Urgent Message: Steroid overprescribing is a universal urgent care issue. While systemic steroids have several indications in which the preponderance of evidence supports their use in the urgent care setting, indication creep has led to their use outside of these scenarios resulting in significant risk for avoidable and unjustifiable adverse reactions.
Citation: Hansen P. Systemic Steroid Stewardship in Urgent Care: Recognizing Indication Creep to Limit Avoidable Harms. J Urgent Care Med. 2023;18(3);29-32
Author Affiliation: Paul Hansen, MD, FAAP, FACP, Mercy GoHealth. The author has no relevant financial relationships with any commercial interests.
Introduction
Systemic steroids have several evidence-based indications and can be powerful tools for various acute issues when used appropriately in urgent care (UC) settings. However, over recent decades, “indication creep” has occurred in the clinical use of systemic steroids due to a variety of factors, such as perceived versatility, relatively rapid onset of profound biological effects, pressure from patient expectations for the receipt of a prescription, as well as a general perception among healthcare providers that short courses of steroids are relatively innocuous.1 Indication creep refers to the increasingly widespread use of a given therapy outside of clinical scenarios of proven benefit.2 Other common examples of indication creep include the use of antibiotics for the treatment of acute bronchitis3 or sinusitis that is not persistent, severe, or suggestive of a “double-sickening” illness script.4,5
This trend, combined with the data from publications in the last decade outlining the harms of even short courses of corticosteroids, provide justification for the College of Urgent Care Medicine to publish a position statement advocating for “steroid stewardship.”6,7,8,9 In UC, steroids are frequently used, often in situations where there is limited or no evidence of benefit, and consequently can cause avoidable harm.6,7,8,10,11
COVID-19: A Case Study in Indication Creep
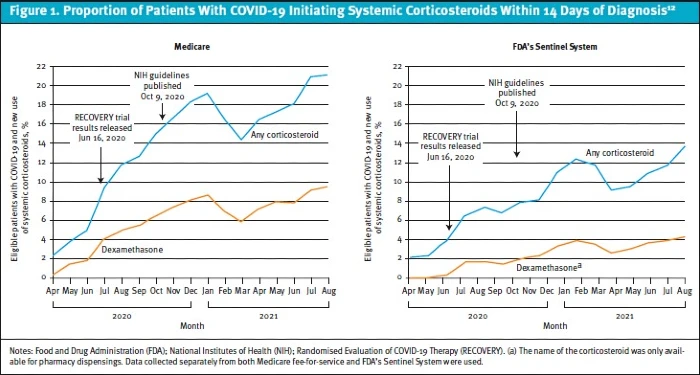
When looking for an example of systemic corticosteroid indication creep in the UC and outpatient settings, COVID-19 serves as a useful example. The publication of top line results of the RECOVERY trial in June 2020 led to headlines heralding the life-saving potential of dexamethasone without a similar emphasis that benefits were seen only among hospitalized patients requiring supplemental oxygen and that there was actually a trend toward harm when systemic steroids were given to hospitalized patients who did not have a new or worsening oxygen requirement.12Thus, despite the publication of National Institutes of Health treatment guidelines advising against systemic steroid prescribing for outpatients with COVID-19 who did not require supplemental oxygen, an alarming trend of increasing corticosteroid use in outpatients with COVID-19 has been observed (Figure 1).13 This trend prompted the Centers for Disease Control and Prevention (CDC) to issue a health advisory in April of 2022.14
Outpatient Short Course Systemic Steroid Use is Increasingly Common
Short course steroid use, variably defined in publications as less than 14 (Yao, 2020; Yao 2021)6,7 to 30 days (Waliee, 2017),8 has risen dramatically in outpatient and acute care settings over the past 20 years. This is not a uniquely American phenomenon. Below are a few examples from large/populationwide studies.
- France: use increased from ~15% to 17% from 2007 to 2013.11
- Taiwan: 1 in 4 adults6 and 4 in 10 children7 received a steroid burst over a 3- and 5-year period in the 2010s, respectively.
- United States: ~1 in 5 adults received a steroid script from 2012-2014.8
Commonly Used for Avoidable Indications
The use of short course systemic steroids (SCSS) is supported by evidence-based guidelines for patients presenting with conditions such as acute asthma or chronic obstructive pulmonary disease exacerbations, children with croup, toxicodendron species related dermatitis, acute gout, or Bell’s Palsy.15,16,17However, prescribing of SCSS outside of these indications in the UC setting is an increasingly frequent phenomenon.10
Common examples of avoidable SCSS use include:
- Acute Respiratory Infections (ARI): including viral upper respiratory infections, acute bronchitis, pneumonia, acute sinusitis, non-severe acute pharyngitis, acute otitis media.15
- A U.S. study showed that the proportion of adult patients with an ARI receiving a systemic steroid increased from 10% in 2008 to 17% in 2016, with significant geographic variability noted. As an example, patients were greater than 14 times more likely to receive a parenteral steroid in the south compared to the northeast.10 The etiology for these striking regional variances is likely multifactorial and have not been fully explored. Of note, there is considerable geographic overlap when comparing SCSS for ARI to the overall and inappropriate antibiotic use variance previously described, the latter of which bolstered the rationale for antibiotic stewardship efforts. Furthermore, the degree of regional variance appears to be an order of magnitude more drastic for SCSS than for antibiotics for ARI, respectively.18,19,20
- Unfortunately, UC centers have been the worst offenders in SCSS for ARIs, using systemic corticosteroids about 25% more frequently than primary care, twice as often as retail walk-in clinics, and slightly more than emergency departments.10
- Unfortunately, UC centers have been the worst offenders in SCSS for ARIs, using systemic corticosteroids about 25% more frequently than primary care, twice as often as retail walk-in clinics, and slightly more than emergency departments.10
- Allergic Rhinitis: Given that nasal steroids have been shown to be equally as effective without the risk of avoidable harms of systemic steroids, current allergy and otolaryngology treatment guidelines do not recommend SCSS.15,21,22 Despite this, nationwide unadjusted claims data shows that greater than 1 in 10 adult US patients diagnosed with allergies received a SCSS.10
- Non-Radicular Low Back Pain: Utilizing SCSS for back pain is a common practice pattern, despite clinical practice guidelines recommending against their use.8,23 In the United States, back pain was the second most common indication for SCSS use behind ARIs.8 While a recent Cochrane meta-analysis showed modest benefit for patients with radicular low back pain, there was no improvement in pain, short- or long-term function, need for surgery, or improvement in quality of life for patients with non-radicular low back pain or spinal stenosis.24,25
Increased Risk for Various Adverse Outcomes
Classically, a provider prescribing a steroid “burst” would discuss certain commonly known risks associated with SCSS, including hyperglycemia, insomnia, changes in mood and appetite, and dyspepsia in adults, and possibly that repeat courses of steroids in children can negatively impact a child’s growth trajectory.26 Unfortunately, more recent evidence has demonstrated additional, more serious harms associated with SCSS use. These additional conditions are important to weigh when considering prescribing SCSS to patients in UC.
Infection
It has long been appreciated that the potent anti-inflammatory effects of steroids come at the expense of immunosuppression. Unsurprisingly, therefore, both adult and pediatric patients prescribed SCSS are at increased risk of sepsis for up to 3 months. The degree of risk of sepsis is a 2-to-5-fold increase in adults and a nearly two-fold increase in children with the risks being highest in the 30-days of after SCSS.6,7,8
Additionally, it has been shown that children are at an increased risk of pneumonia for up to 3 months following SCSS. There is a greater than a two-fold risk that a child will develop pneumonia in the month after a steroid burst, and the risk does not return to baseline until 90 days after receiving the prescription.7
Cardiovascular
A patient is roughly 250% more likely to develop congestive heart failure within the first month after a SCSS. This relative risk is significant for those with and without a previous history of cardiovascular disease or significant comorbidity, respectively, and does not return to baseline for up to 3 months.6,1 Similarly, patients given SCSS are at a >300% increased risk of deep vein thrombosis in the several months after taking steroids.8
Musculoskeletal
Chronic steroid use is associated with osteoporosis and its complications (eg, vertebral compression fractures). However, more recent evidence has shown that even SCSS increases susceptibility to a variety of fractures. Adults are nearly twice as likely to be diagnosed with a fracture in the month following SCSS with the risk attenuating over the subsequent 60 days.8 Similarly, SCSS can also increase the risk of avascular necrosis (AVN). While usually associated with longer term or repeated steroid use, there are case reports of AVN occurring even with single short courses of steroids.15,27,28
Gastrointestinal
The risk of gastrointestinal (GI) bleeding is significantly increased in both adults and children for the 3 months following SCSS. In adult patients, the risk of GI hemorrhage is nearly twice baseline, and the risk in children is increased approximately 1.5 times with the greatest risk being in the 30 days following SCSS.6,7
Discussion
Since shortly after the development of cortisone, the first corticosteroid used therapeutically in 1948, it has been evident that there are significant risks to long-term steroid use.29 However, for many decades the risks of SCSS were felt to be minor and short-lived. Increasingly, over recent years, larger studies in patients of all ages have revealed rare but significant increased risk of serious harms for even short-term corticosteroid therapy, which continue for months after completing the therapies.6,7,8 Importantly, the risks of the adverse events apply to both the straightforward healthy patient with bronchitis and frail patient with multiple medical comorbidities, meaning they might be viewed in the context of our entire patient population rather than a high-risk subset.1
SCSS are effective for a number of conditions commonly seen in UC as discussed above (eg, croup, asthma, radicular low back pain). However, they are similarly commonly utilized for many related UC presentations without evidence to support their benefit (eg, sinusitis, bronchitis, and non-radicular low back pain). This indication creep is understandable and comes from a place of clinicians wanting to offer something helpful for patients seeking treatment. Yet, in situations where the evidence for benefit is minimal, murky, or absent, we are encouraged to prioritize the foundational principle of medicine: “First, do no harm.”
Given the episodic nature of our patient-provider relationships, it is unlikely that a UC clinician would gain relevant clinical experience from these rare downstream adverse events in the weeks or months following our initial encounter to inform our practice patterns. Patients likewise are unlikely to recognize that a fracture, blood clot, or hospitalization for sepsis 1 to 3 months after a steroid burst, may be related. This is why it is so important to foster a culture of systemic steroid stewardship in the UC: so that we can apply this recent evidence to limit our SCSS use to situations where benefit is likely and educate our patients about the potential hazards so that they may be similarly judicious about seeking and taking systemic steroids in the future.
Conclusion
Changing engrained practice patterns and patient expectations is a difficult but worthwhile endeavor if the aim is to improve the quality of care we deliver. Fostering a culture of systemic steroid stewardship will allow us to deliver effective, compassionate, evidence-based care to the patients we serve.
Manuscript submitted September 9, 2023; accepted November 7, 2023.
References
- Wallace BI, Waljee AK. Burst Case Scenario: Why Shorter May Not Be Any Better When It Comes to Corticosteroids. Ann Intern Med. 2020 Sep 1;173(5):390-391. doi: 10.7326/M20-4234. Epub 2020 Jul 7. PMID: 32628530.
- Riggs KR, Ubel PA. The role of professional societies in limiting indication creep. J Gen Intern Med. 2015 Feb;30(2):249-52. doi: 10.1007/s11606-014-2980-0. Epub 2014 Aug 5. PMID: 25092014; PMCID: PMC4314486.
- Morley, V.J., Firgens, E.P.C., Vanderbilt, R.R. et al. Factors associated with antibiotic prescribing for acute bronchitis at a university health center. BMC Infect Dis 20, 177 (2020). Doi: 10.1186/s12879-020-4825-2
- Chow A, et al. File, Executive Summary: IDSA Clinical Practice Guideline for Acute Bacterial Rhinosinusitis in Children and Adults, Clinical Infectious Diseases, Volume 54, Issue 8, 15 April 2012, Pages 1041–1045, doi:10.1093/cid/cir1043
- Truitt KN, Brown T, Lee JY, Linder JA. Appropriateness of Antibiotic Prescribing for Acute Sinusitis in Primary Care: A Cross-sectional Study. Clin Infect Dis. 2021 Jan 27;72(2):311-314. doi: 10.1093/cid/ciaa736. PMID: 33501972; PMCID: PMC7840109.
- Yao TC, Huang YW, Chang SM, Tsai SY, Wu AC, Tsai HJ. Association Between Oral Corticosteroid Bursts and Severe Adverse Events : A Nationwide Population-Based Cohort Study. Ann Intern Med. 2020;173(5):325-330. doi:10.7326/M20-0432
- Yao T, Wang J, Chang S, et al. Association of Oral Corticosteroid Bursts With Severe Adverse Events in Children. JAMA Pediatr. 2021;175(7):723–729. doi:10.1001/jamapediatrics.2021.0433
- Waljee A K, Rogers M A M, Lin P, Singal A G, Stein J D, Marks R M, et al. Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study BMJ 2017;357:j1415 doi:10.1136/bmj.j1415
- College of Urgent Care Medicine Position Statement: Corticosteroid Stewardship. Published 2022 Aug 18. Accessed Nov. 4, 2023.
- Lin KJ, Dvorin E, Kesselheim AS. Prescribing systemic steroids for acute respiratory tract infections in United States outpatient settings: A nationwide population-based cohort study. PLoS Med. 2020 Mar 31;17(3):e1003058. doi: 10.1371/journal.pmed.1003058.
- Bénard-Laribière A, Pariente A, Pambrun E, Bégaud B, Fardet L, Noize P. Prevalence and prescription patterns of oral glucocorticoids in adults: a retrospective cross-sectional and cohort analysis in France. BMJ Open. 2017;7(7):e015905. Published 2017 Jul 31. doi:10.1136/bmjopen-2017-015905
- RECOVERY Collaborative Group, et al. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021 Feb 25;384(8):693-704. doi: 10.1056/NEJMoa2021436. Epub 2020 Jul 17.
- Bradley MC, Perez-Vilar S, Chillarige Y, et al. Systemic Corticosteroid Use for COVID-19 in US Outpatient Settings From April 2020 to August 2021. JAMA. 2022;327(20):2015–2018. doi:10.1001/jama.2022.4877
- Centers for Disease Control and Prevention. Updated Information on Availability and Use of Treatments for Outpatients with Mild to Moderate COVID-19 Who are at Increased Risk for Severe Outcomes of Covid-19. CDCHAN-00463. Accessed September 5, 2023.
- Dvorin EL, Ebell MH. Short-Term Systemic Corticosteroids: Appropriate Use in Primary Care. Am Fam Physician. 2020;101(2):89-94.
- Usatine RP, Riojas M. Diagnosis and management of contact dermatitis. Am Fam Physician. 2010 Aug 1;82(3):249-55. PMID: 20672788.
- Smith DK, McDermott AJ, Sullivan JF. Croup: Diagnosis and Management. Am Fam Physician. 2018 May 1;97(9):575-580. PMID: 29763253.
- Kim C, Kabbani S, Dube WC, Neuhauser M, Tsay S, Hersh A, Marcelin JR, Hicks LA. Health Equity and Antibiotic Prescribing in the United States: A Systematic Scoping Review. Open Forum Infect Dis. 2023 Aug 19;10(9):ofad440. doi: 10.1093/ofid/ofad440. PMID: 37671088; PMCID: PMC10475752.
- Bizune D, Tsay S, Palms D, King L, Bartoces M, Link-Gelles R, Fleming-Dutra K, Hicks LA. Regional Variation in Outpatient Antibiotic Prescribing for Acute Respiratory Tract Infections in a Commercially Insured Population, United States, 2017. Open Forum Infect Dis. 2023 Feb 8;10(2):ofac584. doi: 10.1093/ofid/ofac584. PMID: 36776774; PMCID: PMC9905267.
- Szymczak JE, Linder JA. “Cultural” Variation in Antibiotic Prescribing: Have Regional Differences Had Their Day? Open Forum Infect Dis. 2023 Feb 8;10(2):ofad025. doi: 10.1093/ofid/ofad025. PMID: 36776775; PMCID: PMC9905358.
- Seidman MD, et al. Guideline Otolaryngology Development Group. AAO-HNSF. Clinical practice guideline: Allergic rhinitis. Otolaryngol Head Neck Surg. 2015 Feb;152(1 Suppl):S1-43. doi: 10.1177/0194599814561600. PMID: 25644617.
- Dykewicz MS, et al. Treatment of seasonal allergic rhinitis: An evidence-based focused 2017 guideline update. Ann Allergy Asthma Immunol. 2017 Dec;119(6):489-511.e41. doi: 10.1016/j.anai.2017.08.012. Epub 2017 Nov 2. PMID: 29103802.
- Qaseem A, et al. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017 Apr 4;166(7):514-530. doi: 10.7326/M16-2367. Epub 2017 Feb 14. PMID: 28192789.
- Haley SP, Stem LA. Corticosteroids for Low Back Pain. Am Fam Physician. 2023 Mar;107(3):Online. PMID: 36920810.
- Cashin AG, et al. Pharmacological treatments for low back pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2023 Apr 4;4(4):CD013815. doi: 10.1002/14651858.CD013815.pub2. PMID: 37014979; PMCID: PMC10072849.
- Prednisone. Package Insert. Hikma Pharmaceuticals, 2023.
- Kennedy P, Bassiouni A, Psaltis A, et al. Avascular necrosis after oral corticosteroids in otolaryngology: case report and review of the literature. Allergy Rhinol (Providence). 2016;7(1):e50-e54.
- Dilisio MF. Osteonecrosis following short-term, low-dose oral corticosteroids: a population-based study of 24 million patients. Orthopedics. 2014;37(7):e631-e636
- Benedek TG. History of the development of corticosteroid therapy. Clin Exp Rheumatol. 2011 Sep-Oct;29(5 Suppl 68):S-5-12. Epub 2011 Oct 21. PMID: 22018177.
Download the article PDF: Systemic Steroid Stewardship in Urgent Care: Recognizing Indication Creep to Limit Avoidable Harms
Read More

