Urgent message: Expanding into occupational medicine requires a long-term commitment and willingness to respond to employer and employee needs.
ALAN A. AYERS, MBA, MAcc, Experity
Urgent care providers have conventionally defined their offering as “treatment of acutely rising episodic medical conditions.” However, widespread acceptance of the urgent care business model-retail-facing locations, extended hours, and walk-in service—has led many urgent care centers to expand into longitudinal primary care as well as occupational medicine. Specifically, when people don’t know where to go for a work-related injury, they’ll go to the same urgent care center that treats their family. In addition, as businesses move from decaying urban centers to freeway-accessible business parks, employers seek convenient providers for employee physicals and screenings.
Urgent care centers that have never held themselves out as providing occupational medicine are seeing these patients and employers just show up. And for an urgent care provider who has not offered occupational medicine in the past, the prospect of serving these new constituents can be daunting. The purpose of this article is to describe the landscape for occupational medicine, including the services constituting “occ med,” how workers’ compensation care is directed by employers and payors, and the process for treating and billing for workplace injuries.
Occupational Medicine Services
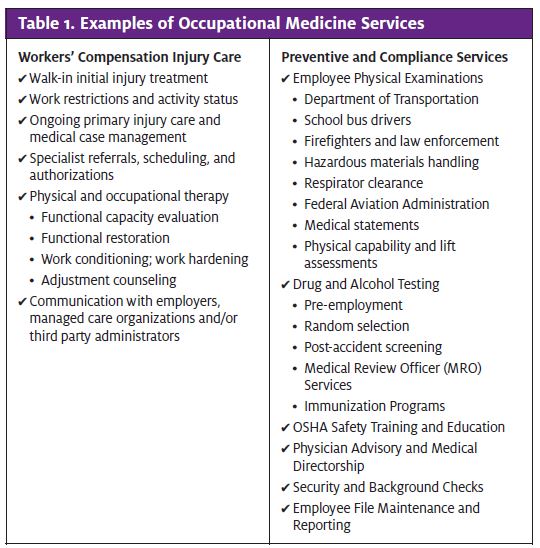
To begin, occupational medicine encompasses a wide range of services that at their most basic level can be delineated as “comp” (meaning workers’ compensation injury care) and “non-comp” (meaning employer services focused on compliance or prevention—primarily physicals and drug screens). Examples of each are listed in Table 1. Typically workplace injuries drive the bulk of revenues and profits for occmed providers, whereas commodity physicals and drug screenings are offered to solidify employer relationships, with the expectation they’ll direct injuries as they occur. A third component—health and wellness—is emerging as occ med shifts from a focus on “workplace injury prevention and treatment” to “total employee well being,” which encompasses early detection through biometric screenings, medical intervention for high-risk factors (i.e. tobacco use), and also exercise and nutrition programs.
Categories of Employers
Whereas urgent care is marketed to the general public—patients who self-pay or use government or private health insurance—occupational medicine is sold to employers who carry workers’ compensation insurance and pay directly for preventive and compliance services. Moreover, whereas urgent care patients typically self-triage, choosing urgent care because of its convenience or accessibility, employees who need occ med services are directed by their employers to the providers who offer the greatest value, outcomes, or communication to the employer.
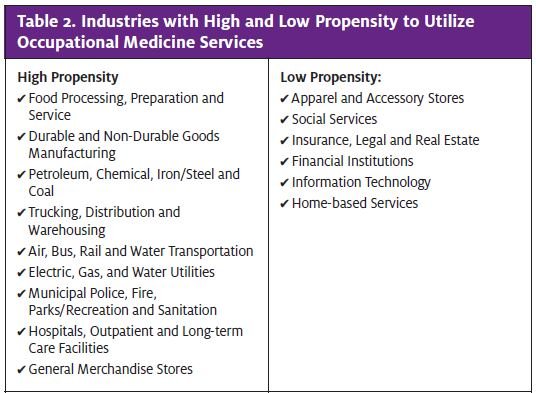
Employers can be segmented by their propensity to utilize occ med as well as their size and decision-making structure. Clearly some businesses have a greater need for occ med than others because they operate in industries that incur a greater risk of injury. For example, statistics show oil rig “roughnecks” get hurt more often and incur higher-acuity injuries than bank tellers. Likewise, some industries have greater compliance needs—a sanitation worker, for instance, may be required to have a commercial driver’s license, liability insurance that requires regular sub- stance abuse testing, vaccinations such as for Hepatitis A and B, and also be able to lift over 70 lb using proper techniques. These are all job requirements that entail occ med services. Table 2 lists industries that have a high and low propensity to utilize occ med.
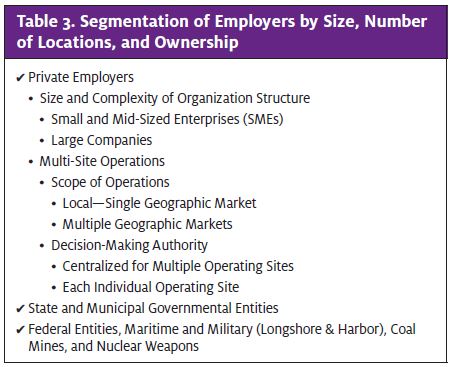
Within industries whose job requirements lead to increased utilization of occupational medicine, employers may be in the public or private sector, large or small, centralized or decentralized in their decision-making. In addition, participation in the workers’ compensation system may vary if employees fit certain profiles—for instance, civilian military contractors working overseas and those who work with nuclear energy have their own distinct workers’ compensation systems. To be successful in
growing a base of occ med clients, an urgent care operator must first understand how services get directed to particular providers. Table 3 illustrates how the choice of an occ med provider may be influenced by any number of individuals in any number of locations.
Workers’ Compensation Payors
Workers’ compensation is defined as a “no-fault system of wage replacement, medical and life insurance bene- fits paid to employees who suffer work-related injuries or diseases. The system was founded for the dual pur- pose of providing income security for workers and their families while also eliminating the risk of employers being sued in tort for workplace injuries.
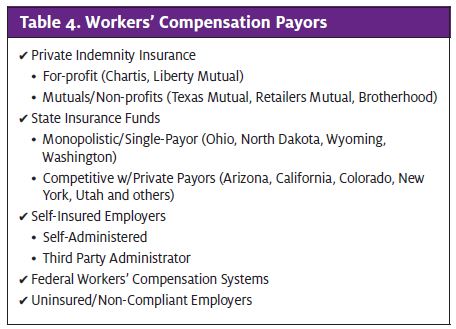
Employers are required by law to purchase workers’ compensation insurance or demonstrate their qualifica- tions to self-insure. As with an employee’s personal health insurance, workers’ compensation medical providers are paid by third parties—private indemnity carriers, state funds, or self-insured employer claims administrators. Table 4 lists the different categories of workers’ compensation payors. In order to be paid for providing workers’ compensation services, a medical provider must become contracted and credentialed with major workers’ compensation carriers following a process that’s similar to contacting and credentialing with a private health plan.
Direction of Care
In the realm of individual health insurance, patients with indemnity policies can choose their providers freely while those with PPOs or HMOs often have their choices limited to providers contracted with the insurance plan. Depending on state law and the structure of the employer’s workers’ compensation coverage, the same concepts apply to direction of care for workplace injuries.
- Workers Choice – Employee may freely choose any provider authorized to treat workers’ com- pensation
- Preferred Provider Panel – Employee may choose from a network of authorized providers, which may include the employer’s or payor’s preferred provider.
- Payor/Employer Directed—Employer or payor requires the employee to utilize its preferred provider.
Understanding the direction of care is a critical determinant of how a workers’ compensation provider markets its services. In states where workers have free choice, some providers advertise “workplace injury services” directly to the general public. But in states that allow for panels or directed care, urgent care centers develop sales relationships with employers, third party administrators, and provider networks. Similar to the rise of Health Maintenance Organizations to control costs related to personal medical care, managed care is emerging in workers’ compensation with case managers employed by third parties increasingly directing medical care to in-network providers.
An employer’s size typically determines its complexity and delineation of specific roles and responsibilities related to occ med. For example, single-site small businesses often have one individual responsible for ensuring that new hires are drug tested and existing employees are compliant with federally prescribed physicals, and assimilating injured workers back into their jobs. Such “generalists” are usually the contact for “all things occ med.” By contrast, large organizations may have distinct capabilities in risk management, safety, compliance, benefits, and other disciplines—in addition to general human resources and operations management. So dealing with large organizations may entail unique contacts for each individual service—with workers’ compensation referrals coming from a different source than pre-employment physicals and random drug screenings. In addition, large organizations with multiple sites may make decisions at the corporate office on where to direct care for all locations, or they may leave decision-making to local managers. Occ med providers with a national footprint, such as Concentra, USHealthworks and Kaiser Permanente, have an advantage over local independents in their ability to serve third party administrators and national accounts like retail chains, airlines, and trucking companies at multiple sites throughout the country.
Workers’ Compensation Provider Process
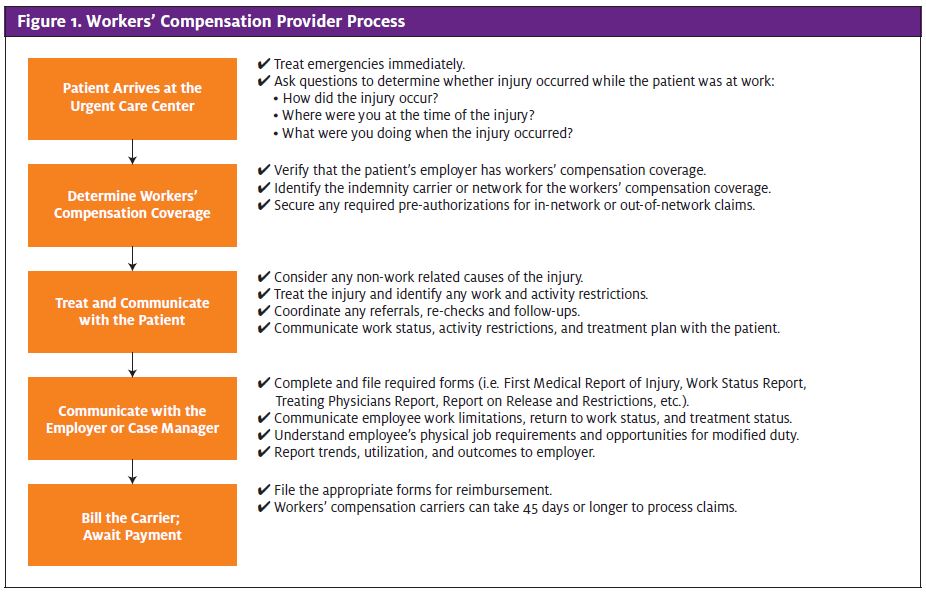
Figure 1 illustrates the process that workers’ compensation providers typically follow, from the time a patient arrives at the center through receipt of payment from the insurance carrier. While the general process is the same in all states, the authorizations required, forms to complete and file, evaluation of causation, and payment timelines do vary so it’s critical that a provider understand the laws in his/her community.
Because workers’ compensation is generally employer- directed care, building a strong reputation as a workers’ compensation provider entails:
- Controlling the number of reportable incidents (these affect employer’s workers’ compensation premiums);
- Evaluating and documenting causation including ruling out non-work-related causes;
- Reducing time away from work by understanding and utilizing modified duty when appropriate;
- Getting employees back to full recovery (and full job activity) quickly; and
- Communicating with the
Delivering an excellent patient experience with short wait times is also important—an employer may be hesitant to refer employees, no matter how fine the medical outcomes, if they perceive their employees will be treated poorly. That’s why, even if the employer picks up the bill, the patient must be treated as the client. Treating patients well in occupational medicine pays dividends for the urgent care operator as satisfied patients will often return (with their families) for their personal medical needs.
Conclusion
The term “occupational medicine” generally refers to “workers’ compensation injury care,” “preventive and compliance services,” and “health and wellness” in which the client is an employer. Success in selling occ med starts with identifying local employers in industries with a propensity for injuries or with compliance requirements for physicals and drug screenings, under- standing the employers’ organization structure and identifying key decision-makers, contracting with the appropriate workers’ compensation insurance carriers and provider networks, understanding the required paperwork, establishing processes to treat patients with a focus on minimizing downtime, and last, communicating with the employers. Expanding into occ med requires a long-term commitment to develop the business, a willingness to understand and respond to employer and employee needs, and also a significant investment in sales and operations resources while the business ramps up.

