Alan A. Ayers, MBA, Macc
Urgent Message: Urgent care is a consumer-driven phenomenon, and physician entrepreneurs continue to evolve the delivery of urgent care services in response to changing consumer preferences, both inside and beyond the brick-and-mortar facility.
Citation: Ayers A. Thinking outside the box to bring urgent care to the patient. J Urgent Care Med. 2024;18(4): 31-33.
While unregulated by most states, the term “urgent care” historically has come to mean a base offering of extended hours, on-site x-ray and lab, IV hydration, EKG, and procedures including laceration repair at a brick-and-mortar location. These standards are derived from the national Urgent Care Association Certification Criteria.1
However, from a patient standpoint, “urgent care” is more commonly taken to mean an acuity of symptoms (ie, non-emergent cuts, fractures, fever), visit priority (walk-in or same day), or services offered (rapid lab testing, x-ray, minor procedures). This definition expands the use of urgent care beyond traditional delivery models. After all, from a clinical standpoint, diagnoses of otitis media, allergic rhinitis, or streptococcal pharyngitis are the same regardless of venue.
Alas, healthcare entrepreneurs continue to reinvent the urgent care model in response to patient demand. One such model is Mobile Med, founded in Columbus, Ohio, in April 2019 by Gregory LaFontaine, PA, and Ryan Cantzler, MD, who I recently interviewed for this Practice Management exclusive in The Journal of Urgent Care Medicine.
Ayers: Mobile Med has a unique business model. Can you describe the services you offer?
LaFontaine: Mobile Med was started as an in-home option for patients to receive the same care and services they’d expect at an urgent care. We can treat anything normally seen at an urgent care, including suturing and draining abscesses. Using telehealth, we can even triage their concerns before a visit and advise if they should be seen at an emergency department. We give patients the option to see us through a house call or virtual appointment.
We have also added Dr. Bethany Recker, a board-certified family practice physician, so we now offer primary care services through a monthly membership program.
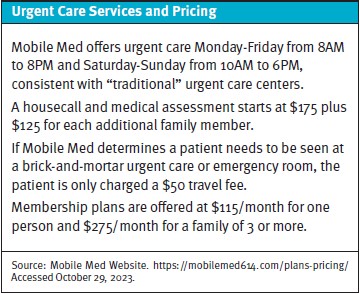
Mobile Med is a direct-pay service, and we do not contract with insurance companies. Although patients pay out-of-pocket for our services, we are priced competitively to what they’d pay at an urgent care after co-pays, deductibles, and other fees. Patients can use funds from health savings accounts, which they have found to be a beneficial way to use these accounts.
Ayers: How do you handle x-rays, lab testing and prescriptions?
LaFontaine: Currently, after evaluating a patient, we order imaging at a local outpatient imaging center or give recommendations on the next steps. We can order lab work or obtain blood and urine samples and send them directly to an outpatient lab. We send our prescriptions electronically using mobile electronic health records.
Patients can use their insurance at testing centers or outpatient labs, but we’ve found that many of these places can offer a reasonable and competitive rate for patients who pay directly.
Ayers: What is your clinical background and what led you to start Mobile Med?
LaFontaine: I have been practicing as a physician assistant for nearly 15 years in emergency departments and urgent cares throughout central Ohio. I also served in the United States Navy as a medical corpsman.
My co-founder, Dr. Ryan Cantzler, is a board-certified emergency medicine physician and has been practicing for 18 years in Columbus. Our newest partner, Dr. Bethany Recker, is a board-certified family practice physician with 19 years of experience. She completed her residency in Columbus and has been practicing here ever since.
Ryan and I came up with the idea for Mobile Med during a happy hour. We were both frustrated that many of the problems we were treating patients for in the clinical setting didn’t need to be seen at a brick-and-mortar healthcare facility. Patients shouldn’t have to be exposed to additional diseases or spend excessive time waiting in a lobby for care. A mother shouldn’t have to take all three of her kids to an urgent care before dinner because that’s the only time she can get one child treated for an ear infection.
Plus, as providers, we get to spend more time talking with patients and explaining what’s happening instead of rushing to get to the next bed.
Ayers: What gaps in care does Mobile Med address? Why do patients choose Mobile Med over other options?
LaFontaine: Mobile Med is healthcare that is centered on the patient. It’s convenient for the patient because we travel to them, thereby cutting out travel time and time spent sitting in a waiting room. We also spend more time with each patient, ensuring we get a thorough history. This also gives the patient time to ask questions and make sure they understand the treatment plan.
We’ve found that the first-time patients choose Mobile Med it’s often for convenience; however, they return because they’re able to be seen and treated quickly and are impressed by the level of service they receive.
Ayers: How did the COVID-19 pandemic accelerate your business model?
LaFontaine: In previous generations, doctors made house calls. Around the time of the pandemic, more and more businesses began to deliver goods and services to your door, however, healthcare was not one of them. Mobile Med changed that. During the pandemic, we became popular for COVID testing, especially before at-home testing was readily available through government-supplied test kits. Patients appreciated our flexibility to come to their residence. Often, we did the tests outside a patient’s home on the front porch or in the garage to accommodate social distancing. The pandemic also really solidified telehealth as an appropriate and accepted option for some health concerns.
Ayers: What is your revenue model? Do you bill insurance?
LaFontaine: Mobile Med is a direct-pay or fee-for-service provider. We do not contract with health insurance companies. However, we do accept HSA cards/funds and patients can use their insurance for reference lab work and other types of testing. Mobile Med also generates recurring revenue from members who pay monthly dues, with discounts for pre-paying for the quarter, semi-annually, or annually.
Ayers: How do you use technology to facilitate your business model?
LaFontaine: As a mobile-based business, we use technology in many ways. We use a HIPAA-compliant app to communicate with patients—including video and text/chat features. Patients really appreciate these options to send us questions, concerns, or even photos if we need to visually monitor their condition.
We’re in the process of developing our own app that will combine some of the technologies we’re currently using over several platforms (EMRs, telehealth, chat/text with providers, billing, plus more). We’re also testing new ways to treat patients, like using a mobile ultrasound to diagnose fractures, start IVs, evaluate gallbladders, etc.
Ayers: A trend we’re seeing in all urgent care is the convergence of urgent and primary care. Your model includes both. How do you define “primary care” and how is primary care synergistic to urgent care in your model?
LaFontaine: We started as an urgent care and found that many ailments we were seeing could be easily managed by a primary care provider (PCP). Also, patients were using urgent cares because they couldn’t get an appointment with their PCP—and many aren’t even established with a PCP. Continuity of care is so important, and Mobile Med supports that blending of urgent and primary care. Patients who have used us for urgent care have enjoyed our service so much that they’ve joined as primary care members with Dr. Recker. This provides personalized care for the whole patient.
Primary care is the ongoing care of your day-to-day health, including maintenance of chronic conditions and medication management. Urgent care should be used when you cannot wait to see your primary care provider or don’t have life-threatening symptoms that need to be treated in an emergency department. If patients are going to an urgent care frequently, they’d likely benefit from consistent care with a primary care provider who can address their issues.
Ayers: One of the criticisms of mobile urgent care services is that it’s less efficient than brick-and-mortar in that a clinic provider can see more patients per hour going from exam room to exam room than from house to house. How do you overcome this challenge and drive efficiencies in your business?
LaFontaine: We’re not an efficiency model —we’re a patient-driven model. We gain cost advantages by using a lean staff, technology, and the fact that we don’t staff a brick-and-mortar urgent care clinic. The providers do a lot of things themselves instead of using support staff (taking vitals, sending prescriptions, sending referrals, doing paperwork for sports physicals, etc.). Because we don’t contract with insurance, we also have less paperwork and billing needs than other practices or clinics.
Ayers: How do you see your business growing and evolving in the future?
LaFontaine: Our business model is constantly evolving. For example, we’ve already added services based on patient needs, like hormone replacement therapies, medical weight loss, and medical marijuana. We’re adding innovative aesthetic treatments that will give patients new options for that type of care. We’re meeting our patients where they want new or specialized care.
We are also constantly looking to technology and new ways to run our practice. We’ve seen patients respond positively to the technology they are already using in their everyday lives, so it makes sense for Mobile Med to use it, too. We’re definitely reexamining healthcare business models to find ways to make our business patient-centered, not just about profitability.
Ayers: Is there anything else our readers should know?
LaFontaine: As providers, we’ve had much more satisfaction in our jobs by spending more time with our patients. We feel like we’re truly helping them instead of just “treating and street-ing” them. Often our patients don’t actually need an appointment with us. We can text them to answer questions about their treatment plan and reassure them that they’re doing the right things and recovering in the right timeframe. And instead of being affiliated with large healthcare groups or hospitals, we’re making decisions that best fit our practice and patients. Spending time with our patients and improving their lives—isn’t this why we all went into medicine in the first place?
Conclusion
Urgent care was born of physician-entrepreneurs who saw an opportunity to meet patients’ episodic medical needs without the hassle and costs of emergency rooms or waiting for a primary care appointment. Urgent care grew as consumers loved the convenience and access of an on-demand, extended hours facility near where they work and play. Now that patients have acclimated to urgent care services, entrepreneurs continue to evolve the model in response to changing patient needs and preferences.
References
- Urgent Care Association Website. Certification Criteria. https://urgentcareassociation.org/quality/certification. Accessed November 30, 2023.
Click Here to download the PDF

