Urgent message: It is important for urgent care providers to be able to recognize the lesser-known arthritides as causes of acute joint pain and to recognize their specific manifestations on x-rays. Further work-up is warranted because some of these diseases can be associated with various metabolic disorders.
MAY MOHTY, MD, FAAP, FAAUCM, and HAMILTON WHITE, MS4
Introduction
The deposition of calcium pyrophosphate dihydrate crystals in and around joints is called CPPD (calcium pyrophosphate dihydrate deposition) disease. This condition manifests in a variety of ways along a spectrum. One manifestation has long been known by the name pseudogout, which is called acute CPP crystal arthritis. This refers to an acute attack of CPP crystal–induced arthritis, which clinically resembles an acute gouty arthritis induced by monosodium urate crystal deposition. CPPD can also contribute to a more chronic osteoarthritis that does not present so acutely. The term chondrocalcinosis refers to calcifications seen in hyaline cartilage on x-rays, and the condition is frequently seen in patients with CPPD disease. Radiographically, a dense line within the hyaline cartilage parallels the articular surface, with concretions of calcium pyrophosphate exuded beyond the subchondral articular surface. Although chondrocalcinosis is often thought of as being synonymous with CPPD disease, it is not seen in all cases of CPPD disease, nor is it specific for CPPD disease when seen.
Because CPPD disease is less well known than other arthritides such as osteoarthritis or rheumatoid arthritis, it is important clinically for providers to be aware of this disorder because it can present similarly to other causes of joint pain. CPPD disease can also be associated with a variety of metabolic disorders, and thus it is important to screen for certain conditions in patients with CPPD disease. The following case shows one way in which CPPD disease may present, plus the appropriate workup necessary once CPPD is suspected.
Case Presentation
A 82-year-old man presented to an urgent care center with pain and swelling in both of his wrists. He reported that the pain felt like soreness in his wrists at rest that is aggravated with pronation and supination. He had been taking acetaminophen, which had provided some relief, but he had avoided taking nonsteroidal anti-inflammatory drugs because his primary-care physician had advised him to do so. He had a history of neuropathy in both hands, and had undergone carpal tunnel surgery on both wrists in the past. He reported no trauma to his hands or wrists that might have caused his current discomfort. His wrist pain had steadily been increasing over the last few weeks to months. A review of systems revealed no rashes, fever, chills, nausea, recent weight loss, or recent illness. Of note in the patient’s chart was a past knee x-ray showing chondrocalcinosis compatible with CPPD disease.
Physical Examination
On initial presentation, the patient’s vital signs were as follows:
- Height: 5 ft 9 in (175.26 cm)
- Weight: 182 lb (82.55 kg)
- Blood pressure: 125/78 mm Hg
- Pulse: 88 beats/min
- Respiratory rate: 18 breaths/min
- Temperature: 98.1°F (36.7°C)
- Oxygen saturation: 98% on room air
Findings on physical examination were significant for circumferential tenderness to palpation over both wrists, along with soft-tissue hypertonicity and swelling that was more prominent over the right wrist. Findings for the Tinel sign were positive bilaterally, and there was notable atrophy of the thenar eminence on the left hand. No neurovascular compromise was detected.
Complete range of motion was intact in both wrists, although movement aggravated the patient’s symptoms. No crepitus was detected with movement.
Laboratory Tests and Imaging
The patient underwent the following laboratory tests:
- Calcium
- Phosphorus (inorganic)
- Alkaline phosphatase
- Serum iron
- Magnesium
- Transferrin
- Thyroid-stimulating hormone
- Ferritin
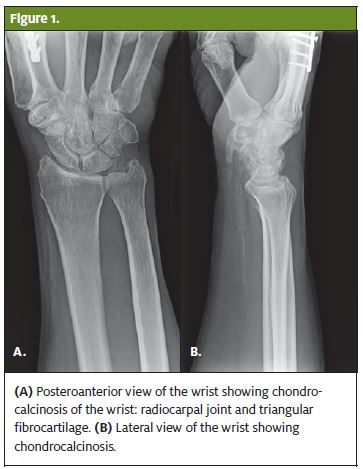
Initial evaluation of the patient began with obtaining an x-ray of the right wrist (Figure 1), which was read as showing moderate osteoarthritis as well as chondrocalcinosis. Calcifications were seen in the radiocarpal joint and in the triangular fibrocartilage.
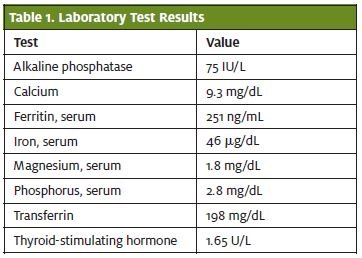
 Because CPPD disease is associated with various metabolic disorders, blood work was done to screen for possible contributing or associated conditions. A definite link has been found between CPPD disease and hyperparathyroidism, hemochromatosis, hypophosphatemia, and hypomagnesemia, but only a possible association has been seen with familial hypocalciuric hypercalcemia, among other conditions.1,2 With this in mind, measurement of the patient’s level of thyroid-stimulating hormone was ordered to rule out thyroid pathology. Tests for serum ferritin, serum iron, and transferrin levels were ordered to screen for hemochromatosis (Table 1). The patient was also screened for hypomagnesemia and hypophosphatemia, because these conditions have also been associated with acute attacks of CPP arthritis and with chondrocalcinosis.3 The patient’s calcium level was also evaluated to determine whether there was underlying hypercalcemia.
Because CPPD disease is associated with various metabolic disorders, blood work was done to screen for possible contributing or associated conditions. A definite link has been found between CPPD disease and hyperparathyroidism, hemochromatosis, hypophosphatemia, and hypomagnesemia, but only a possible association has been seen with familial hypocalciuric hypercalcemia, among other conditions.1,2 With this in mind, measurement of the patient’s level of thyroid-stimulating hormone was ordered to rule out thyroid pathology. Tests for serum ferritin, serum iron, and transferrin levels were ordered to screen for hemochromatosis (Table 1). The patient was also screened for hypomagnesemia and hypophosphatemia, because these conditions have also been associated with acute attacks of CPP arthritis and with chondrocalcinosis.3 The patient’s calcium level was also evaluated to determine whether there was underlying hypercalcemia.
With a diagnosis of CPPD disease suspected, the patient was sent home and instructed to begin a 5-day course of prednisone to decrease the swelling and inflammation in his wrists, and he was told that the results of his blood work would be reported to him. He was instructed to follow up with his primary-care physician to discuss the laboratory results. For all blood work, the results were within normal limits.
Diagnosis
The diagnosis was bilateral wrist pain due to CPPD disease.
Discussion
With the variety of ailments that can cause arthralgic pain, it is important to maintain a high suspicion for CPPD disease as a possible cause. At this time, further clinical research is necessary to clarify the causes of CPPD disease and to discover more effective and lasting treatments. An early and thorough diagnosis, however, can be helpful in detecting and treating other associated conditions that the patient might have.
Epidemiology
The incidence of CPPD disease increases with age, irrespective of race.4 It is common in both males and in females, but slightly more common in females. Younger patients who present with CPPD disease are more likely to have a secondary contributing cause, such as a metabolic disorder. Although the exact incidence of CPPD disease worldwide is unknown, a study in France showed that CPPD disease was the cause of 10,691 hospital admissions between 2009 to 2011 in that country.5
Clinical Presentation
CPPD disease can be difficult to diagnose because the clinical presentation is so varied. The majority of patients with CPPD disease actually do not experience joint symptoms. For those who do experience joint symptoms, CPPD disease can mimic multiple arthritides, such as gout, rheumatoid arthritis, neuropathic arthropathy, and osteoarthritis.6 Clinicians should have a high suspicion for CPPD disease in patients older than 50 years who present with joint pain. Although chondrocalcinosis is frequently seen on images in patients with CPPD, it is not seen in all patients affected by the disease.1 Studies of patients with CPPD disease indicate that the joints most frequently affected by chondrocalcinosis, in descending order of frequency, are knees, wrists, hips, symphysis pubis, and metacarpophalangeal joints. Chondrocalcinosis is usually found bilaterally in all of these joints except at the hips.5
 Treatment
Treatment
Many cases of acute CPP crystal arthritis are self-limited. It is important to screen for other conditions associated with CPPD disease, but attempts at treating these associated diseases unfortunately have not proven to halt the progression of crystal deposition.6 There is a dearth of clinical trials showing proven strategies for treating CPPD disease, and thus most treatment strategies focus on reducing joint inflammation. The European League Against Rheumatism (EULAR) published recommendations in 2011 for the management of CPPD disease. For acute CPP crystal arthritis, they recommend “cool packs, temporary rest and joint aspiration combined with steroid injection.”7 For chronic inflammatory arthritis with CPPD, they recommend the use of nonsteroidal anti-inflammatory drugs or “low-dose colchicine 0.5 to 1.0 mg daily.” They also recommend giving parenteral or oral corticosteroids.
References
- McCarty DJ. Calcium pyrophosphate dihydrate deposition disease—1975. Arthritis Rheum. 1976;19(suppl 3):275–285.
- Announ N, Guerne PA. [Diagnosis and treatment of calcium pyrophosphate crystalinduced arthropathy.] [Article in German.] Z Rheumatol. 2007;66:573–578.
- Jones AC, Chuck AJ, Arie EA, et al. Diseases associated with calcium pyrophosphate deposition disease. Semin Arthritis Rheumatol. 1992; 22:188–202.
- Saffar P. Chondrocalcinosis of the wrist. J. Hand Surg [Br]. 2004;29:486–493.
- Abhishek A. Calcium pyrophosphate deposition disease: a review of epidemiologic findings. Curr Opin Rheumatol. 2015;28:133–139.
- Rosenthal AK, Ryan LM, McCarthy DJ. Calcium pyrophosphate crystal deposition disease, pseudogout, and articular chondrocalcinosis. In: Koopman WJ, Moreland LW, eds. Arthritis and Allied Conditions. 15th edition. Philadelphia, PA: Lippincott Williams & Wilkins; 2005:2373.
- Zhang W, Doherty M, Pascual E, et al. EULAR recommendations for calcium pyrophosphate deposition. Part II: management. Ann Rheum Dis. 2011;70:571–575.

