Published on
Shomel Gauznabi, MBChB, FRNZCGP, FRACGP, FRNZCUC, MD; Ivan Koay, MBChB, MRCS, FRNZCUC, MD
Urgent Message: There is literature supporting that regional anesthesia, specifically hematoma blocks, is a safe, effective, and well tolerated alternative to procedural sedation for the management of pediatric forearm fractures.
Citation: Gauznabi S, Koay I. Systematic Rapid Review: Efficacy of Hematoma Blocks for Pediatric Forearm Fractures. J Urgent Care Med. 2024; 19(x):42-50
Key Words: pediatric forearm fractures, anesthesia, hematoma blocks, urgent care
Author Affiliations: Shomel Gauznabi MBChB. FRNZCGP. FRACGP. FRNZCUC, University of Auckland, New Zealand. Ivan Koay MBChB, MRCS, FRNZCUC, MD, Kings College Hospital Urgent Treatment Centre, London; Royal New Zealand College of Urgent Care.
Abstract
Introduction: Forearm fractures are a common injury, especially in the pediatric population. There is significant variation in the use of anesthesia and analgesia techniques used to facilitate closed reduction of pediatric forearm fractures. In recent decades, there has been a trend towards favoring procedural sedation (PS) for reducing such fractures. As procedural sedation is not generally feasible in urgent care (UC), it is worthwhile to understand if current available evidence supports its use in terms of better outcomes for reduction and patient and caregiver experience compared to various methods of regional anesthesia, specifically hematoma blocks (HB).
Aim:The objective of this study was to conduct a rapid literature review of studies looking at the efficacy of the use of HB for pediatric forearm fractures.
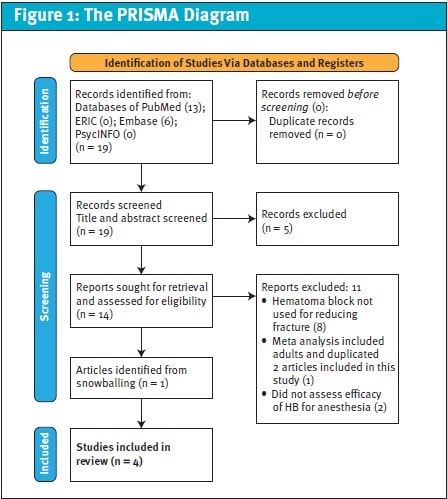
Methods: A systematic rapid literature search with predefined key terms was performed in December 2023 assessing the relevant peer-reviewed articles from the databases of PubMed, ERIC, Embase, and PsycINFO that met the inclusion criteria. Only journal articles in English with full texts were included. Utilizing the Preferred Reporting Items for Systematic Reviews and Meta-Analyses framework (PRISMA), data extraction was systematically structured, and the included studies were appraised systematically.
Results: Four of the initial 19 studies returned from the search met the inclusion criteria for this study. The results of all 4 studies were consistent in finding HB adequate for providing sufficient analgesia and allowing for non-inferior closed reductions of pediatric forearm fractures when compared to PS.
Discussion: This literature review supports use of HB in achieving successful analgesia and non-inferior results in closed reduction of forearm fractures in the pediatric population. However, most pediatric forearm fractures are initially managed with PS for anesthesia. In comparison to PS, hematoma blocks require fewer resources and have a lower risk of complication. The included studies demonstrated that HB provides adequate analgesia for closed reduction of pediatric forearm fractures without compromising radiographically determined outcomes of reduction success. We propose, especially in a UC setting where PS is largely unavailable, use of HB is worthy of consideration as a first-line method of anesthesia for pediatric forearm fractures warranting reduction. Emergency department referral for specialist consultation and/or PS therefore can be reserved for patients in whom this lower risk, lower resource strategy proves unsuccessful.
Introduction
Distal radius fractures (DRFs) are the most common fracture of the upper extremity with a bimodal peak incidence among children and older adults.1 DRFs account for 45% of all pediatric fractures and are commonly treated in the emergency department (ED) with closed reduction facilitated by procedural sedation.2-4 In contrast to adults, pediatric DRFs require less precise reduction, as children’s bones have better remodeling potential, which declines with increasing age.5,6 Closed reduction and immobilization is typically definitive treatment for children who sustain DRF, even if significantly displaced or angulated; surgical open reduction and internal fixation (ORIF) is therefore performed much less commonly than in adults.7, 8, 9 For this reason, performing an adequate initial closed reduction shortly after injury is critical for angulated and displaced pediatric forearm fractures to have optimal outcomes without surgery.7 Despite children’s ability to recover normally with a greater degree of post-reduction deformity, outcomes are best when as near anatomical alignment is achieved by the closed reduction procedure.5 Pain during reduction is disconcerting for patients and caregivers and may also impede the mechanics of successful reduction.10 Conversely, adequate levels of analgesia and/or anesthesia facilitate successful closed reduction and minimize pain and anxiety for both the child and parent.7, 11
A variety of anesthesia strategies may be employed when attempting closed fracture reduction, including various non-sedating regional anesthesia techniques (eg, hematoma blocks [HB], Bier block [BB], axillary, or supraclavicular block), or procedural sedation (PS) using agents such as ketamine, propofol, opioids, and/or midazolam.12-16 Procedural sedation is defined as use of sedatives or dissociative agents with/without analgesics to induce a state that allows the patient to tolerate a procedure without compromising cardiorespiratory function—differentiating it from general anesthesia. PS remains among the most commonly employed strategies for DRF reduction in children in the ED setting, however, it is a less common option in urgent care (UC) settings.11, 17, 18 Although PS has been shown to allow for good outcomes with closed DRF reductions, it carries risks, such as vomiting, dysphoria, hallucinations, respiratory depression, airway obstruction, and laryngospasm.11,19 Furthermore, PS requires extensive healthcare resources and prolonged monitoring, which makes it impractical for use in the UC setting.
An ideal anesthetic agent for UC would be easy to administer, effective, safe, inexpensive, agreeable to patients and parents, rapidly provided, and not require monitoring or special equipment.20 Regional anesthesia (RA) such as HB meets most of these criteria and can be performed in the ED or UC as an alternative to PS.21 A HB is defined as a procedure where local anesthetic is injected directly into the fracture site.10 However, many clinicians have less confidence in the appropriateness and efficacy of HB in children compared to adults,10 despite limited evidence to inform an opinion on the matter. This perception allows for continued preferential use of PS over alternative, less resource intensive means of achieving anesthesia that may be equally effective.
The objective of this study was to review the available literature regarding the use of HB in children with acute forearm fractures requiring manipulation and compare relative analgesic efficacy, anxiolytic effects, adverse effects (AE) of the procedure, and the outcomes of reduction when compared to PS.
Methods
Search Strategy
A systematic literature search was conducted in December 2023 following international guidelines.22 This rapid review protocol follows the PRISMA guideline.23 The MeSH terms used in conjunction with Boolean operators were *Regional anesthesia OR regional block OR hematoma block AND *Forearm OR Ulnar OR Radius Fracture* AND *Pediatric OR Children*. These MeSH terms provided focused and appropriate article results without returning irrelevant articles. No date ranges of publications were used given the few number of studies returned in the preliminary search. Snowballing, a research technique used to identify eligible studies from the references of included studies, was used to identify further eligible articles to include in the review.
Study Collection Criteria
Only journal articles were included in the review; grey literature such as reports and documents that were not published in academic journals were excluded. The studies included ranged from quasi-experimental, retrospective medical record review, prospective cohort design, and randomized controlled trial.
The inclusion criteria were: exclusively pediatric subjects (defined as an age <18 years); endpoints of efficacy and adverse effects of the use of HB for forearm fracture reduction; ED or outpatient setting; full text available; and English language publication. The exclusion criteria were: grey literature; non-peer reviewed publications; and case reports.
Data extraction
After removing duplicate articles, the abstracts of results returned were reviewed to ensure they met the eligibility criteria of this review. The full texts of each were then further analyzed to confirm that it met inclusion criteria. Data extraction was standardized to compare each study’s aims, design methods, setting, participant demographics, outcomes, quality review, and suitability for inclusion.
Quality Appraisal
Study quality assessment was completed for each publication meeting the initial screening for inclusion criteria. Joanna Briggs Institute’s Critical Appraisal Tools were used to evaluate the quality of publications.24 There was collaboration of the analysis of eligible articles and validating the findings, but all the preceding steps were completed systematically by a sole author (SG). Rapid reviews usually involve peer review throughout the literature review, but it can be completed by a sole researcher that follows a systematic approach with a predetermined search protocol, predefined inclusion criteria and systematic data extraction.24-26 This review was carried out in a structure consistent with this approach.
Results
A PRISMA flow chart was used to record the data extraction process (Figure 1).
From the initial search, 19 studies were identified. The studies contained the following databases : PubMed (n=13 results), ERIC (n=0 results), Embase (n=6 results), and PsycINFO (n=0 results). Of these 19 studies, the abstracts were screened to ensure they fully met the eligibility criteria for inclusion. The full texts of these 14 articles then underwent further analysis to determine if articles met the determined inclusion criteria. The reference lists of all studies that underwent full-text analysis were then reviewed to identify further potential eligible studies. This identified 1 additional eligible study, leading to 4 studies total included in the final review.
The systematic literature review established 4 articles in the wider literature that meet the study eligibility criteria.
The included articles were highly heterogenous in their study populations, design, and geography. Three studies were conducted in the United States, and 1 was conducted in India. Two of the studies reviewed the use of HB in comparison to PS for DRFs specifically.7, 15 These studies were interventional studies. One compared the use of RA for diaphyseal forearm fractures.25 One study, Sulton et al., included all pediatric forearm fractures but defined RA as either BB or HB, and compared this to PS 25. This was the only retrospective electronic medical record (EMR) review.
The studies each used different medications for the PS group. The HB groups also had some variability with the doses ranging from 5-15 mL of 1% lidocaine without epinephrine. There was also heterogeneity in the average subject age and the ages included in the study. Similarly, the eligibility criteria varied between studies. The majority of the studies evaluated procedural success (ie, adequacy of reduction), efficacy of analgesia, and proceduralist, patient, and parental satisfaction between the interventional arms. However, the validated scoring tools used to measure these outcomes varied as well. The overall participant numbers included in each study were not significant, however, this was particularly small for Sulton et al. as they included both BB and HB under the RA arm.
Despite these differences between studies, the results were consistent across all publications: HB provided excellent reduction outcomes; excellent analgesia and anxiolysis; and was found to be satisfactory by the proceduralist, patient, and their family.7, 15, 19, 25 Additionally, the aggregate results suggest that analgesia provided by HB is comparable to that of PS and did not compromise the immediate likelihood of successful reduction or long-term outcomes.19, 25
In all studies, adverse effects in the RA groups were statistically less frequent than in the PS groups. All studies demonstrated that the RA groups had significantly shorter length of stay (LOS) during their ED visit. The largest time difference, found in the Bear et al. study, was an average reduction of 2 hours in the ED LOS for the RA group.7 Refer to Table 1 for a summary of the literature review findings.
| Table 1. Literature Review Findings Summary – Systematic Rapid Review: Efficacy of Hematoma Blocks for Pediatric Forearm Fractures | |
|---|---|
| Article: Hematoma Block Versus Sedation for the Reduction of Distal Radius Fractures in Children, 2015 Author: Bear et al.7 | |
| Aim: Hematoma block (HB) vs. procedural sedation (PS) for distal radius fractures. Method: Quasi-experimental study Pittsburgh, Penn., USA; 2012 to 2014. PS regime – Initial intravenous (IV) ketamine, midazolam, and atropine. HB regime – 10 mL of 1% lidocaine (100 mg). IV morphine or oral midazolam provided at doctor’s discretion. | Findings: 52 children, 26 each in each arm. Ages 5-16. Similar demographic in both groups. No difference between groups with overall patient satisfaction or satisfaction with anesthesia. Patients receiving HB spent an average ED LOS of 134 min less than the PS group (P < .001). No significant differences in reduction outcome. |
| Strengths: Prospective, interventional study, similar subject characteristics in both groups. | Weaknesses: Single center trial. Lack of randomization and blinding. Majority of patients were age 9 and older. |
| Article: Regional Anesthesia as an Alternative to Procedural Sedation for Forearm Fracture Reductions in the Pediatric Emergency Department, 2023 Author: Sulton et al.19 | |
| Aim: Regional anesthesia (RA) Bier block or HB vs. PS for reducing forearm fractures. Method: Retrospective EMR review of pediatric DRF in 2 urban pediatric EDs in the USA. Ages 2 to 18 years between 2016 to 2021. Cohorts were matched to reduce selection bias. PS regime – ketamine +/- propofol. HB regime – 1% lidocaine without epinephrine | Findings: 642 in RA group (636 received BB, 6 received HB). Similar characteristics between the matched cohorts. 13% of PS encounters had an AE with only 0.2% in the RA cohort, P<0.001. Most common AE was hypoxia (9.8%) and upper airway obstruction (3.2%) only occurring in the PS. No reduction failures in either group. LOS was on average 27 minutes less for the RA group. (p<0.001). |
| Strengths: Research procedure well-detailed. Large number of patients. | Weaknesses: Retrospective cohort analysis. Only 6 patients received a HB. |
| Article: Reduction of Forearm Diaphyseal Fractures In Children Under Hematoma Block In Emergency: A Prompt and Cost-Effective Approach, 2021 Author: Mander et al.25 | |
| Aim: Review closed reduction of radius or ulnar diaphyseal fractures under HB. Method: Prospective cohort study in India. 5-11 years with diaphyseal forearm fracture; 2019 to 2020. HB group – 5mL of 2% lidocaine (100 mg). | Findings: Total of 20 patients. 70% had both radius and ulnar diaphyseal fractures. 4 cases (20%) lost alignment and required repeat intervention. The remaining had no issues with reduction. |
| Strengths: Prospective, Interventional study. Follow-up available up to 6 months post-treatment. | Weaknesses: Small sample. Only included diaphyseal forearm fractures. |
| Article: A Randomized Comparison of Nitrous Oxide Plus Hematoma Block Versus Ketamine Plus Midazolam for Emergency Department Forearm Fracture Reduction in Children, 2006 Author: Luhmann et al.15 | |
| Aim: Compare PS vs. RA – nitrous oxide and hematoma block (N2O/HB), for forearm fracture reduction. Method: Randomized controlled trial. Ages 5 to 17 ED in St. Louis, USA; patients who required reduction of mid- to distal forearm fractures. PS group: midazolam + ketamine. HB regime: 50% N2O and O2 before HB with a maximum of 150 mg (15 mL of 1% lidocaine). | Findings: 102 children, 55 in PS and 47 in RA group. Similar demographics across both cohorts. Both groups had very little distress during procedure. Mean recovery time was significantly shorter for children who received N2O/HB (16 minutes) compared with PS (83 minutes). More parents of those children who underwent N2O/HB would opt to repeat this method. Orthopedic surgeon assessment reported no difference in satisfaction of reductions both groups. |
| Strengths: Randomized design. Blinded evaluator of pain and distress levels. Reasonably sized study population. | Weaknesses: True blinding was not possible given study methodology. Singler center study. Follow-up to only 24 hours post-discharge. HB block group also received nitrous oxide for anxiolysis |
Discussion
Although there are relatively few articles that explore the use of HB for facilitating reduction of forearm fractures in children, this literature review confirms a consensus of evidence supporting the adequacy of HB for achieving sufficient analgesia to allow for appropriate closed reduction of forearm fractures in the pediatric population.7, 10, 15, 19, 25
Although not all forearm fractures are amenable to RA or HB, HB would be reasonable for most pediatric forearm fractures that require closed reduction.7 Furthermore, many pediatric forearm fractures, such as buckle/torus fractures or minimally displaced fractures, do not require any manipulation.9 The efficacy and safety of BB and HB approaches to RA have been well studied in adult populations12, 13, 17 and also show a low risk of AE or toxicity with appropriate dosing.26 However, as this review demonstrates, the use of RA prior to closed reduction of pediatric forearm fractures is less well studied.27 This lack of evidence may contribute to limited use of these anesthesia techniques in children with forearm fractures in favor of PS.11, 17, 18
For example, in a survey of U.S. and Canadian pediatric orthopedic and emergency physicians, 42% of respondents reported they used RA for pediatric forearm fractures “rarely” or “never.” Among the 22% of respondents who reported never using RA, there was a pervasive belief reported that it would provide insufficient analgesia.27 This belief, however, is not substantiated by prior studies 7 or by the findings of this literature review.
HB anesthesia represents a less resource intensive alternative to PS for analgesia in the reduction of pediatric forearm fractures and existing evidences suggest it is not inferior to PS.7 The findings of this review also confirm the obvious benefits of HB in UC. The anesthetic agent used is widely available, easy to administer, effective, safe, and inexpensive. It can be provided rapidly and is agreeable to patients and parents, while not requiring monitoring or special equipment.20 HB satisfies these criteria for the majority of cases of forearm fractures.7 PS has its own limitations, including an exposure to numerous medications with potential side effects, need for physicians with competence in airway management and registered nurses to provide continuous monitoring due to the risk of hypotension and airway compromise. The medications, equipment, and staff required to perform such PS is rarely available in UC settings, nor does the time required for PS and recovery fit into the UC model of patient flow. The articles included in the literature review demonstrated that using RA reduced ED LOS up to 2 hours.7 This benefit is exactly why HB is particularly appealing for use in UC settings and may prevent the need for ED referrals, especially given unanimous support for its safety and efficacy in the existing literature.
Although we did not assess cost-effectiveness of HB compared with PS, there are reduced direct and indirect costs such as staffing, costs of medications, and opportunity costs of seeing other patients during PS and monitoring.9,10 HB can also be performed much more rapidly, does not require IV access, has decreased demands of clinicians’ time, and has fewer risks. HB importantly also provides adequate analgesia (which extends into the post-procedure period) without compromising radiographic outcomes of reduction adequacy.13, 28, 29
Although RA is generally well tolerated, in younger children (<6 years) the anxiolytic benefits of PS may be superior.16, 27,20, 30 This may limit the utility of RA in the management of pediatric forearm fractures in preschool aged children.
Strengths of Literature Review
This literature review, the first of its kind on this topic, was conducted systematically, with clearly specified search parameters, inclusion and exclusion criteria. A systematic approach to quality appraisal was applied as well to limit researcher bias.
Several studies compared HB directly to PS, which helps increase the applicability of the findings to the clinical question the review aimed to address. All studies included had similar outcome measures: quality of reduction; adequacy of analgesia and anxiolysis in patients, parents and clinician; LOS; and AE.
Limitations of Literature Review
All steps in a “rapid review” approach are completed with collaboration from multiple authors, however, it is still possible to undertake the review with a sole researcher if a systematic process is undertaken.23 In this review, all authors participated in determination of eligible articles, but subsequent steps were completed systematically by a sole author (SG).
Overall, the small number of studies on this specific topic is the main limitation in interpreting the results of this review. The aggregate number of patients across all 4 studies was small (<800 children), and the study design was unsurprisingly somewhat heterogenous. Only a single study used a randomized, blinded, and prospective design, which would be ideal for increasing certainty as to the lack of confounding.
This literature review did not explore other forms RA, such as periosteal nerve blocks, axillary nerve or other peripheral nerve blocks, or BB. These forms of RA were intentionally not included because these forms of RA are generally outside the scope and training of many UC clinicians.19 As previously mentioned, due to the ages of subjects included in the studies reviewed, the applicability of the findings of this review in patients less than 6 years is uncertain.
Recommendations
When encountering situations where closed reduction of pediatric forearm fractures is indicated, HB would be appropriate to consider as the first-line method of anesthesia, especially in UC settings.7, 25 When RA does not provide adequate anesthesia, use of PS would remain an option although it may involve referral to an ED setting.7
Future studies on this topic should use prospective design and randomization as much as able to limit bias and confounding. Additionally, UC-based studies could confirm that this approach is safe, effective, and feasible outside of ED settings.
Although less extensively studied, for middle to distal forearm fractures, lidocaine HB can augment the benefits of N2O based sedation and analgesia, 31 and this could be further studied as N2O requires fewer staff and resources than IV medication based PS. Luhmann et al. demonstrated the efficacy of the combination of N2O/HB in fracture reduction outcomes, analgesia, anxiolysis, and acceptability for parents, patients, and interventionalists.15 However, there may be disadvantages of using the N2O/HB combination compared to using HB alone or PS and this should be further explored.15
Conclusion
Overall, this literature review summarizes the existing evidence on the use of HB to facilitate closed reduction forearm fractures in children. While studies are few in number, there are consensus results which indicate that RA, and specifically HB, is a safe, effective, and well tolerated alternative to PS for the management of pediatric forearm fractures.
Manuscript submitted May 18, 2024; accepted October 7, 2024.
References
- Alluri RK, Hill JR, Ghiassi A. Distal Radius Fractures: Approaches, Indications, and Techniques. The Journal of Hand Surgery. 2016;41(8):845-854. doi:https://doi.org/10.1016/j.jhsa.2016.05.015.
- Wiik AV, Patel P, Bovis J, et al. Use of ketamine sedation for the management of displaced paediatric forearm fractures. World Journal of Orthopedics. 2018;9(3):50-57. doi:https://doi.org/10.5312/wjo.v9.i3.50.
- Rimbaldo KM, Fauteux-Lamarre E, Babl FE, Kollias C, Hopper SM. Deformed pediatric forearm fractures: Predictors of successful reduction by emergency providers. The American Journal of Emergency Medicine. 2021;50:59-65. doi:https://doi.org/10.1016/j.ajem.2021.06.073.
- Chinta SS, Schrock CR, McAllister JD, Jaffe DM, Liu J, Kennedy RM. Rapid Administration Technique of Ketamine for Pediatric Forearm Fracture Reduction: A Dose-Finding Study. Annals of emergency medicine. 2015;65(6):640-648.e2. doi:https://doi.org/10.1016/j.annemergmed.2014.12.011.
- Bin K, Rony L, Henric N, Moukoko D. Pediatric fracture reduction in the emergency department. Orthopaedics & Traumatology: Surgery & Research. 2022;108(1, Supplement):103155. doi:https://doi.org/10.1016/j.otsr.2021.103155.
- Waters PM, S.D., Flynn JM, Fractures in Children. Lippincott Williams&Wilkin, 2019.
- Bear, D.M., et al., Hematoma block versus sedation for the reduction of distal radius fractures in children. J Hand Surg Am. 2015. 40(1): p. 57-61.
- Flynn JM, Skaggs DL, Waters PM. Rockwood & Wilkins Fractures in Children Print. Wolters Kluwer Health; 2014.
- Clinical Practice Guidelines : Distal radius and or ulna metaphyseal fractures – Emergency Department. www.rch.org.au. Accessed July 23, 2024.
- Tseng PT, Leu TH, Chen YW, Chen YP. Hematoma block or procedural sedation and analgesia, which is the most effective method of anesthesia in reduction of displaced distal radius fracture? Journal of Orthopaedic Surgery and Research. 2018;13(1). doi:https://doi.org/10.1186/s13018-018-0772-7.
- McCarty EC, Mencio GA, Green NE. Anesthesia and Analgesia for the Ambulatory Management of Fractures in Children. Journal of the American Academy of Orthopaedic Surgeons. 1999;7(2):81-91. doi:https://doi.org/10.5435/00124635-199903000-00001.
- Singh GK, Manglik RK, Lakhtakia PK, Singh A. Analgesia for the reduction of Colles fracture. A comparison of hematoma block and intravenous sedation. Online J Curr Clin Trials. 1992;Doc No 23:.
- Funk L. A prospective trial to compare three anaesthetic techniques used for the reduction of fractures of the distal radius. Injury. 1997;28(3):209-12. doi:https://doi.org/10.1016/s0020-1383(96)00183-0.
- Kriwanek KL, Wan J, Beaty JH, Pershad J. Axillary Block for Analgesia During Manipulation of Forearm Fractures in the Pediatric Emergency Department A Prospective Randomized Comparative Trial. Journal of Pediatric Orthopaedics. 2006;26(6):737-740. doi:https://doi.org/10.1097/01.bpo.0000229976.24307.30.
- Luhmann JD, Schootman M, Luhmann SJ, Kennedy RM. A Randomized Comparison of Nitrous Oxide Plus Hematoma Block Versus Ketamine Plus Midazolam for Emergency Department Forearm Fracture Reduction in Children. Pediatrics. 2006;118(4):e1078-e1086. doi:https://doi.org/10.1542/peds.2005-1694.
- Aarons C, Fernandez MD, Willsey M, Peterson BC, Key CR, Fabregas J. Bier Block Regional Anesthesia and Casting for Forearm Fractures. Journal of Pediatric Orthopaedics. 2014;34(1):45-49. doi:https://doi.org/10.1097/bpo.0b013e31829fff47.
- Godambe SA, Elliot V, Matheny D, Pershad J. Comparison of Propofol/Fentanyl Versus Ketamine/Midazolam for Brief Orthopedic Procedural Sedation in a Pediatric Emergency Department. Pediatrics. 2003;112(1):116-123. doi:https://doi.org/10.1542/peds.112.1.116.
- Mitchell L, Archer E, Middleton S, et al. Paediatric distal radial fracture manipulation: multicentre analysis of process times. Emergency Medicine Journal. 2009;26(1):41-42. doi:https://doi.org/10.1136/emj.2007.057208.
- Sulton CD, Fletcher N, Murphy J, Gillespie S, Burger RK. Regional Anesthesia as an Alternative to Procedural Sedation for Forearm Fracture Reductions in the Pediatric Emergency Department. Pediatric Emergency Care. 2023;40(2):83-87. doi:https://doi.org/10.1097/pec.0000000000002993.
- Blasier RD. Anesthetic Considerations for Fracture Management in the Outpatient Setting. Journal of Pediatric Orthopaedics. 2004;24(6):742-746. doi:https://doi.org/10.1097/01241398-200411000-00027.
- Constantine E, Tsze DS, Machan JT, Eberson CP, Linakis JG, Steele DW. Evaluating the Hematoma Block as an Adjunct to Procedural Sedation for Closed Reduction of Distal Forearm Fractures. Pediatric Emergency Care. 2014;30(7):474-478. doi:https://doi.org/10.1097/pec.0000000000000164.
- Smela B, Toumi M, Świerk K, Francois C, Biernikiewicz M, Clay E, Boyer L. Rapid literature review: definition and methodology. J Mark Access Health Policy. 2023 Jul 28;11(1):2241234. doi: 10.1080/20016689.2023.2241234.
- Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine. 2018;169(7):467-473.
- Joanna Briggs Institute (JBI). Critical appraisal tools. JBI. Published 2020. Access 25/07/2024. https://jbi.global/critical-appraisal-tools.
- Mander H, Ashraf A, Singh GP, Gupta N, Vaibhav B, Verma S. Reduction of forearm diaphyseal fractures in children under haematoma block in emergency: A prompt and cost-effective approach. International Journal of Orthopaedics Sciences. 2021;7(4):760-763. doi:https://doi.org/10.22271/ortho.2021.v7.i4k.2965.
- Meinig RP, Lynette Lobmeyer AQ. Plasma Lidocaine Levels Following Hematoma Block for Distal Radius Fractures. Journal of Orthopaedic Trauma. 1989;3(3):187-191. doi:https://doi.org/10.1097/00005131-198909000-00001.
- Constantine E, Steele DW, Eberson C, Boutis K, Amanullah S, Linakis JG. The Use of Local Anesthetic Techniques for Closed Forearm Fracture Reduction in Children. Pediatric Emergency Care. 2007;23(4):209-211. doi:https://doi.org/10.1097/pec.0b013e31803e1792.
- Case RD. Haematoma block—a safe method of reducing Colles’ fractures. Injury. 1985;16(7):469-470. doi:https://doi.org/10.1016/0020-1383(85)90168-8.
- ohnson PQ, Noffsinger MA. Hematoma block of distal forearm fractures. Is it safe? Orthop Rev. 1991 Nov;20(11):977-9.
- Kennedy RM, Luhmann JD, Luhmann SJ. Emergency department management of pain and anxiety related to orthopedic fracture care: a guide to analgesic techniques and procedural sedation in children. Paediatr Drugs. 2004;6(1):11-31. doi: 10.2165/00148581-200406010-00002.
- Hennrikus WL, Simpson RB, Klingelberger CE, Reis MT. Self-administered nitrous oxide analgesia for pediatric fracture reductions. J Pediatr Orthop. 1994 Jul-Aug;14(4):538-42. doi: 10.1097/01241398-199407000-00023.
Download the Article PDF: Systematic Rapid Review: Efficacy of Hematoma Blocks for Pediatric Forearm Fractures

