Published on
Urgent message: “Mock trials” are a valuable tool to help urgent care providers offer better medical care, record more appropriate documentation, and learn about medical proceedings.
Michael Weinstock, MD; Kaetha Frost, DO; Heath Jolliff, DO; Amal Mattu, MD; Seth McIntire, DO; Marc Calvert, JD; Mark Kitrick, JD; and Matt Delaney, MD
Citation: Weinstock M, Frost K, Jolliff H, Mattu A, McIntire S, Calvert M, Kitrick M, Delaney M. See you in court: practice and documentation change from a mock trial. J Urgent Care Med. 2022;16(5):23-27.
ABSTRACT
Background
The risk of medicolegal action following an emergency department visit is a source of misinformation and stress for clinicians.
Objective
To determine if viewers of a mock trial think it will result in a change in practice and/or documentation.
Methods
Participants included the residents and attendings at the host facility and invitees from the Council of Residency Directors (CORD) listserv, social media, and past participants of this yearly conference. During a 90-minute mock trial the defendant was represented by a volunteer third-year emergency medicine resident, practicing attorneys as counsel, and two EM physicians with extensive real-world medicolegal experience as expert witnesses. Following closing statements, the audience participants completed a survey. Those who did not watch all or most of the trial and those who did not answer all the survey questions were excluded.
Results
There were 682 unique views of the conference on Zoom video, of which 404 participants met the inclusion criteria, representing 176 attending physicians of which 137 (80%) were EM; 99 residents of which 79 (80%) were EM; 34 physician assistant (PA) students; 32 medical students; 27 nurse practitioners/students; 20 PAs, four attorneys and 12 “other.” Three hundred eighty-five (95%) thought the physician in the case practiced “standard of care,” but only 212 (52%) thought they practiced “excellence in care.” A significant number of participants 290 (72%) stated they would change or consider changing their practice and 374 (92%) stated they would change or consider changing their documentation after watching the mock trial.
Conclusions
A mock trial appears to be an effective teaching modality to create practice change and documentation change.
INTRODUCTION
Across a wide variety of medical learners, the threat of being sued after an adverse medical event is a source of significant stress.1-5 While there are various publications, lectures, courses, and podcasts focused on medicolegal risk, these educational products often have a limited scope featuring a medical expert discussing various high-risk patient presentations. Additionally, medicolegal training in residency is often lacking.6 Brown, et al reported that only 7% of malpractice cases filed against emergency clinicians resulted in a trial7; given the rarity of courtroom cases, learning from real-life experience gleaned by attendings and residents is sporadic.
The concept of a mock trial allows clinicians to safely simulate and fully experience a rare yet high-stakes experience. Mock trials are commonly conducted during law school, but have also been used on occasion as an educational tool for clinicians.8-12 Drukteinis, et al found that involving EM residents as “expert witnesses” helped them develop greater comfort and competency when providing expert testimony.9 Lennon, et al reported that while family medicine residents found a mock trail to be an engaging educational tool, most participants struggled to identify the important postintervention takeaways, specifically the ability to name key components of negligence.12
In other professions like commercial aviation, training for and simulating rare, high-risk episodes is a common part of both initial and ongoing training. Bringing together clinicians and lawyers during a mock trial can provide real-world experience in a low-stakes environment.
The goal of the mock trial described in this paper was to teach about the legal process surrounding malpractice trials as well as medical concepts such as bedside ED evaluation, consultation with a specialist, and documentation techniques such as how to document a conversation with a specialist. We chose a case with the common ED chief complaint of chest pain.13 Participants were evaluated with a post mock trial poll to see if this learning modality would lead to change in medical practice and documentation. This is the largest study with the most diverse set of participants on this topic identified in the current medical literature.
METHODS
A mock trial was conducted at a community teaching program in Ohio in September 2020 and was viewed by 642 clinicians located across the U.S. using a teleconference platform (Zoom). The video was archived and could be viewed later, but all the included survey respondents viewed the proceedings in real time. These participants included residents and attendings from the host facility of a community teaching program (including EM, Internal Medicine, Family Medicine and Psychiatry), PA students in a large PA training program, and other clinicians and trainees from outside the host facility who were informed about the program through the CORD listserv, social media, and promotional emails sent to members of a large ED staffing organization and to past participants of this yearly conference (the third annual Adena Thought Leaders Summit). The study was granted IRB exempt status from the Adena Health System institutional review board.
The program started with a description of the case—an actual case and the actual documentation was used—and an interview with a medicolegal expert (Amal Mattu, MD). Following this, a 90-minute mock trial was conducted. The defendant was represented by a volunteer third-year EM resident, and practicing attorneys served as counsel for the plaintiff and the defense. Similarly, two EM attending physicians with extensive real-world medicolegal experience served as the expert witnesses.
The trial included opening statements followed by direct and cross examination of the expert witnesses and the volunteer defendant physician. The trial ended with closing statements from each attorney. Participants completed an online poll after the presentation of the mock trial in which they were asked predetermined questions related to the primary outcomes of effect on practice and documentation.
In addition to demographic and “confirmation of viewing” questions, the specific practice and documentation questions were:
- Based on what you have learned, will your practice of medicine change?
- Based on what you have learned, will your documentation change?
Case Details
The case concerned a 58-year-old man who presented with chest pain, diaphoresis, and radiation of the pain. The initial electrocardiogram from EMS was read by the computer as showing “acute MI suspected.” The initial ECG in the ED was done at 00:03 and was read by the computer as “**Acute MI**.” This was faxed to the interventional cardiologist.
At 00:29 the ED physician discussed the case with the interventional cardiologist. The actual documentation reads:
“Discussed this case with Dr. ___, the on-call physician, called him stat as ekg has concave st elev V1 thru V4 with nonspec st dep inferiorly.”
A second ECG was done in the ED at 00:36 and was read by the computer as showing “**Acute MI**.”
At 00:52 the ED physician discussed the case with the hospitalist who was taking the call from home. The actual documentation reads:
“Discussed this case with Dr. ____, the on-call physician. The patient will be admitted to the hospital. The patient requires intensive care” and “Xray data reviewed, Reviewed EKG”
The patient was admitted to the ICU of this community hospital at 00:52. During the night, the patient continued to have chest pain and another ECG was done at 05:32; it showed new convex upward ST elevation, reciprocal changes, and new right bundle branch block, indicative of an anterior STEMI and subsequent SBP of 76 mmHg despite vasopressor therapy, as well as complete heart block. The patient was taken for cardiac catheterization with percutaneous transluminal coronary angioplasty (PTCA) and stent of the left anterior descending (LAD) coronary artery with intracoronary abciximab and adenosine. Because of continued hypotension the patient had placement of an intra-aortic balloon pump (IABP) and a temporary pacemaker and was then transferred to a tertiary care hospital due to cardiogenic shock.
A lawsuit ensued with allegations of “failure to diagnose” and “delay in diagnosis.”
RESULTS
There were 682 unique views of the conference. After excluding participants who did not answer questions and with incomplete answers to questions and including only those who watched “all” or “almost all” of the mock trial, there were 404 responses composed mostly of EM attendings and EM residents (Table 1).
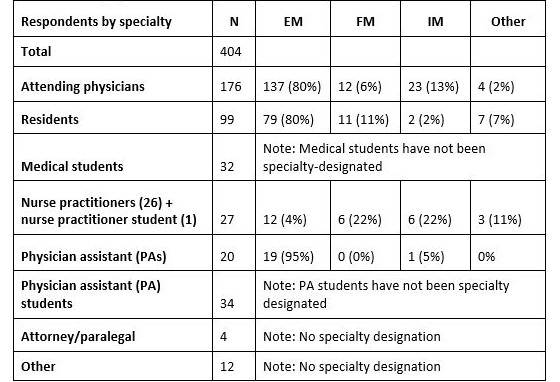
EM, emergency medicine; FM, family medicine; IM, internal medicine
After the trial ended, participants were asked questions in an online poll pertaining to the care rendered. Most (385/404; 95%) felt that “standard of care” was met, but far fewer 212/404 (52%) felt that “excellence in care” was practiced. (Table 2.)
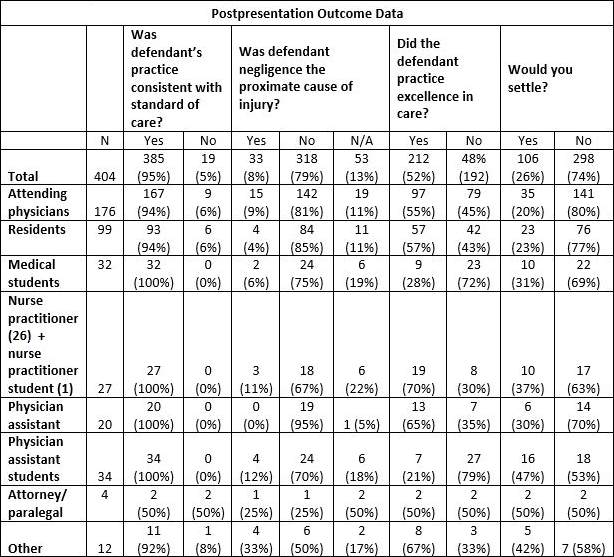
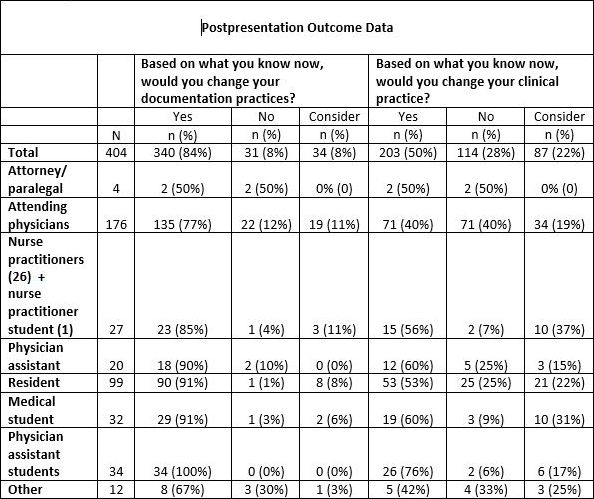
Most participants felt both that they would change or consider changing their clinical practice (290/404; 72%) and that they would change or consider changing their documentation practices 374/404 (93%), based on viewing the mock trial. (Table 3.)
DISCUSSION
While mock trails are a common educational endeavor in law schools, their use in clinician training schools (eg, medical school, PA school, etc.) and residency education programs has been less widespread. To date, when used in a medical setting, mock trials have tended to focus on providing a broad overview of the medicolegal process or have focused more narrowly on preparing participants for potential work as an expert witness.10-12,14 While our mock trial provided an overview of the legal process, the primary goal of our intervention was to provide participants with practical tips that could be used to improve patient safety and documentation, and potentially mitigate their medicolegal risk.
Our data show that when used as an educational endeavor, mock trials can influence future clinical practice. Across a variety of disciplines, participants reported that the defendant met the standard of care and that they did not feel as if the case should be settled with an admission of negligence. Despite being overwhelmingly supportive of the physician’s case, a large majority of participants reported that they would change their practice based on the experience of watching the mock trial.
One of the main points discussed during the presentation involved discrepancies in the medical record. While documentation is often considered to be an area of enhanced risk in lawsuits, to date there appears to be a significant amount of variability when it comes to formal training in this area. Wittels, et al found that only 63% of EM clerkships allowed students to document patient encounters in the medical record. Somewhat ironically, 60% of programs reported that they limited student documentation out of concern for increased medical liability.15 Our data suggest that exposure to a mock trial allowed participants at various levels of training to learn specific techniques that would help them further refine their documentation practices.
Increasing the rate of knowledge translation is a crucial, and at times difficult, goal of all educational endeavors. It is estimated that it takes on average 17 years for new information to work its way into routine clinical practice.16 Novel endeavors such as our mock trial may help reduce this gap between acquisition of new knowledge and implementation at the bedside.
Previous studies have found that participants who stated that they were interested in making practice changes were much more likely to have made these adjustments within 30 days compared with similar participants who did not make similar statements.17 In our study, the majority of participants reported that they would change their clinical practice as a result of the mock trial. This finding is notable in light of the fact that 94% of physician participants stated that they thought the defendant met the standard of care. This willingness to change practice despite being in support of the litigated case suggests that participating in a mock trial may equip clinicians to further refine their medical practice. To our knowledge, this mock trial was seen by the most live viewers in the history of such endeavors, and this is the largest study ever performed of potential for practice change from a mock trial. (Note: The entire video of the trial can be viewed at: https://www.atls2020.com/atls2020. Another example of a mock trial, with some of the same participants, can be viewed at: https://emcrit.org/emcrit/refractory-anaphylaxis-mock-trial/).
LIMITATIONS
Limitations include all the shortcomings inherent in survey data. Though the respondents answered that they would change their documentation and practice, we do not know if this actually occurred. There were participants from many institutions around the country, but the mock trial occurred at only one institution and the results could have been affected by the specific attorneys, experts, and defendant, and therefore may not be generalizable to all emergency clinicians.
Participants were excluded if they did not watch “all or almost all” of the trial, but we did not independently verify whether the 404 included study participants had watched or concentrated on the mock trial uninterrupted. Data were not available on participants who watched the trial but did not complete any of the survey.
CONCLUSION
Although the vast majority of participants maintained that the defendant in the mock trial met the standard of care, a large percentage stated that they planned to change both their future medical practice and documentation as a result of having viewed the mock trial. Our data suggest that the use of mock trials for medical education can influence clinicians’ future practice.
REFERENCES
- Carlson JN, Foster KM, Pines JM, et al. Provider and practice factors associated with emergency physicians’ being named in a malpractice claim. Ann Emerg Med. 2018;71(2):157-164.
- Martin CA, Wilson JF, Fiebelman ND 3rd, et al. Physicians’ psychologic reactions to malpractice litigation. South Med J. 1991;84(11):1300-1304.
- American College of Obstetricians and Gynecologists. ACOG Committee opinion no. 551: coping with the stress of medical professional liability litigation. Obstet Gynecol. 2013;121(1):220-222.
- Michelin DP. Overcoming the stress of malpractice litigation: solutions to help physicians stay healthy and engaged. Mich Med. 2016;115(1):18.
- ACEP: Litigation stress—a primer. Available at: https://www.acep.org/life-as-a-physician/ethics–legal/medical-legal2/litigation-stress—a-primer/. Accessed December 12, 2021.
- Zhao B, Cajas-Monson LC, Ramamoorthy S. Malpractice allegations: a reality check for resident physicians. Am J Surg. 2019;217(2):350-355.
- Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
- Schlicher NR, Ten Eyck RP. Medical malpractice: utilization of layered simulation for resident education. Acad Emerg Med. 2008;15(11):1175-1180.
- Drukteinis DA, O’Keefe K, Sanson T, Orban D. Preparing emergency physicians for malpractice litigation: a joint emergency medicine residency-law school mock trial competition. J Emerg Med. 2014;46(1):95-103.
- Curato M, Shlahet A. Report of a collaboration between a law school and an emergency medicine residency program for a full-scale medical malpractice litigation simulation. AEM Educ Train. 2019;3(3):295-298.
- Baker SE, Ogundipe K, Sterwald C, et al. A winning case? Assessing the effectiveness of a mock trial in a general psychiatry residency program. Acad Psychiatry. 2019;43(5):538-541.
- Lennon RP, Clebak KT, Stepanian JB, Riley TD. Mock trial as a learning tool in a family medicine residency. Fam Med. 2020;52(10):741-744.
- Rui P, Kang K. National Hospital Ambulatory Medical Care Survey: 2017 emergency department summary tables. National Center for Health Statistics. Available at: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2017_ed_web_tables-508.pdf. Accessed January 12, 2021.
- Foley KT, Ferency MJ, Sarzynski EM. Expert witness training for geriatric medicine fellows using courtroom simulation. PRiMER. 2017;8(1):10.
- Wittels K, Wallenstein J, Patwari R, Patel S. Medical student documentation in the electronic medical record: patterns of use and barriers. West J Emerg Med. 2017;18(1):133-136.
- Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. 2011;104(12):510-520.
- Domino FJ, Chopra S, Seligman M, et al. The impact on medical practice of commitments to change following CME lectures: a randomized controlled trial. Med Teach. 2011;33(9):e495-e500.
Author affiliations: Michael Weinstock, MD, Adena Health System; The Wexner Medical Center at The Ohio State University. Kaetha Frost, DO, Adena Health Systems. Heath Jolliff, DO, Ohio University Heritage College of Medicine. Amal Mattu, MD, University of Maryland. Seth McIntire, DO, Adena Health Systems. Marc Calvert, JD, Calvert and Associates. Mark Kitrick, JD, Kitrick, Lewis, and Harris. Matt Delaney, MD, University of Alabama. The authors have no relevant financial relationships with any commercial interests. Drs. Weinstock, Jolliff, Mattu, and Delaney consult as experts in medical malpractice cases. Drs. Calvert and Kitrick are practicing medical malpractice attorneys.
Read More Health Law Articles
- Are You Prepared To Defend Yourself In Court? This Mock Trial Might Help You Figure It Out
- Overview Of A Malpractice Trial (And How To Survive)


