthcare system. Further research is needed to determine how tachycardia at urgent care discharge might best be addressed to optimize patient safety.
Limitations
There are several limitations to the findings of our study. First, our analysis was performed among patients seen at a single urgent care clinic within 1 healthcare system; this may limit the ability to generalize these findings to other UC practices and other geographic locations. For instance, the included study population of the UC clinic during the study period was nearly 73% Hispanic; this may not reflect the demographics of other UC clinics. Additionally, the data does not include UC or ED return visits and admissions that may have occurred outside of our healthcare system. This was a retrospective grouped analysis, and there was no matching between tachycardic and non-tachycardic cohort patients. While we included demographic covariates, there may be other factors including clinical conditions such as fever, comorbid conditions, access to primary care, etc. that may impact the findings. Given the retrospective design, there was no standardization for the number of times vital signs were recorded, and therefore, the true value for patients’ HR at the time of urgent care discharge was extrapolated from the last HR data point entered by the clinical staff. Finally, urgent care or ED visits after discharge were used as a surrogate for adverse outcomes and short-term morbidity, however, this may not always be the case. The reason for urgent care or ED utilization after the index visit was not available, and therefore, it is unclear to what extent these may have been expected revisits (eg, wound check, suture removal, etc.) vs revisits related to morbidity associated their condition or other complications.
Conclusion
Patients discharged from the urgent care clinic with a HR >100 BPM were found to have a significantly higher odds of returning to the urgent care or visiting the ED within 7 days as well as higher odds of being admitted to the hospital within 7 days compared to patients with a HR <100 BPM when discharged from urgent care.
References
- Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992 Jun;101(6):1644-55. doi: 10.1378/chest.101.6.1644. PMID: 1303622.
- Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G; SCCM/ESICM/ACCP/ATS/SIS. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003 Apr;31(4):1250-6. doi: 10.1097/01.CCM.0000050454.01978.3B. PMID: 12682500.
- Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, Coley CM, Marrie TJ, Kapoor WN. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997 Jan 23;336(4):243-50. doi: 10.1056/NEJM199701233360402. PMID: 8995086.
- Shah BA, Ahmed W, Dhobi GN, Shah NN, Khursheed SQ, Haq I. Validity of pneumonia severity index and CURB-65 severity scoring systems in community acquired pneumonia in an Indian setting. Indian J Chest Dis Allied Sci. 2010 Jan-Mar;52(1):9-17. PMID: 20364609.
- Anurag A, Preetam M. Validation of PSI/PORT, CURB-65 and SCAP scoring system in COVID-19 pneumonia for prediction of disease severity and 14-day mortality. Clin Respir J. 2021 May;15(5):467-471. doi: 10.1111/crj.13326. Epub 2021 Jan 23. PMID: 33417280.
- Kline JA, Mitchell AM, Kabrhel C, Richman PB, Courtney DM. Clinical criteria to prevent unnecessary diagnostic testing in emergency department patients with suspected pulmonary embolism. J Thromb Haemost. 2004 Aug;2(8):1247-55. doi: 10.1111/j.1538-7836.2004.00790.x. PMID: 15304025.
- Kline JA, Courtney DM, Kabrhel C, Moore CL, Smithline HA, Plewa MC, Richman PB, O’Neil BJ, Nordenholz K. Prospective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008 May;6(5):772-80. doi: 10.1111/j.1538-7836.2008.02944.x. Epub 2008 Mar 3. PMID: 18318689.
- Mayuga KA, Fedorowski A, Ricci F, et.al. Sinus Tachycardia: a Multidisciplinary Expert Focused Review. Circ Arrhythm Electrophysiol. 2022 Sep;15(9):e007960. doi: 10.1161/CIRCEP.121.007960. Epub 2022 Sep 8. PMID: 36074973; PMCID: PMC9523592.
- Sklar, David P., et al. Unanticipated death after discharge home from the emergency department. Annals of Emergency Med. 49.6 (2007): 735-745.
- Candel, Bart GJ, et al. The Association Between Vital Signs And Clinical Outcomes In Emergency Department Patients Of Different Age Categories. Emergency Medicine Journal. 39.12 (2022): 903-911.
- Ljunggren, Malin, et al. The association between vital signs and mortality in a retrospective cohort study of an unselected emergency department population.Scand J Trauma Resusc Emerg Med. 24.1 (2016): 1-11.
- Gabayan, Gelareh Z., et al. Qualitative factors in patients who die shortly after emergency department discharge. Academic Emergency Med. 20.8 (2013): 778-785.
- Chang CY, Abujaber S, Pany MJ, Obermeyer Z. Are vital sign abnormalities associated with poor outcomes after emergency department discharge? Acute Med. 2019;18(2):88-95
- Simpson, Scott A., et al. A Mortality Surveillance Collaboration Between a Health System and Public Health Department. American Journal of Public Health. (2023): e1-e4.
- Ling DA, Sung CW, Fang CC, Ko CH, Chou EH, Herrala J, Lu TC, Huang CH, Tsai CL. High-risk Return Visits to United States Emergency Departments, 2010-2018. West J Emerg Med. 2022 Oct 18;23(6):832-840. doi: 10.5811/westjem.2022.7.57028. PMID: 36409935; PMCID: PMC9683777.
- Hutchinson CL, Curtis K, McCloughen A, Qian S, Yu P, Fethney J. Identifying return visits to the Emergency Department: A multi-centre study. Australas Emerg Care. 2021 Mar;24(1):34-42. doi: 10.1016/j.auec.2020.05.007. Epub 2020 Jun 24. PMID: 32593525.
- Hu KW, Lu YH, Lin HJ, Guo HR, Foo NP. Unscheduled return visits with and without admission post emergency department discharge. J Emerg Med. 2012 Dec;43(6):1110-8. doi: 10.1016/j.jemermed.2012.01.062. Epub 2012 Jun 5. PMID: 22674038.
- Quinten VM, van Meurs M, Olgers TJ, et al. Repeated vital sign measurements in the emergency department predict patient deterioration within 72 hours: a prospective observational study. Scand J Trauma Resusc Emerg Med. 2018;26(1):57.
- Russell J. The Value of Repeat Value Signs. J Urgent Care Med. 2022;17(2):1-2.
- Melrose G. It’s About Time: Repeat Vitals and Long Waits. J Urgent Care Med. 2023; 17(5):1-2.
Author Affiliations: Vitoria Regina Nunes Maia, MD, Department of Internal Medicine, Hospital Santa Rosa de Lima, Serra Negra, Sao Paulo, Brazil. Ryan Loh, PhD, Behavioral Health Services, Denver Health and Hospital, Denver, Colorado. Michael Weinstock, MD, Department of Emergency Medicine, Adena Health System and Department of Emergency Medicine, The Wexner Medical Center at The Ohio State University, Chillicothe, Ohio. Lindsey E. Fish, MD, Department of General Internal Medicine, Denver Health and Hospital and Division of General Internal Medicine, University of Colorado School of Medicine, Denver, Colorado.


