Published on
Urgent message: “Dizziness” can prove to be one of the more vexing complaints encountered in urgent care. To provide appropriate care, the clinician must understand whether the patient is experiencing near-syncope, disequilibrium, ill-defined light-headedness, or vertigo.
Martin Samuels, MD, DSc (hon), FAAN, MACP
The problem of dizziness can be one of the most exasperating in the practice of medicine. Physicians all know that sinking feeling elicited by the patient who sits down and, when one asks “What can I do for you?”, says, “I’m dizzy.” The goal of this article is to offer urgent care practitioners a reasoned approach to dizziness that will lead expeditiously to diagnosis and effective therapy.
Principles of Diagnosis
The first principle in evaluat- ing a dizzy patient is to take an open-ended history.
This is a good rule in tak- ing any medical history, but it is particularly applicable in this instance. When the patient says to you, “I am diz- zy,” sit back in your chair, slowly spin around, perhaps stare aimlessly out the window, and reply, “What do you mean, dizzy?” Then wait for the response.
This may take what seems to be a long time; nonetheless, don’t probe further by asking “Does the room spin?” “Do your legs get weak?” “Do you feel as if you might stagger?” “Are you lightheaded?” because the answer to all these questions will nearly always be “yes.” If you are fortunate enough to be the first physician to examine a patient complaining of dizziness, always take the undirected approach and wait for the response. There are several possible responses.
Syncope or Near-Syncope
“I feel as if I might faint,” or “I feel giddy or light-headed.” Some patients do faint or report that they have done so while others have never actually fainted (near-syncope). Pathophysiologically, both syndromes suggest any of several cardiovascular disorders that produce a generalized decrease in cerebral blood flow. There is no qualitative difference between syncope and near-syncope with respect to the differential diagnosis. This topic was discussed in detail in the October 2006 issue of JUCM, and will not be explored further here.
Disequilibrium
“My balance is off and I feel as if I might fall.” This version of dizziness generally reflects one of two major categories of neurologic disease, apart from disorders of the vestibular system.
Cerebellar ataxia is due either to a primary disease of the cerebellum (e.g., cerebellar degeneration, tumor in or near the cerebellum, cerebellar infarct) or disorders of the tracts leading to (cerebellopetal) or from (cere- bellofugal) the cerebellum. Neurologic examination will ordinarily unveil such pathology by revealing axial (e.g., wide-based gait; falling to one side) or appendicular ataxia (e.g. side-to-side tremor on goal-directed action).
Multiple sensory deficits syndrome is due to several abnormalities in the various sensory proprioceptive systems. When a number of these systems fail, the central nervous system receives conflicting proprioceptive input, with consequent dizziness. Typically, such a patient complains of dizziness at night for instance, when the lights are out or dim and he or she has to go to the bathroom. On occasion, the patient may fall, particularly in environments in which there are no reliable visual cues (e.g., the shower).
The treatment of this extremely common syndrome is common sense (as many of the sensory abnormalities that can be corrected should be); such patients should not be treated with drugs that might sedate them, as antivertigo medications would do. Mistaking this syndrome for vertigo would, in fact, make matters worse.
Anxiety and/or Depression
There are patients who when asked, “What do you mean, dizzy?” respond, usually after a pause, “Dizzy.” If the physician persists with “Do you mean you might faint?” or “Do you mean that you might fall?” or “Do you mean that the room spins?” the patient repeats, “No, I mean I’m dizzy.”
This disorder can only be called true dizziness, and it generally arises from various psychological disorders, most commonly anxiety (with or without hyperventilation) and/or depression.
Vertigo
The fourth and last category of disorder found in patients who complain of dizziness is true vertigo (an illusion or hallucination of motion). Some patients insist that they themselves are moving, while others such as the one presented above have the sense that the environment is moving. In either case, these patients transmit the message that they feel as if they are tilting, rocking, falling, spinning, or moving in some fashion.
Vertigo indicates a disturbance in the vestibular system. The important clinical question is whether the vertigo is due to a disorder in the peripheral nervous system or in the central nervous system, for central and peripheral etiologies each have their own differential diagnosis and treatment.
Evaluation of Vertigo
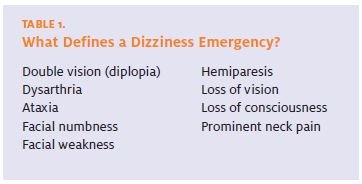
The first step is to perform a complete history and physical examination, as well as a neurological examination with particular attention to the VIII cranial nerve. (Symptoms that may reflect a true dizziness emergency are listed in Table 1.)
Cochlear VIII Nerve Function
Pure Tone Hearing Loss
Test for pure tone hearing loss. This can be done in the office by assessing the sensitivity of the patient’s hearing or comparing the patient’s hearing with one’s own, using a ticking watch or the sound of fingers rubbing together. If there is hearing loss, the patient should be referred for additional audiologic testing to determine the specific type of hearing loss.
While hearing loss associated with vertigo can have a relatively benign prognosis such as with Ménière’s disease, vestibular schwannoma must be excluded as a cause since it requires urgent surgical intervention. This can be accomplished by MRI to image the VIII cranial nerve, or by audiogram to exclude retrocochlear hearing loss. (Alternatively, a skilled physician with a thorough understanding of the pathophysiology of the vestibular system may differentiate via a systematic approach to evaluating hearing loss; this is detailed online at www.jucm.com.)
Vestibular VIII Nerve Function
Testing for Nystagmus
The vestibular aspect of the VIII cranial nerve may be examined by testing for nystagmus. First, ask the patient to sit on the end of the examining table and to look about 45° to the right and to the left. (Asking the patient to look beyond 45° is not useful, since when asked to look too far in either direction, about 10% of the normal population show some degree of gaze-evoked endpoint nystagmus.) If nystagmus develops when the gaze is directed to 45°, note the direction of the fast phase, the direction of the slow phase, and in what position of the eyes they occur.
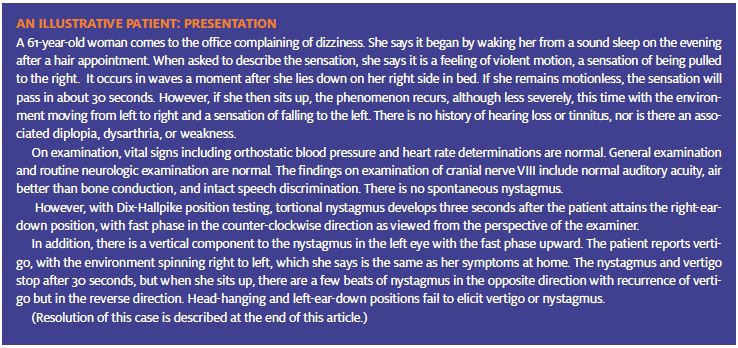
Next, the patient should be put through a series of positions called the Dix-Hallpike maneuver (Figure 1). All vertigo is positional to some extent, but there are specific pathogenetic and prognostic implications if vertigo is exclusively positional. Once position testing has been done, the physician knows in which direction the world seems to be spinning and in which direction the patient seems to be falling when the vertigo develops. The directions of the fast and slow phases of the nystagmus have been recorded. The next step is the interpretation of these data.
Peripheral or Central Nervous System?
A basic understanding of the neuroanatomy and neurophysiology of the vestibular system is necessary for effectively interpreting findings from the neurological exam. (A detailed review can be found online at www.jucm.com.)
Criteria for Locating the Lesion
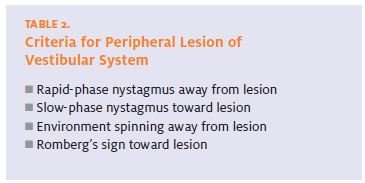
There are four criteria for a peripheral type of vertigo and nystagmus (see Table 2). If there are 1) fast-phase nystagmus away from the lesion,2) slow-phase nystagmus toward the lesion, 3) environment spinning away from the lesion, and 4) Romberg’s sign toward the lesion, one can say with confidence that there is a lesion of the peripheral nervous system, probably in either the end organ or the peripheral nerve. If any of these four rules fails to hold, one can assume by exclusion that the lesion is in the central nervous system.
Central nervous system lesions can cause bilateral nystagmus in the same position of the head, vertical nystagmus of any kind, and any conditions in which the directions of the fast and slow phases, the Romberg’s sign, and the spinning of the environment do not strictly fit the four criteria specified. Those criteria specify only the anatomic localization without implying anything about the severity or seriousness of the under- lying disease. Peripheral diseases can be self-limiting (e.g., vestibular neuronitis) or very serious (e.g., vestibular schwannoma). Central diseases can range from the trivial cmplications of many drugs (e.g. benzodi azepines) to vertebrobasilar insufficiency.
Synthesizing the Data
Thus, by testing the auditory system and the vestibular system, one can divide all cases of vertigo into three categories: 1) peripheral (by vestibular criteria) 2) peripheral (by vestibular criteria) disease with hearing loss (by auditory criteria), and 3) central disease. With this in mind, we can now consider the major diseases in each category.
Peripheral Cochlear Lesions
Labyrinthitis is thought to be a result of viral infection of the endolymph and perilymph, affecting both the vestibular and cochlear components of the system. The usual history is viral illness followed by acute onset of severe spinning vertigo and sensory neural deafness with tinnitus. Examination shows a classic peripheral picture by vestibular criteria and a classic cochlear picture by auditory criteria. Despite its severe onset, labyrinthitis is a benign illness that resolves completely in three to six weeks. Patients regain normal hearing and vestibular function.
Vestibular neuritis, or acute vestibulopathy, is thought to be pathogenetically identical to labyrinthitis but without any hearing symptomatology. If the patient has vertigo unaccompanied by a hearing abnormality, it is strictly speaking impossible to be sure whether the disease is cochlear or retrocochlear. However, its natural history is also benign, and it resolves completely in three to six weeks, which makes a retrocochlear illness very unlikely.
Cochlear neuritis is the syndrome of acute pure deafness without vestibular symptoms or signs. It is thought to be analogous to vestibular neuritis.
Ménière’s disease is caused by a cryptogenic hydrops of the endolymph such that there is intermittent swelling of the semicircular ducts, with damage to the hair cells.
Typically, an attack of Ménière’s disease is characterized by a dull ache in the region of the mastoid process or around the ear associated with severe tinnitus, a cochlear kind of sensory neural hearing loss, and a classic peripheral type of vestibular syndrome with severe spinning vertigo. It is identical in almost every respect to an acute attack of labyrinthitis. However, it does not resolve completely in three to six weeks, and patients are left with residual hearing loss. Several months or years later, a similar attack may occur, leaving the patient with even more severe hearing loss. Tinnitus, a nonspecific sign of auditory system disorder, is a major problem for these patients, who can be terribly disabled for weeks at a time by the vertigo that accompanies acute attacks.
Many therapies have been tried, including shunting of the perilymphatic system and diuretics, but none are curative. About 15% of these patients have bilateral disease in subsequent years. Management of such patients is complex and often best entrusted to an otolaryngologist or otoneurologist, as deliberate toxic (e.g., intraaural aminoglycoside antibiotics infusion) destruction or surgical severing of the vestibular nerve may be required.
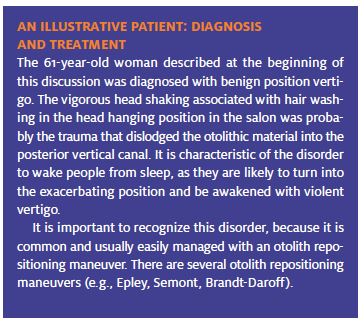
Benign positional vertigo, or Bárány’s vertigo, usually occurs in older patients and is characterized by the sudden onset of a peripheral vestibular syndrome with no auditory aspect. It is present only in certain positions, which are specific to the individual.
Typically, the patient reports that a few moments after attaining a certain position, perhaps in bed at night, severe vertigo occurs in which the world spins in one direction while the patient has a sensation of falling in the other direction.
If he or she does not move, the vertigo stops, which implies that it is transient in type. If the patient sits up, the vertigo recurs, but this time in reverse. If the patient repeats the posture several times, the tendency toward vertigo and nystagmus will fade.
All the symptoms can be reproduced using the Dix- Hallpike maneuver, during which the patients will experience vertigo with the affected ear down and an associated nystagmus that is rotatory in the dependent eye and vertical in the opposite eye. Benign positional vertigo has a benign natural history, which improves gradually over a six-month period and ends with complete recovery.
Peripheral Retrocochlear Syndromes
Vestibular Schwannoma
A second category of disease is a peripheral type of vertigo, characterized by retrocochlear hearing loss (i.e., patients are found to have poor speech discrimination). Such patients should have an image of the inner ear, preferable an MRI. If an MRI cannot be obtained (e.g., due to the presence of a pacemaker), a CT scan with thin cuts through the inner ear is also very useful.
It is important to recognize the presence of a tumor while it is still contained within the internal auditory meatus and thus easily surgically resectable. Any patient with a history of progressive hearing loss should at some time during the evaluation have a careful auditory examination, and if any retrocochlear characteristics are found, a brain image with careful views of the internal auditory meatus should be obtained.
If you are treating a dizzy patient with peripheral cochlear findings of hearing loss and there has been no improvement in three to six weeks, referral and/or imaging may be indicated.
Central Lesions
The last category of vertigo is central disease (i.e., patients with vestibular symptomatology that does not meet the criteria for peripheral disease). This group includes patients who exhibit vertical nystagmus or bilateral nystagmus when their head is in an identical position.
Drugs
All drugs that act by intoxicating the reticular activating system in the core of the brainstem including all anti-convulsants, all sedatives, and some sleeping pills— will by their nature produce nystagmus in two different directions in the same position of the head. When the patient looks to the right, the nystagmus beats to the right. When the patient looks to the left, it beats to the left. Overdosage can produce vertigo. Most sedatives (e.g., benzodiazepines) cause this type of nystagmus.
The fact that the lesion is central does not necessarily mean that it is serious. In fact, the appearance of this form of nystagmus may prove that a given drug (e.g. phenytoin) is in the therapeutic range. Such patients should be asked specifically about their use of drugs, including alcohol; before any invasive studies are per- formed, it is useful to order blood and urine toxic screening.
Demyelinating Illness
Demyelinating illnesses, such as multiple sclerosis, can and often do produce vertigo.
Vascular Disease Affecting the Brainstem In approaching vascular disease affecting the brain- stem, it should be remembered that the most common manifestation of vertebrobasilar insufficiency is vertigo, but vertigo is almost never the only manifestation.
Such patients can also be expected to complain of double vision, weakness of the limbs, sensory loss, dysarthria, and dysphagia. It might be possible for dis- ease of the small branch of the vertebral artery to produce vertigo as its only symptom, but in such instances there is no specific or emergency therapy anyway. This presentation may also be seen in the same type of patient who presents with multiple sensory deficit syndrome. Referral may be indicated.
Disorders of the Temporal Lobe
Temporal lobe seizures arising from trauma, tumors, or prior strokes can, as one of their manifestations, produce vertigo. Vertigo is rarely the only symptom of a temporal lobe seizure, however, and such a diagnostic consideration requires neurologic consultation.
Migraine
Migraine is strongly associated with vertigo. About 10% of patients with vertigo will, ultimately, be found to have migrainous vertigo. The reverse association is even more common. The majority of migraineurs have a his- tory of motion sickness, which is physiological vertigo, and some patients have vertigo as the only aura of migraine. Episodes of vertigo lasting about 20 minutes, with or without associated headache, should raise this possibility. Often, a therapeutic trial with anti-migraine medication is required to make this diagnosis.
Treatment of Vertigo
Antiserotonin and Antihistamine-type
There are three categories of drugs for treating true ver- tigo: anticholinergic and antihistamine-type drugs, and the phenothiazine agent promethazine.
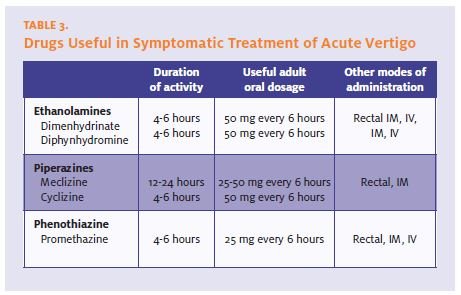
Anticholinergic and antihistaminetype drugs include dimenhydrinate, diphenhydramine, meclizine, and cyclizine. All of these drugs are effective if the dosage is adequate—about 50 mg every six hours (see Table 3). They can produce major sedation at higher doses or in susceptible patients such as the elderly or those on multiple medications, but this is often of no concern.
Promethazine is the only phenothiazine that works against the nausea associated with vestibular imbalance and vertigo. Other phenothiazines, useful for chemical nausea, are of no help whatsoever in this setting. Promethazine may be effective primarily because it is an anticholinergic, not because it is a phenothiazine. It is useful also because it can be given together with the anti- cholinergic drugs and may be adminis- tered by a non-oral (e.g., rectal) route. A combination of promethazine and anti- histamine is particularly effective for acute vertigo.
Summary
To evaluate dizziness, one must first decide whether it can be categorized as near-syncope, disequilibrium, ill- defined light-headedness, or vertigo. If it is vertigo, vestibular and auditory testing will allow one to place the patient into one of three categories: peripheral dis- ease, peripheral disease with hearing loss, or central disease. When this distinction is made, one can create a reasonable differential diagnosis and arrive at the likely diagnosis. Some of these disorders (e.g., vestibular schwannoma) require specific evaluation and treat- ment, whereas others have a benign natural history and require only symptomatic relief for the duration. Symptomatic therapy of vertigo is straightforward and makes use of the three categories of drugs discussed.
Selected Reading
- Drachman DA, Hart CW. An approach to the dizzy patient. Neurol- ogy. 1972;22:323.
- Roydhouse N. Vertigo and its treatment. Drugs. 1974;7:297. Schuknecht H. Cupulolithiasis. Arch Otolaryngol. 1969;90:765. Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999;341:1590-1596.
- Epley JM. New dimensions of benign paroxysmal positional ver- tigo. Otolaryngol Head Neck Surg. 1980;88:599-605.
- Dieterich M, Brandt T. Episodic vertigo related to migraine (90 cases): Vestibular migraine? J Neurol. 1999;246:883-892.
- Tinetti ME, Williams CS, Gill TM. Dizziness among older adults: A possible geriatric syndrome. Ann Intern Med. 2000;132:337-344. Waterston J. Chronic migrainous vertigo. J Clin Neurosci. 2004;11:384-388.
- Baloh RW. Vestibular neuritis. N Engl J Med. 2003;348:1027-1032. Baloh RW. Dizziness. In: Manual of Neurologic Therapeutics, 7th edi- tion. Samuels MA, ed. Philadelphia: Lippincott Williams & Wilkins. 2004. pps. 65-75.