Urgent message: Nurse-initiated protocols (NIPs) have been found to be beneficial in emergency department settings. Nurse-initiated x-rays for ankle and foot injuries can reduce patients’ length of stay while improving staff satisfaction. Utilization of NIPs in an urgent care setting can bring positive benefits to patients, staff, and the organization.
Allison Usset Gilles, DNP, FNP-C, RN; Der Xiong, DNP, FNP-C, RN; and Jenny A. Prochnow, DNP, MBA, RN
INTRODUCTION
Background
Overcrowding and long wait times are prevalent in healthcare facilities across the United States. The relationship between wait times and patient satisfaction has been well studied and demonstrates that longer wait times lead to lower patient satisfaction scores.1 Further, overcrowding and long wait times correlate with decreased confidence in the healthcare provider (HCP), decreased perceived quality of care, increased patient mortality rates, increased treatment delays, and inadequate pain control.1,2
Nurse-initiated protocols (NIPs) that target certain presenting complaints are a possible workflow process improvement presented in the literature. These protocols can be useful when the provider is not available for immediate patient assessment. Often in emergency department settings, a patient will wait for hours before being assessed by a physician, whereas the use of NIPs allows nursing staff to initiate diagnostic testing during this time.2 Use of NIPs has been found to improve patient outcomes and decrease patient’s length of stay (LOS).2,3
Objective
There is a lack of research regarding NIPs in an urgent care setting, as most studies on NIPs in the literature were conducted in the ED. However, the leaders and staff at one Midwestern, suburban urgent care center have seen the negative impacts of long patient wait times and the need for NIPs in an urgent care setting. The purpose of this project was to examine the impact of the implementation and evaluation of NIPs in one UC setting. The following PICO (population, intervention, control, and outcomes) question was formulated to explore the use of NIPs in UC: “Can nurses in an ambulatory care setting (P), accurately use (O) nurse-initiated protocols (I) such as ankle and foot radiographic tests for orthopedic injuries as compared to current practice (C); increase nurse/provider satisfaction; and decrease patient LOS (O)?”
It was hypothesized that NIPs would be used accurately by the nursing staff and lead to a decrease in patient wait times and an increase in nurse and HCP satisfaction.
Review of Literature
Common themes regarding NIPs were discovered after examining evidence in the literature. These include wait times, patient satisfaction scores, staff satisfaction, and accuracy of NIPs.
NIPs can decrease the time patients wait for radiographic images. The implementation of nurse-initiated x-rays (NIXR) can reduce the time from triage assessment to x-ray and x-ray review by an HCP).3 NIXR can also reduce the patients’ LOS in a department (;;;; ).3-10
NIPs can also have a positive impact on patient and staff satisfaction. Patients and families had positive feedback about NIPs and indicated satisfaction, as well.9 Nurses in the literature review reported increased job satisfaction and an increased sense of autonomy and empowerment, and felt NIPs benefited their department (an, Eley, Hughes, & Sinnott, 2016;.3,9,11 All physicians surveyed were satisfied by having results available at the time of patient assessment.9
While NIXR is as accurate as radiographic tests ordered by providers, the literature concluded that NIXR decreased the number of x-rays ordered while maintaining or increasing the number of fractures detected).5,6,8,9 In addition, there was no statistical difference or fewer ankle fractures missed with NIXR6,8 in the context of the Ottawa Ankle Rules (OAR), a validated tool that has been deemed successful and useful in assessing patients who presented with a suspected foot or ankle fracture.8 This tool provides a functional assessment to determine if patients need radiographic imaging. It was created with the intention of detecting the problem quickly, minimizing unnecessary imaging, and shortening ED wait times and cost.12 In one study, the sensitivity of the OAR by nurses was 100%.13
Methods
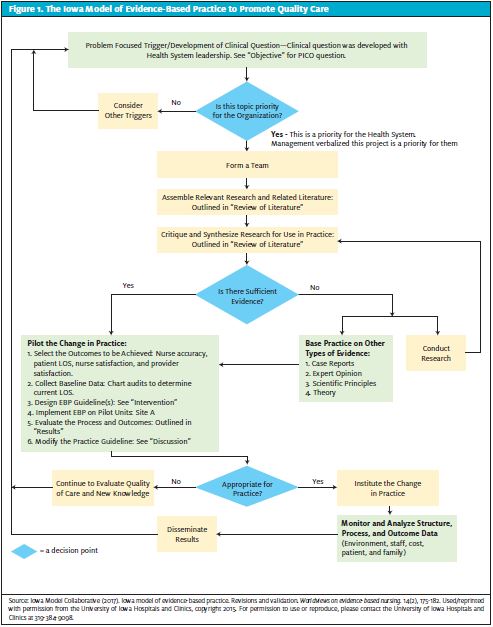
Evidence-based practice implementation model
The Iowa Model of Evidence-Based Practice to Promote Quality Care was used to guide the implementation process of this project (Figure 1). This model was selected due to the lack of high levels of evidence in the literature regarding this topic,. It can be used for practice changes based on research from lower levels of evidence.14
Setting and Sample
The setting for this project was a Midwestern suburban UC center. This UC center is a walk-in clinic that treats patients of all ages for non─life-threatening illnesses and injuries. The UC employs 14 full- or part-time registered nurses (RNs). Patients who come to UC are treated based on order of arrival and seriousness of their condition. Wait times vary and depend on how many other patients are waiting to be seen. Average LOS (check-in time to discharge) for patients in this UC in 2018 ranged from 78.67 minutes (May) to 106.28 minutes (January). In December 2018, UC saw between 63 and 118 patients per day and performed 27 ankle and 35 foot x-rays.
IMPLEMENTATION
Two NIPs were implemented at the UC in May 2019; the implementation period lasted 12 weeks. The two protocols, an NIXR for ankle injuries and an NIXR for foot injuries, were created based on the OAR.
The project started with 13 RNs being educated on how to use the protocols. All RNs were emailed the protocols, along with learning materials on how to use the protocols prior to an individual education session with the project leads. During the education session, the project leads would verbally describe the protocol, including patient inclusion and exclusion criteria. Project leads also used YouTube instructional videos, demonstrated the protocols on mannequins, and demonstrated on the RN. Lastly, the RN could practice on the project leads and mannequins and ask any clarifying questions.
Education was also provided on the required documentation, in the electronic health record (EHR), when using the protocols. RNs were shown how to document the patient’s verbal consent or right to refuse treatment in the nursing notes.
RNs were required to score 80% or higher on an eight-question post-test after the education session. An RN with less than 80% was walked through the test and protocol with the project leads until they achieved a score of 80% or higher.
OUTCOME MEASURES
The four outcomes evaluated were nurse accuracy in using the protocols, patient LOS, nurse satisfaction, and HCP satisfaction.
Nurse accuracy was determined by the nurse’s documentation in the EHR. The project leads examined the EHR for each patient who presented to UC with foot or ankle complaints. Project leads then looked at the RN’s documentation to determine if the assessment documented by the RN resulted in the correct outcome (no orders placed by nurse or radiographic imaging ordered) based on the protocol. A “missed opportunity” existed when a patient fit the ankle and foot protocol, but the RN did not document in the EHR why an x-ray was not ordered. Thus, “misses” were one element of the nurse accuracy outcome. Another aspect of the accuracy outcome was based on whether providers ordered any additional imaging. Providers could order radiographic tests for patients with normal OAR assessment findings or could order additional radiographic imaging in addition to the imaging ordered by the RN.
Patient’s LOS was determined by the EHR. The EHR incorporates a timestamp tab that determines when a patient checks into UC and when the provider prints their discharge paperwork.
Lastly, RN satisfaction and HCP satisfaction information were gathered from survey questions using a five-point Likert scale emailed to RNs and HCPs. Nurses were asked to consider the following statements in the survey:
- The education session for the nursing protocols prepared me to use them in practice
- The protocols were easy to follow
- I feel confident using the nurse-initiated protocols
- With the addition of the nurse-initiated protocols, I feel more impowered as a nurse in my practice
- I feel the protocols are beneficial to patients, families, and the organization
Statements HCPs were asked to respond to included:
- I believe the nurses followed the protocols accurately
- I think it is beneficial for nurses to order foot and ankle x-rays prior to my assessment
- The protocols save time for you and the patient/family
- The protocols are beneficial to patients, families, and the organization”
Table 1.Summary of Nurse Accuracy Data
| May | June | July | August | Total | |
| # of adult x-rays | 15 | 59 | 75 | 21 | 170 |
| # excluded due to protocol | 5 | 40 | 40 | 9 | 94 |
| # of missed opportunities | 4 | 14 | 22 | 10 | 50 |
| # of x-rays ordered by RN | 6 | 5 | 13 | 2 | 26 |
DATA ANALYSIS
To determine how accurately RNs can use NIPs (see Table 1), the number of missed opportunities to order an x-ray was considered, as was the number of RNs who did not follow the protocol. The LOS (in minutes) was also analyzed for all adult patients who received ankle or foot x-rays. A t-test assuming unequal variances determined whether patient LOS differed with statistical significance across the x-rays ordered by the RN vs the x-rays ordered by an HCP. Statistical significance was determined at the 0.05 level. RN and provider satisfaction were analyzed via the surveys. The process to create a data sheet was the same for the RN satisfaction survey as well as for the provider satisfaction survey.
RESULTS
Nurse Accuracy
There were 170 x-rays performed on patients seen for ankle and foot injuries from May to August 2019, during which time 94 patients with ankle or foot injuries were excluded based on the protocol criteria. Patients were excluded if they sustained the injury more than 7 days prior, if they had other physiological complaints other than the ankle or the foot, and if there was no bone tenderness in the malleolar zone or fifth metatarsal.
During the implementation period in May, there were 10 patients who met the inclusion criteria and RNs ordered six x-rays (60%). In June, RNs ordered five x-rays and 19 patients met the criteria (26%). In July, 35 patients met inclusion criteria and 13 x-rays were ordered by RNs (37%). During the implementation period in August, 12 patients fit the protocols and two x-rays were ordered by the RNs (16%).
Of the 26 x-rays ordered by nursing staff, two were positive for fractures. Of the 94 patients who were excluded due to the exclusion criteria, no x-rays were ordered by an RN. One x-ray was possibly ordered inappropriately by an RN (no documentation of the SMARTPHRASE or where the patient had bone tenderness). One additional x-ray was ordered by a provider on a patient who had imaging ordered by an RN.
Patients Length of Stay
The mean difference in patient LOS in urgent care between patients who had x-rays ordered by an RN vs an HCP was 21 minutes. The average patient LOS when an RN ordered imaging was 75 minutes, compared with an average patient LOS of 96 minutes when the x-ray is ordered by an HCP. Table 2 shows the mean LOS between patients who had imaging ordered by the RN vs an HCP. The conducted t-test gives statistical significance that the patient LOS differs across the two groups; it is 95% certain that patient LOS, on average, is anywhere from 3.9 to 38.8 minutes longer when the x-ray is ordered by a HCP rather than a RN [CI(3.9,38.8), p=.0172].
Table 2.Summary of Overall LOS (in Minutes) of Patients When Imaging Ordered by Provider vs RN
| Group | N | Mean | Mean Difference (MD – RN) | Lower CL Difference | Upper CL Difference | p – value |
| MD | 48 | 95.9 | ||||
| RN | 25 | 74.5 | ||||
| 21.4 | 3.9 | 38.8 | .0172* |
Nurse Satisfaction
Eleven of the 13 RNs completed the survey. Figure 2 displays the results from the RN satisfaction survey, which included responses from these statements:
- The education session for the nursing protocols prepared me to use them in practice.
- The protocols were easy to follow.
- I feel confident using the nurse-initiated protocols.
- With the addition of the nurse-initiated protocols, I feel more empowered as a nurse in my practice.
- I feel the protocols are beneficial to patients, families, and the organization.
Responses to question 1 show nine RNs agreed or strongly agreed that the educational session prepared them for use. Eight RNs agreed or strongly agreed that the protocols were easy to use and follow (Question 2). In question 3, seven RNs agreed or strongly agreed that they felt confident using the NIPs. In response to question 4, six RNs agreed or strongly agreed that with the addition of the NIPs, they felt more empowered as a nurse in their practice, though five RNs neither agreed nor disagreed. Eight RNs agreed or strongly agreed that the protocols are beneficial to patients, families, and the organization (question 5).
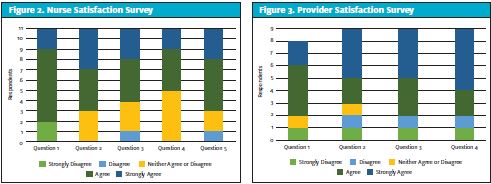
HCP Satisfaction
Eight out of 43 HCPs completed the provider satisfaction survey. The survey contained four questions based on a five-point Likert scale:
- I believe the nurses followed the protocols accurately.
- I think it is beneficial for nurses to order foot and ankle x-rays prior to my assessment.
- The protocols save time for you and the patient/family.
- The protocols are beneficial to patients, families, and the organization.
Figure 3 illustrates the responses to the provider satisfaction survey. In question 1, six HCPs agreed or strongly agreed the RNs followed the protocols accurately while one HCP strongly disagreed. Five HCPs agreed or strongly agreed that it is beneficial for RNs to order imaging prior to their assessment, while two strongly disagreed or disagreed (question 2). In question 3, six HCPs agreed or strongly agreed that the protocols saved time for them and the patient whereas two strongly disagreed or disagreed. Six HCPs agreed or strongly agreed that the protocols are beneficial to patients, families, and the organization (question 4).
Figure 3. Provider Satisfaction Survey
DISCUSSION
RNs can use NIPs accurately with proper education and training, as demonstrated by nurse accuracy data. There were 50 missed opportunities where RNs could have ordered an x-ray but did not; in other words, of the 170 patients, RNs missed 29.4% of patients. However, of the 170 patients, only one x-ray was ordered inappropriately, without clear documentation by the RN of whether the patient fit the protocol (0.006%). This is important because it shows, overall, RNs did not order x-rays when they shouldn’t. Although missed opportunities are important to document and show there could be improvement in this area, it is more important to discover that RNs aren’t ordering x-rays when they shouldn’t because this would expose the patient to unnecessary radiation.
The data analysis also demonstrated a positive impact on patients’ LOS in UC. Patients had a reduced LOS when an x-ray was ordered by an RN upon arrival to UC instead of those patients who had to wait for HCP assessment before getting the x-ray. This is a significant finding because organizations should be striving to decrease patient LOS.
Nurse satisfaction was overall positive, with most RNs feeling confident using the protocols. However, one RN strongly disagreed that they felt confident using the protocols. It is vital that every RN is comfortable and confident using the NIPs. A reassuring finding showed the implementation of the NIPs had a positive impact on the RNs sense of empowerment. Most of the RNs reported that NIPs brought benefits to patients, families, and the organization. Follow-up can be done with the RNs to build confidence and comfort levels in using NIPs, especially with additional opportunities to practice skills in using them.
The results of the provider satisfaction survey had primarily positive findings. Most of the HCPs reported that RNs used the protocols accurately, felt it was beneficial for RNs to order x-rays prior to their assessment, reported that the protocols save time for the patient/families, and felt the protocols are beneficial to patients, families, and the organization.
Limitations
One limitation of this pilot study was the lack of responses to the provider satisfaction survey. Only 18.6% of HCPs submitted survey responses. As a result, we cannot conclude the responses that were received reflect the beliefs of the providers overall. Project leads sent out a reminder email to RNs to complete the survey but did not send the reminder email to HCPs, which may have been beneficial to get more responses and, therefore more accurate HCP perception.
Another limitation of this study was the timing and location of the project. During this time, other workflow process improvement changes were taking place in this setting. Because this change took place at the same time as the implementation of NIPs, many RNs expressed that other important changes took precedence over using the NIPs. And since the project was implemented at only one clinic, it is not clear whether NIPs would be successful in other UC settings.
In addition, at present relatively few urgent care centers utilize RNs in the evaluation and treatment plan of incoming patients. As such, the generalizability of these results is unclear.
Lastly, patient LOS in UC can be impacted by many different factors such as short staffing, provider experience, patient volume in UC that day, and number of patients with high acuity that day. Those variables were not factored into the patient LOS stay results and therefore the results could be impacted.
CONCLUSION
NIPs are commonly used in EDs but have not been utilized in UC settings. All studies involving NIPs have been done in the ED and the benefits of NIPs are well established in the literature. However, UC settings are now becoming the new mainstream site for patients seeking quick medical treatment. Patient volumes in UC are increasing due to decreased cost compared with the ED, and the desire for rapid care and treatment. In addition, UC settings are transforming themselves to perform more functions than ever before, such as providing primary care access, same-day appointments, high-quality services, and convenient care.15
The goal of this project was to implement NIPs in an urgent care setting. Overall, the results of this study were positive. However, the sustainability of the ankle and foot NIPs depends on RNs’ confidence and initiated effort in using it. For this reason, we suggest that more time and exposure of the NIPs are needed before full benefits of the project are realized and for sustainability of the project. Further feedback from all staff about the NIPs and discussions on how to improve them is crucial before the protocol is implemented at other UCs. Further studies on the impact of NIPs especially NIXR for ankle and foot injuries are encouraged in other UC settings.
- Bleustein C, Rothschild DB, Valen A, et al. Wait times, patient satisfaction scores, and the perception of care. Am J Manag Care. 2014;20(5):393-400.
- Castner J, Grinslade S, Guay J, et al. Registered nurse scope of practice and ed complaint-specific protocols. J Emerg Nurs. 2013;39(5):467-473.
- Douma MJ, Drake CA, Odochartaigh D, Smith KE. A pragmatic randomized evaluation of a nurse-initiated protocol to improve timeliness of care in an urban emergency department. Ann Emerg Med. 2016;68(5):546-552.
- Curr S, Xyrichis A. Does nurse-led initiation of Ottawa Ankle Rules reduce ED length of stay? Int Emerg Nurs. 2015;23(4):317-322.
- Ho JK, Chau JP, Chan JT, Yau CH. Nurse-initiated radiographic-test protocol for ankle injuries: A randomized controlled trial. Int Emerg Nurs. 2018;41:1-6.
- Ho JK-M, Chau JP-C, Cheung NM-C. Effectiveness of emergency nurses’ use of the Ottawa Ankle Rules to initiate radiographic tests on improving healthcare outcomes for patients with ankle injuries: a systematic review. Int J Nurs Stud. 2016;63:37-47.
- Youwei L, Qunfnd L, Hua D, et al. The impact of triage nurse-ordered diagnostic studies on pediatric emergency department length of stay. Indian J Pediatr. 2018;85(10):849-854.
- Lee WW, Filiatrault L, Abu-Laban RB, et al. Effect of triage nurse-initiated radiography using the Ottawa Ankle Rules on emergency department length of stay at a tertiary centre. Canadian Journal of Emergency Medicine. 2015;18(2):90-97. doi:10.1017/cem.2015.67
- Robinson DJ. An integrative review: Triage protocols and the effect on ed length of stay. CJEM. 2013;39(4):398-408.
- 10. Rowe BH, Villa-Roel C, Guo X, et al. The role of triage nurse ordering on mitigating overcrowding in emergency departments: A systematic review. Acad Emerg Med. 2011;18(12):1349-1357.
- Cabilan CJ, Eley R, Hughes JA, Sinnott M. Medication knowledge and willingness to nurse-initiate medications in an emergency department: a mixed-methods study. J Adv Nurs. 2015;72(2):396-408.
- Stiell IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of radiography in acute ankle injuries. JAMA. 1993;269(9):1127-1132.
- Maclellan J, Smith T, Baserman J, Dowling S. Accuracy of the Ottawa Ankle Rules applied by non-physician providers in a pediatric emergency department. CJEM. 2017;20(5):746-752.
- Melnyk BM, Fineout-Overholt E. Evidence-Based Practice in Nursing & Healthcare: A Guide to Best Practice. Philadelphia: Wolters Kluwer; 2019.
- Ayers A. Urgent care 2.0: health systems taking the retail approach to the next level. J Urgent Care Med. September 9, 2018. Available at: https://www.jucm.com/urgent-care-2-0-health-systems-taking-retail-approach-next-level/. Accessed March 2019.
Acknowledgements: The authors thank the Winona State University Statistical Consulting Center, specifically Silas Bergen, PhD (Associate professor of statistics and director of Statistical Consulting Center at Winona State University) and Mikolaj Wieczorek (Winona State University Student) for their assistance and contribution to the data analysis. Allison Usset Gilles, DNP, FNP-C, RN is a Nurse Practitioner at Allina Urgent Care. Der Xiong, DNP, FNP-C, RN is aNurse Practitioner at CVS Pharmacy. Jenny A, Prochnow, DNP, MBA, RN is an Associate Professor, Winona State University. The authors have no relevant financial relationships with any commercial interests.

