Published on
Urgent message: Injection/aspiration therapy for selected musculoskeletal complaints is becoming more common in urgent care practice. Part 2 of this series offers step-by-step guidance on treatment of conditions from “tennis elbow” to bursitis and cysts.
THOMAS V. GOCKE, III, MS, ATC, PA-C, DFAAPA
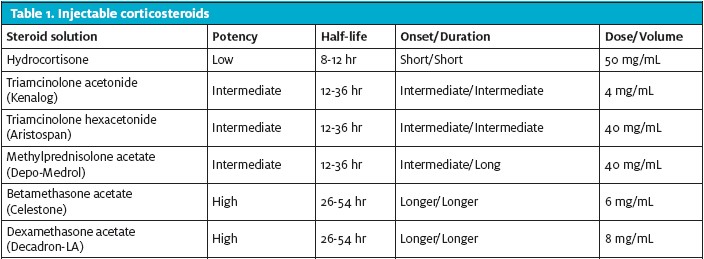
The focus of Part 1 of this series, in the September issue of JUCM, was on understanding the inflammatory response, use of corticosteroids and anesthetic agents (Table 1), pre- and post-aspiration/injection considerations, and the approach to injections for subacromial impingement syndrome. Part 2 reviews approaches to lateral epicondylitis, olecranon and prepatellar bursitis, ganglion cyst, trochanteric bursitis, knee injection and aspiration, and evaluation of joint infection. The overall objective is to highlight common presenting symptoms and successful approaches to injection or aspiration that urgent care providers can use in practice. As noted in the previous installment, any injection or aspiration procedure should be performed using sterile technique.
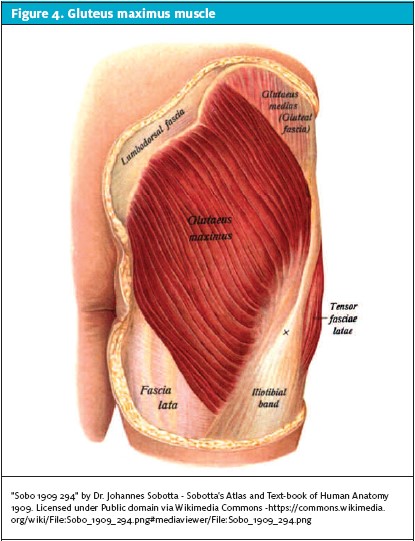
Lateral Epicondylitis
Also known as “tennis elbow,” lateral epicondylitis can be a source of elbow pain for many patients. Previous injury, repetitive motions, weight lifting, heavy lifting and carrying and trauma are all common causes. Corticosteroid injection to the lateral epicondyle can be a technical challenge because of difficulty identifying the point of maximal tenderness and delivering an injection to the appropriate anatomic location. Remember that the radial nerve (posterior interosseus and sensory branches) lies close to the origin of the common extensor tendons (CET) and, in some cases, infiltration of this nerve structure can lead to numbness and eventually rebound pain and burning in the proximal elbow.1-8
The best patient position for injection for tennis elbow is seated with the elbow supported on the exam table, which facilitates access to the lateral elbow and the origin of the CET (Figures 1A and 1B). The best way to isolate the CET tendon origin is to flex the elbow maximally. The lateral flexor crease formed in this max flexed position allows the provider to specifically palpate the extensor carpi radialis brevis (ECRB) origin of the common extensor tendon. This is also usually the point of maximal tenderness.
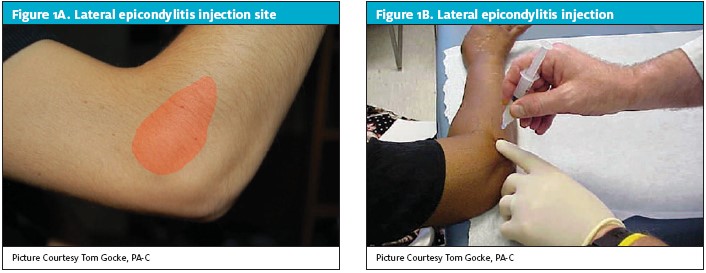
Once the appropriate landmarks are identified, prep and palpate as described in Part 1 of this series. As a guide for injection, place your index finger next to the injection site and ensure that the syringe is perpendicular to the site to prevent an unintended injection into the radial nerve structures. Most patients report no pain with the procedure; those with pain and numbness of the arm should be brought back for a follow-up exam. Because the injection is intended to deliver medication at the tendon-bone interface, only a small volume of injection solution is necessary. Use of a 26-G .-inch needle is appropriate to introduce 0.5 mL of 0.25% bupivacaine, 0.5 mL of 1% lidocaine, and 1 Ml of triamcinolone acetonide 40 mg/mL. In rare cases when a patient has muscle hypertrophy of the forearm muscles, a 1-inch or 1 .-inch hypodermic needle can be used for injection.1-3, 6-10
As with shoulder injection, patients treated for tennis elbow should be discharged with instructions to rest for 24 hours after injection. A wrist splint is appropriate for those who have severe range of motion (ROM) decreases or pain at the CET that intensifies with wrist motion. Post-injection cryotherapy also should be recommended. At 3 to 5 days post-injection, encourage patients to start a gentle stretching program for their affected wrist and elbow.1-3,11-13
Olecranon and Prepatellar Bursitis
Olecranon and prepatellar bursitis are common conditions associated with acute injury and chronic recurrent pressure on the elbow and knee. Regardless of the mechanism of injury, the inflammatory response in the bursae results in swelling, warmth, and pain over the affected area. In most cases, olecranon and prepatellar bursitis are not a result of bacterial infection but there are cases in which bacteria penetrate skin lesions and can lead to infection (Figure 2). Therefore, it is important for providers to pay attention to skin injuries, especially when they are attempting to aspirate and/or inject the olecranon/prepatellar bursae (or any joint or other bursae).1-3,9,14-18
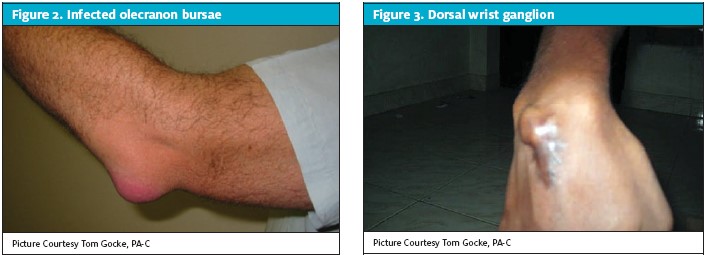
The best patient position for an aspiration and/or injection of the olecranon/prepatellar bursae is the semi-sitting or recumbent position. This allows the elbow to be flexed across the body or the knee to be flexed 15 degrees on a rolled up towel, thus facilitating better access to the inflamed bursae. Because of the prominence of the bursae, it is easy to identify the fluid/swollen area. Pick a dependent entry point on the bursae to allow for better drainage during aspiration and pay particular attention to the color and consistency of the fluid. If the aspirated fluid is clear and infection is not a concern, the hub of the syringe can be changed sterilely and the corticosteroids injected into the bursae thru the aspiration needle. If there is any suspicion or concern about infection or the fluid is turbid, the fluid should be sent to the lab for appropriate analysis. If there is any question about the possibility of infection, administration of corticosteroids into the bursae is contraindicated. (See the section on evaluation of joint infection at the end of this article.)
As a guide for aspiration or injection, use your sterile, gloved index finger and thumb to squeeze the swollen bursae and force fluid closer to the skin surface. Once the needle enters the bursae, there should be little resistance with aspiration of fluid or injection of cortisone–anesthetic solution. In most cases, patients report little pain with the procedure. A 22-G needle can be used for injection into the bursae and an appropriate solution is 1 mL 0.25% bupivacaine, 1 mL 1% lidocaine, and 1 mL of triamcinolone acetonide 40 mg/mL. If aspiration is planned before injection, 3 mL of 1% lidocaine can be used to anesthetize the skin and then the skin can be prepped a second time prior to aspiration. A 16- or 18-G needle is appropriate for aspiration of fluid. If there is no concern for infection (clear bursae fluid, no skin manifestations and negative exam and history), after aspiration, the hub of the syringe can be changed sterilely and a steroid injection delivered into the bursae.1-3,9,15,17,18
Ganglion Cyst
Ganglion cysts of the dorsal wrist are common and occur as a result of injury to the dorsal carpal joint capsule. A defect in the lining of the wrist joint allows a portion of the synovium to extrude through the defect and as it fills with synovial fluid, a liquid-containing sack is formed.
Ganglion cysts in the dorsal wrist area often grow and shrink depending on wrist motion and repetitive activity. Patients typically present for treatment because of significant wrist pain caused when the fluid or the ganglion cyst fails to decompress and distension occurs.
Transillumination is a simple way to determine if the swollen area over the dorsal wrist is a fluid-filled mass. Solid masses do not light up whereas fluid-filled masses transmit light. Some ganglion cysts resolve with aspiration and injection. In most cases, however, this form of treatment is temporary and frequent recurrences necessitate surgical excision. Aspiration and injection with corticosteroids can provide a relatively long duration of symptom relief and therefore are a great first line treatment. As with other areas for injection or aspithe provider should pay particular attention to skin structures and the possibility of infection, either to the skin or the joint. Any suspicion that the patient has an infection should cause the provider to rethink the treatment decision-making process.1-3,19-21
The best position for aspiration and/or injection of a ganglion cyst is with the patient seated. Support the wrist with a small roll of towels and have the patient flex it slightly to expose the ganglion dorsally and make it more prominent (Figure 3). Pick a dependent entry point on the ganglion to allow for better drainage during the aspiration process and pay particular attention to the color and consistency of the aspirated fluid. In most cases, the ganglion fluid is a gelatinous substance that can be difficult to draw through a needle and syringe. If there is any suspicion or concern about infection, the fluid should be sent to the lab for appropriate analysis. (See the section on evaluation of joint infection later in this article). In the case of possible infection, administration of corticosteroids into the ganglion is contraindicated. If the aspirated fluid is clear/gelatinous and infection is not a concern, change the hub of the syringe using a sterile technique and inject corticosteroids into the ganglion thru the aspiration needle.
The guides and techniques for injection/aspiration of a dorsal wrist ganglion also can be used when attempting to aspirate/inject bursae, including the same anesthetic/corticosteroid injection solutions. A word of caution about aspirating or injecting volar wrist ganglions. It is not recommended that any urgent care pro vider attempt to aspirate or inject a volar wrist ganglion, particularly if it overlies the radial artery. In most cases, such fluid-filled sacks are, indeed, ganglions, but radial artery aneurysms also can have a similar presentation. Attempting to aspirate and inject a radial artery aneurysm can lead to severe consequences for the patient and the provider. Urgent care providers who do not have color duplex Doppler ultrasound should refer these patients to an experienced provider who is capable of managing complications, should a fluid-filled cyst turn out to be an aneurysm.1-3,19-21
Discharge instructions for aspiration/injection are the same as for the other anatomical sites and as described in Part 1. Placement of a bulky dressing and an elastic wrap over the dorsal hand helps maintain pressure over the ganglion and reduces the chance of reaccumulation of fluid. A wrist brace also can be used to minimize wrist motion, particularly in patients who perform manual labor. The bulky dressing and/or wrist brace should be worn for 3 to 5 days before it is removed and normal activities are resumed. Remind patients that despite aspiration and or injection of their dorsal wrist ganglion, there is still a chance that the ganglion fluid could return.1-3,11-13
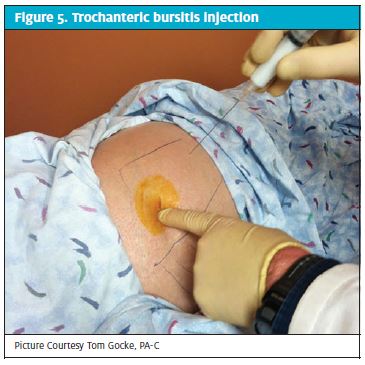
Trochanteric Bursitis
Acute and chronic injury, altered gait, change in activity levels, obesity, and acute/chronic back pain all can cause trochanteric bursitis. The trochanteric bursa is located adjacent to the bony prominence of the lateral hip joint, between the iliotibial band and the greater trochanter. The tendons of the gluteus medius and maximus also overlie this area (Figure 4). Regardless of the mechanism of injury, the inflammatory response in the bursa results in swelling, warmth and pain over the affected area. This distends and “overstuffs” the native anatomy, resulting in increased pressure over the bursa, from the iliotibial band, on flex/extension of the knee or hip joint. Patients with trochanteric bursitis will complain of pain with getting in or out of a car/chair and lateral hip pain when sleeping on the affected side. Lateral hip pain when walking on level ground or climbing stairs or inclines also is common. Back pain can occur secondary to an altered gait as a result of trochanteric bursitis. Septic bursitis in the trochanteric region is rare but does occur so it is important to be observant for skin injuries before injecting the trochanteric bursae.1-3,10,22,23
The best patient position for an injection of the trochanteric bursae is the lateral decubitus, which allows for direct visualization of the lateral hip/greater trochanter and palpation of the area of maximal tenderness. The point of maximal tenderness is usually the spot where the bursa lies beneath the Iliotibial band and greater trochanter. Palpation multiple times may be necessary in patients with extra tissue over the trochanter, to ensure that the needle is guided toward the greater trochanter. A key point with guiding the needle into the bursae is to keep it perpendicular to the trochanter. That helps ensure that the sciatic nerve is avoided during your injection (Figure 5).
Antiseptic soap should be used to prep the skin for trochanteric injection because the lateral hip is not far from the anus and there is a possibility of contamination with enteric bacteria. After prepping the skin, use a sterile, gloved index finger to ensure injection of the area of maximal tenderness, advancing the needle until bone is contacted. If injection without resistance is not possible, withdraw the needle slightly and again attempt to inject. To confirm that the sciatic nerve has been avoided, always ask patients during injection whether they are experiencing pain or burning sensations radiating down their leg. If that is the case, abort the injection and withdraw the needle. Most patients report no pain with injection. A 22-G spinal needle is preferable to skin injuries and to the characteristics of fluid aspirated from the knee is important to determine whether to proceed with injection. Clear to yellowish fluid (looks like lemonade) is usually consistent with synovial fluid and typically has a low probability of infection. Bloody, dark, turbid fluid, however, should significantly raise a provider’s suspicions for infection, particularly when a patient’s history includes comorbidities such as diabetes or immune compromise. If fluid aspirated from the knee is questionable, it should be sent for analysis before the joint is injected because proceeding with a corticosteroid injection could greatly increase risk of infection.1-3,15,16,24
The best patient position for knee injection is sitting or semi-sitting. Having a patient lie down with the affected knee hanging over the edge of the bed is an alternative for those who are anxious about getting an injection or have a history of fainting during injection.
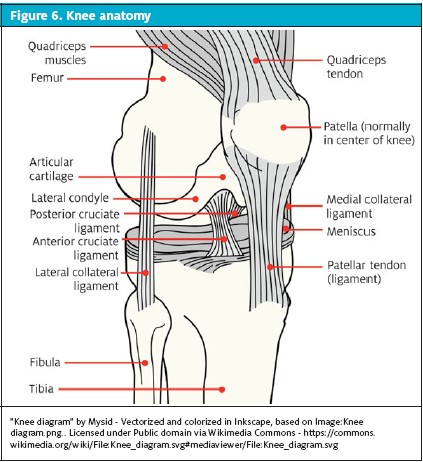
After examining the skin and associated joint structures, identify the lateral joint window and use it as the injection site. This lateral joint window is bordered medially by the patellar tendon, inferiorly by the proximal tibia, superiorly by the lateral patella and laterally by the articulation of the lateral femoral condyle and proximal tibia (Figure 6). Imagine the aiming point as the femoral notch when introducing the needle into the joint. Do not plunge the needle to the hub because that might result in contacting the articular surface of the lateral femoral condyle, thus causing pain.
Once the needle has advanced past the infrapatellar fat pad (Hoffa’s fat pad), the injection should flow freely with little or no resistance, however, if resistance is encountered or contact is made with the bone, simply reposition the needle. Patients commonly report a full feeling in the knee after the injection is complete. A 22-G needle should be used for injection. An appropriate injection solution is 3 mL of 0.25% bupivacaine and 2 mL of triamcinolone acetonide, both without epinephrine.1-3,15,16, 25
Knee Aspiration
The best position for knee aspiration (with or without injection) is with the patient supine, which works very well for those who are anxious about having a needle inserted into their knee or who have a history of fainting during injection. The aspiration and injection site is the superior lateral arthroscopic portal region, which is approximately one thumb width cephalad to the superior edge of the patella and one thumb width inferior (toward the floor) (Figure 7). Imagine the aiming point superior and parallel to the top border of the patella. The entry angle should neither be parallel to the floor nor too steep because an angle too flat will cause the needle to strike the lateral femoral condyle and plunging the needle to the hub could result in contacting the articular surface of the lateral femoral condyle, thus causing pain. Skin prep for a knee aspiration is the same as for the other anatomical sites and as described in Part 1.
Some providers elect to introduce the aspiration needle into the joint without use of local anesthesia but that can be very painful and make a patient more apprehensive. If anesthesia is chosen, 10 mL of 1% lidocaine is appropriate. After the local anesthetic agent has taken effect, the skin at the aspiration site should be prepped a second time before the needle is introduced.
Once the needle has been introduced into the suprasynovial pouch, aspirate should flow freely without resistance and little effort should be needed to withdraw fluid from the knee. In the case of resistance or contact with the bone, the needle should be repositioned. Patients commonly report a quick, sharp pain as the needle passes through the joint capsule. If it is difficult to get the fluid to flow out of the knee, a sterile, gloved hand can be used to milk fluid out of the suprasynovial pouch, forcing it closer to the aspiration needle (Figure 8).
To administer a steroid injection after aspiration, leave the aspiration needle in the suprasynovial pouch, change the hub of the aspiration syringe and attach the injection syringe. Then inject the knee and withdraw the needle from the knee joint. An appropriate injection solution is 3 mL 0.25% bupivacaine and 2 mL triamcinolone acetonide 40 mg/mL, both without epinephrine.1-3,15,16,25
Discharge instructions are as for the other anatomical sites, including rest and cryotherapy. A bandage and an elastic wrap should be applied to the knee prior to discharge to minimize reaccumulation of fluid and it should remain in place for 24 hours.1-3,11-13
Patients who present with one or more hot, swollen, erythematous, painful joint(s) should make a provider suspicious of a septic joint until proven otherwise. A patient’s history and physical examination should help the provider to gain more insight into why a patient is presenting with a swollen joint.
Patients who have a history of rheumatoid arthritis (RA) and any joint with structural irregularities (traumatic/arthritic/surgical) are at increased risk of developing septic arthritis. Important risk factors to consider are history of total joint arthroplasty (hip and knee most common), intravenous drug use, diabetes, previous corticosteroid injection history, skin ulcers/dermatitis and alcoholism. In cases in which clinical suspicious of infection is high, necessary steps should be taken to help confirm or refute that the patient has a joint infection. In our facility, we routinely obtain laboratory studies—complete blood cell count with differential, basic metabolic panel, erythrocyte sedimentation rate (ESR-sed) and C-reactive protein (CRP)—to determine baseline values for infection. These tests provide a general overview of a patient’s systemic reaction to a possible joint infection. It is important to remember that in the early presentations of a joint infection, the white blood cell (WBC) count, ESR and CRP may be low or in normal range but that does not completely rule out a joint infection. (Note: we do not routinely order blood cultures on patients we suspect of having a joint infection. However, the overall past medical and clinical history may make this a necessity, particularly in patients who have chronic illness or autoimmune diseases, who are taking immune-suppressing medications, or who have overwhelming sepsis).24, 26-30
In my opinion, the most important information, aside from the patient’s history, is the analysis of joint fluid. Analysis of joint fluid can not only help to confirm the diagnosis it also will help to identify organisms/crystal associated with joint infection/inflammation. That is why it is so important to aspirate the affected joint(s) prior to starting any patient on antibiotic therapy. We routinely order the following labs and cytology on any aspirated fluid from a joint: Gram stain, cell count, crystals and cultures (aerobic/anaerobic/acid-fast bacillus [AFB]). The Gram stain, we hope, will give us an idea about the potential organism that is causing a joint infection while we await final culture results. Staphylococcus aureus and Streptococcus are the two most common pathogens found in septic joints (91%).24,27-29 However, with methicillin-resistant S. aureus (MRSA) on the rise, it should be considered a common pathogen as well. Gram-negative enteric bacteria can be associated with joint infections and may result from hematogenous spread. Urinary catheters, feeding tubes, and IV devices also can contribute to infection. Final cultures for aerobic and anaerobic organisms are typically completed after 3 days of incubation.
Although routine culture for AFB is not common, providers should take into consideration a patient’s nationality, living situation, world travel and potential tuberculosis exposure risk when deciding whether to include this test on the culture request.30
Controversy surrounds the cell count analysis of joint fluid. Several studies looking at joint fluid cell counts to determine a threshold for establishing joint sepsis indicate that for WBC counts >25,000 and good clinical correlation, the likelihood of joint sepsis is increased. A comprehensive review of the medical literature confirms that joint fluid WBC >25,000 in native joints and WBC >10,000 in prosthetic joints are consistent with joint sepsis. A higher percentage of polymorphic neutrophils in the joint fluid analysis is considered supportive but not necessarily a deciding factor in determining joint sepsis. Patient history, fever presentation, comorbid factors, joint fluid analysis, ESR, and CRP all aid in the determination of joint infection.36-41
Conclusion
Injection therapy for patients with selected musculoskeletal complaints is becoming more common in urgent care practice. Although performing these procedures is not technically demanding, they do require that an urgent care provider have a thorough understanding of the pertinent musculoskeletal anatomy. Discharge instructions should be procedure-specific and detailed to help guide patients through their recovery process. They should briefly answer a patient’s potential questions, alert a patient to potential adverse effects or complications, and offer guidance on what to do in the case of problems following an injection. Taking the extra time to discuss with patients the intended effects and benefits of injection therapy, general risks, and what to expect in the post-procedure course will go a long way in allaying fears and improving customer service in urgent care.
References
- Diagnostic & Therapeutic Injections of the Shoulder Region www.aafpa.org/afp/2003/0315/p1271.html
- Gocke TV. Common injections & joint aspirations for MSK injuries. Orthopaedic Educational Services, Inc. 2013 www.orthoedu.com
- Mercier L, Injection & Aspiration Therapy: Practical Orthopaedics 4th edition, Mosby, St Louis, 1995, p 453-457
- Lateral Epicondylitis Injection. www.emedicine.medscape.com/article/103440-overview
- Best Treatment for Lateral Epicondylitis Remains a Matter of Debate www.aaos.org/news/aaosnow/dec12/clinical2.asp
- Scher DL. Lateral eEpicondylitis. Orthopaedics. 2009;32(4)
- Griffin LY. Procedure-Tennis Elbow Injection. Essentials of Musculoskeletal Care. 3rd edition. American Academy of Orthopaedic Surgeons. 2005; p 267-268.
- McNabb JW. A Practical Guide to Joint & Soft tissue Injection & Aspiration. 2nd edition. Lippincott Williams & Wilkins. 2010; p 69.
- Mercier L. Elbow. Practical Orthopaedics. 4th edition. Mosby, St Louis: 1995. p 86-89.
- Griffin LY. Trochanteric bursitis. Essentials of Musculoskeletal Care. 3rd edition. American Academy of Orthopaedic Surgeons: 2005. p 461-466.
- Knight KL. Pain and pain relief during cryotherapy. Cryotherapy: Theory, Technique and Physiology. 1st edition. Chattanooga Corporation, Chattanooga, TN:1985. p 127-137.
- McNabb JW. A Practical Guide to Joint & Soft tissue Injection & Aspiration. 2nd edition. Lippincott Williams & Wilkins:2010. p 3-5.
- McNabb JW. A Practical Guide to Joint & Soft tissue Injection & Aspiration. 2nd edition. Lippincott Williams & Wilkins: 2010. p 8-11.
- Hansen BP, Beck CL, Beck EP, Townsley RW. Postarthroscopic glenohumeral chondrolysis. Am J Sports Med. 2007;35:1628-1634.
- Mercier L. Knee. Practical Orthopaedics. 4th edition. Mosby, St Louis: 1995. p 207-225.
- Griffin LY. Procedure-knee aspiration/injection. Essentials of Musculoskeletal Care. 3rd edition. American Academy of Orthopaedic Surgeons: 2005. p 571-573.
- Griffin LY. Procedure-olecranon bursa aspiration. Essentials of Musculoskeletal Care. 3rd edition. American Academy of Orthopaedic Surgeons: 2005. p 272-273.
- McNabb JW. A Practical Guide to Joint & Soft tissue Injection & Aspiration. 2nd edition. Lippincott Williams & Wilkins: 2010. p 73.
- Mercier L.Forearm, wrist, hand. Practical Orthopaedics. 4th edition. Mosby, St Louis: p 98-104.
- Griffin LY. Procedure-dorsal wrist ganglion aspiration. Essentials of Musculoskeletal Care. 3rd edition. American Academy of Orthopaedic Surgeons: 2005. p 367.
- McNabb JW. A Practical Guide to Joint & Soft tissue Injection & Aspiration. 2nd edition. Lippincott Williams & Wilkins: 2010. p 98.
- Mercier L. Hip. Practical Orthopaedics. 4th edition. Mosby, St Louis: 1995. p 183-184, 198.
- McNabb JW. A Practical Guide to Joint & Soft tissue Injection & Aspiration. 2nd edition. Lippincott Williams & Wilkins: 2010. p 135.
- Approach to Septic Arthritis www.aafp.org/2011/0915/p653
- McNabb JW. A Practical Guide to Joint & Soft tissue Injection & Aspiration. 2nd edition. Lippincott Williams & Wilkins: 2010. p 142-150.
- Life in the Fast Lane: http://lifeinthefastlane.com/education/procedures/local-anaesthetic
- Mathews CJ and Coakley: Septic arthritis: current diagnosis and therapeutic algorithm. Curr Opin Rheumatol. 2008;20:457-462.
- Abbasi D. Orthobullets- Septic Arthritis www.orthobullets.com/trauma/1058/septic-arthritis—adult
- Aman S, Gupte CM, Liyanage SH, et al. The value of synovial fluid analysis in the assessment of knee joint destruction in arthritis in a three year follow up study. AnRheum Dis. 1999;58:559-562.
- Opara TN, Risteli J, Luukkainen R, et al. Tuberculous arthritis of the knee with Staphylococcus superinfection. J Bone Joint Surg BR. 2007;89-B(5):664-666.