Published on
Urgent Message: Rib fractures most commonly occur after blunt chest injury. Consider serious associated injuries such as pneumothorax, hemothorax, and pulmonary contusion when assessing patients with suspected rib fractures. Ensuring appropriate analgesia is critical for reducing the risk of complications.
Dustin M. Nelson, BS; Shering Torres, MAS, MD; Michael Weinstock, MD
Citation: Nelson DM, Torres S, Weinstock M. Urgent Care Considerations for the Patient with Suspected Rib Fracture. J Urgent Care Med. 2025; 19(4): 13-21
Questions for the Clinician at the Bedside
- When should rib fractures be suspected?
- Which patients with rib fractures should be referred to the emergency department?
- What associated injuries should be considered in patients with blunt chest injury?
- What are the most critical aspects of excellence in the urgent care management of rib fractures?
Editor’s Note: While the images presented here are authentic, the patient case scenarios are hypothetical.
Abstract
Rib fractures typically occur after blunt trauma to the thoracic region. The identification of a rib fracture is a marker for potential significant blunt force to the torso as well as an opportunity to decrease the risk for complications including pneumonia, which is more likely in elderly patients. The recommended initial imaging study of choice is plain chest radiography (CXR). Rib x-ray series, conversely, are not recommended as they do not affect patient outcomes or management. The priorities for urgent care (UC) management of patients with suspected blunt chest injuries and suspected rib fractures center around considering and excluding serious associated injuries (eg, pneumothorax, pulmonary contusion, etc.) and ensuring appropriate analgesia to prevent subsequent complications.
Clinical Scenario
A 56-year-old man presented to the urgent care with sharp right thoracic pain, which began after he fell down the stairs in his home earlier that day. He said he feels pain when taking deep breaths and pain with any movement of his torso. He denied head trauma, head or neck pain, vomiting, numbness, tingling, dizziness, abdominal pain, hematuria, hematochezia, or melena.
The patient was afebrile. The remainder of his vitals revealed a heart rate 106 beats per minute (bpm), respiratory rate of 24 breaths per minute, and blood pressure of 138/92 mmHg. His oxygen saturation was 94% on room air. On exam, the patient appeared generally uncomfortable. He was splinting and holding his right side. On pulmonary exam, he was tachypneic with shallow breathing, but his lung sounds were clear and symmetric. His abdomen was soft and non-tender to palpation. He was tachycardic with a regular rhythm. Visual examination of the chest wall revealed a small area of ecchymosis of the right lateral posterior chest, which was tender to palpation with crepitus.
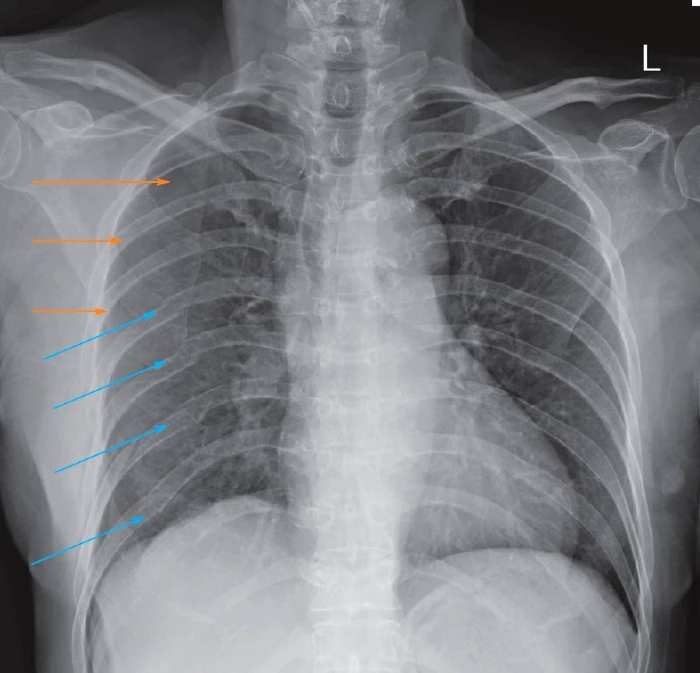
An upright chest x-ray (CXR) was performed, which demonstrated multiple posterior right-sided rib fractures as well as a right-sided pneumothorax (Image 1).
Image 1. Multiple Right Sided Rib Fractures (blue arrows) with Pneumothorax (orange arrows)
Epidemiology
Rib fractures are frequently encountered among patients after sustaining blunt thoracic trauma presenting to the emergency department (ED) or UC, with falls and motor vehicle collisions (MVC) accounting for the largest proportion of cases.[1],[2] As patients age, rib fractures can occur with progressively less force. In older patients, rib fractures commonly occur with low mechanism injuries such as falls from standing.[3] Based on aggregate data from the National Trauma Data Bank, rib fractures have been found to occur more frequently in Caucasian and male patients with a median age of 51 years at the time of diagnosis.[4] The most common ribs fractured are ribs 5-9,1 with a median number fractures being 2.[5] Fracturing ribs 1-3 requires higher force mechanisms as they are anatomically well-protected by the larger thoracic muscles and shoulder girdle, and such fractures are a marker of more significant mechanism.1
Blunt chest trauma can produce myriad serious and potentially life-threatening injuries. In many ways, rib fractures serve primarily as an indicator that the thoracic region has sustained significant blunt mechanical forces, and therefore, heightened vigilance in evaluating for associated injuries is warranted. Morbidity and mortality associated with rib fractures increases linearly with the number of fractured ribs.5
Importantly, to date, there have been no studies published describing the prevalence of rib fractures and associated injuries in patients presenting to UC centers after thoracic trauma. In a large retrospective ED-based study of patients with rib fractures, the most frequent complication encountered was pneumothorax (PTX) (37.2% of cases) followed by hemothorax (HTX) (26.8% of cases), pulmonary contusion (17.2% of cases), and flail chest (5.8% of cases).[6] A flail chest occurs when the chest wall moves paradoxically with inspiration and is associated with scenarios where there are multiple consecutive rib fractures on the ipsilateral side of the chest with multiple sites of fracture in the affected ribs.[7],[8] Less commonly other serious associated injuries may occur such as tracheobronchial tree injury, blunt aortic injury, intra-abdominal solid organ injury, injury to the great vessels (particularly with 1-3 rib fractures), sternal fracture, and cardiac contusion.7,[9],[10]
A systematic review of 73 studies on patients with chest injury revealed the most significant risk factors for mortality associated with blunt chest wall trauma:[11]
- Age >65 years
- Presence of 3 or more rib fractures
- Presence of comorbid cardiopulmonary disease
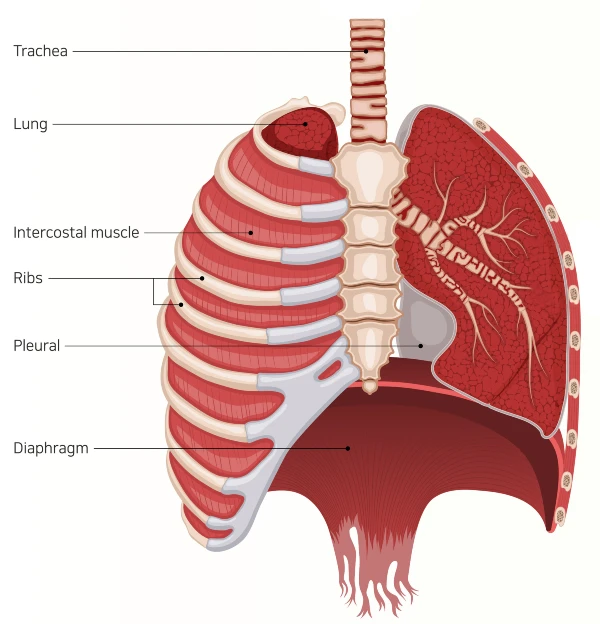
Understanding The Anatomy
The thoracic cavity contains many vital organs and structures including the heart, lungs, great vessels, and esophagus; these structures are protected by 12 paired ribs and the associated musculature of the chest wall. Respiratory inspiration is created by diaphragmatic contraction, which leads to depression of the diaphragm, expansion of the thoracic cavity and negative intrathoracic pressure. The diaphragm’s movement is innervated by the phrenic nerve. During expiration, the diaphragm elevates to the level of the 4th intercostal space (approximately the nipple line) and depresses to the level of the 12th intercostal space with maximal inspiration.[12] (Image 2) Therefore, depending on the phase of the respiratory cycle, intra-abdominal organs may variably be susceptible to the forces of blunt thoracic trauma as well. While this is more significant in cases of penetrating thoracic trauma, it is important to consider injuries to abdominal contents with rib fractures from blunt trauma inferior to the 4th intercostal level as well. Intra-abdominal injuries and hemoperitoneum may present with shoulder pain due to the phrenic also providing nerve’s sensory innervation of the diaphragm.[13]
Image 2. Thoracic Anatomy: Ribs and Diaphragm
History
Before taking a history, begin with an assessment of the patient’s stability by reviewing vital signs and general level of distress. As with all trauma histories, attention should be paid to understanding the timing and mechanism of the injury. Consider and inquire about injuries to the head, spine, abdomen, and/or extremities as patients may have sustained multiple other injuries after falls or MVCs. If there was an altercation, inquire about other injuries such as a closed fist injury, head or neck injury; explore if the patient may be a victim of criminal assault such as intimate partner violence or elder abuse. In young children, rib fractures are a conspicuous finding and are highly correlated with non-accidental trauma (NAT).[14]
Have the patient indicate where the area of maximal pain is located. Pain from thoracic trauma is generally pleuritic in nature, and this historical feature does not distinguish rib fracture from chest wall contusions or deeper injuries such as PTX or HTX. Patients may complain of inability to take a deep breath (ie, “splint”) because the pain is exacerbated with movement of the chest wall.7 Similarly, pain from blunt thoracic trauma is typically exacerbated by body movement. While pain being exacerbated by movements does suggest that the chest wall sustained injury, it does not exclude the possibility of associated injuries to deeper structures (eg, pulmonary contusion, PTX).[15]
While significantly less common, atraumatic rib fractures, known as stress fractures, can occur in certain populations as well. In patients with bone diseases—such as osteoporosis or cancer metastatic to the ribs—fractures can occur without blunt force after coughing or sneezing.[16] Athletes who row can sustain stress fractures of the lower ribs and baseball players (particularly adolescents) can have upper rib fractures from throwing or forcefully swinging the bat.[17] ,[18]
Physical Exam
As with all trauma evaluation, begin with assessing the patient’s clinical status and ensure they are breathing and mentating adequately and in no acute distress. Patients with hypotension, significant tachycardia, or hypoxemia after thoracic trauma warrant immediate activation of emergency medical services (EMS). It is important to not postpone EMS activation for interventions such as CXR as this can result in unnecessary delays to receiving definitive care among patients with time-sensitive diagnoses.
After a primary survey and review of the vital signs, assess for any external evidence of trauma to the head and neck before examining the torso. It is critical to expose the patient’s chest, back, and abdomen, inspecting for signs of trauma such as ecchymoses, abrasions, or lacerations. Observe the patients respiratory pattern noting if there is splinting, paradoxical chest wall movement, or significant tachypnea. For patient’s presenting after a MVC, look for the presence of a “seatbelt sign”—bruising of neck, chest, or abdomen from pressure from the seat belt, as this has been found to be associated with a 4-fold higher likelihood of significant intrathoracic injury.[19]
Rib fractures are less common in children than adults as the ribs and chest wall are more pliable. Bruising of the chest in young children, while not pathognomonic for NAT, should raise suspicion for underlying rib fractures. However, in 1 series of cases of NAT, 58% of children with underlying rib fractures did not show visible bruising.[20]
When palpating the chest, assess the area of greatest tenderness. Palpate the entirety of each rib from the spine to the sternum surrounding the area of the patient’s pain paying attention to any signs of step-off irregularities or crepitus. Point tenderness or palpable deformity increases the likelihood of underlying rib fracture.[21] Careful auscultation of each hemithorax in comparison to the contralateral side may reveal decreased breath sounds. It is important to note that while decreased breath sounds can be present with PTX and/or HTX, this finding is insensitive, and normal breath sounds should not be used to rule out these diagnoses or as rationale to forego thoracic imaging. In one series of trauma patients with PTX and/or HTX, auscultation failed to identify any abnormality of breath sounds in 42% of cases.[22]
Because of the range of positions of the diaphragm through the respiratory cycle, patients with blunt chest trauma are also at risk for intra-abdominal organ injury. A 2017 article published in the American Journal of Surgery found that 77% of the patients with liver lacerations and 79% of patients with splenic lacerations had overlying fractures of the lower ribs.[23] As such, a thorough abdominal exam is a critical aspect of the physical exam after blunt chest injury. Begin with inspection for bruising (ie, seatbelt sign) or distention. Abdominal seatbelt sign is an even more ominous finding than chest seatbelt sign and has been found to be associated with an eight-fold higher likelihood of intra-abdominal injury.19 Palpate the abdomen for focal tenderness and signs of peritonitis (eg, rebound tenderness or guarding). Patients with significant abdominal tenderness and/or bruising from a seatbelt injury should be referred to the ED as they have a high likelihood of requiring surgical intervention.[24]
Imaging
Plain Radiography
When there is clinical suspicion for rib fractures, an upright CXR is the most critical initial study.1 While a single or 2-view CXR is only 50% sensitive for the diagnosis of a single rib fracture, definitive identification of rib fractures rarely affects management. In fact, in a 2021 study reviewing over 1,700 patients who underwent rib series radiography, there were no cases of changes in any patient’s management related to findings of dedicated rib films.[25] Similarly, a recent study of over 400 trauma patients who underwent both CXR and rib x-ray series found that the addition of the rib radiographs changed management in only 1 patient (0.2%).[26] The dramatic and reproducible evidence of rib series’ lack of impact on patient management provides the evidential support for the American College of Radiology (ACR) Appropriateness Criteria guidelines on blunt chest injury which do not recommend obtaining dedicated radiographs rib series after blunt chest injury.1
The ACR guidelines for the initial imaging study after blunt chest injury instead strongly support the utility of a standard CXR as a screening tool for complications of chest wall injury, such as PTX, HTX, and pulmonary contusion.1 This recommendation is based on the test characteristics of standard CXR, which has a greater sensitivity for the injuries that affect management; CXR also has significantly less ionizing radiation when compared to that of a rib series.1 Although the diagnosis of multiple rib fractures has certain prognostic implications, there is no evidence that performing dedicated rib studies affects patient outcomes.
When assessing the CXR, evaluate for signs of rib fractures. Fractures may appear as a discontinuity in the bone’s cortices and/or disruption in the trabecular pattern. Examine for evidence of serious complications. PTX can be identified as an area of lucency without pulmonary markings and the presence of a pleural line separated from the thoracic wall. Upright films are more sensitive than supine films for PTX identification as the intrapleural air will tend to move cephalad and be detectable in the superior most portion of the affected hemithorax.[27] The sensitivity of upright CXR for detection of PTX is approximately 70%.[28] Tension PTX occurs when air trapped in the pleural space exerts sufficient pressure to impair cardiac venous return. Tension PTX is a clinical diagnosis and should be suspected in patients with evidence of significant PTX, hypoxemia and/or hypotension.[29] Immediate treatment for tension PTX consists of EMS activation and needle decompression of the hemithorax.[30]
Similarly, HTX can be identified as a pleural effusion, and gravity effects will make this most apparent in an upright film. CXR is approximately 63% sensitive for identification of HTX.28 Pulmonary contusions may be delayed in their radiographic appearance and appear as air space opacities. A widened mediastinum should prompt consideration for blunt aortic injury.[31] Importantly, with these sensitivities, a normal CXR is far from adequate in excluding complications of blunt chest injury in patients in whom there is high clinical pre-test probability of significant injury (ie, severe pain, abnormal vital signs, high energy mechanism of injury).27
Special consideration is warranted for patients with first or second rib fractures as these patients have a high risk of concomitant great vessel injuries.2 In pediatric patients, costochondral junction fractures are highly specific for NAT, but CXR is not sufficiently sensitivity to exclude thoracic NAT in cases of high clinical suspicion.[32]
Point-of-Care Ultrasound
Point-of-care ultrasound (POCUS) has gained increasingly wide adoption in recent decades as a useful adjunct to the bedside assessment of trauma patients. With appropriate equipment and training, POCUS is an ideal tool for screening assessment of trauma patients.[33] There is little published data on the prevalence of POCUS use in UC centers. However, given the increasing affordability and portability of POCUS devices, it is reasonable to expect that equipping UC clinicians with such technology and appropriate training would have a meaningful impact on resource utilization and patient outcomes. Additionally, in the hands of experienced clinicians, POCUS has superior sensitivity to CXR for both PTX (85% vs. 71%) and HTX (79% vs. 63%).28 POCUS also has superior sensitivity to CXR (85% vs. 56%) for the detection of rib fractures, especially in cases where multiple rib fractures are present.[34],[35]
Computed Tomography
While not commonly available in the UC setting, chest computed tomography (CT) is the gold standard for both identification of rib fractures and associated intra-thoracic injuries related to blunt chest trauma.1,[36] While chest CT is much more sensitive for rib fractures and other post-traumatic complications, the majority of UC patients with blunt chest injury do not require chest CT. The NEXUS Chest CT Rule was derived and validated to help clinicians determine which patients with blunt chest injury are likely to have findings on chest CT that affect management. The rule is >99% sensitive excluding serious intrathoracic injury if a patient has a normal CXR and has no distracting injury, chest wall tenderness, or high-risk mechanism of injury.[37] Given many patients will have some degree of bony chest tenderness, however, this rule unfortunately cannot be used in many patients and is poorly specific. However, emergency physician gestalt has also proven highly reliable for excluding clinically significant injuries that might only be diagnosed on chest CT.[38] Unfortunately, there are no studies on the efficacy of UC clinician gestalt in ruling out significant intrathoracic injury. Patients presenting to UC, however, are typically much lower acuity/risk than patients with similar complaints in an ED setting. Given this set of circumstances and until more evidence is available, it seems most reasonable for UC clinicians to use a combination of clinical judgment and CXR findings to determine who will benefit from thoracic CT imaging. Unless immediate CT is available, such patients warrant ED referral.
Urgent Care Management of Rib Fractures
Management of rib fractures in UC includes: risk stratification for complications; assessment of respiratory status; appropriate pharmacologic and non-pharmacologic interventions to ensure pain is adequately managed; and measures to reduce subsequent complications.
Indications for immediate ED referral include the following:
- Evidence of (or suspicion for) associated pneumothorax, hemothorax, hypoxemia, tracheobronchial injury, injury to the great vessels, intraabdominal injury, flail chest, and/or sternal fracture
- Hypoxemia (O2 saturation <92% on room air)
- Intractable pain
- Significant hypotension or tachycardia
Suggested discretionary criteria include:
- Elderly patients (>65 years) and those with suspected barriers to adequate pain control
- 3 or more rib fractures or displaced fractures
- Decreased pulmonary function, such as chronic obstructive pulmonary disease (COPD) or other comorbid conditions (eg, sleep apnea, obesity hypoventilation syndrome, alcohol use disorder) that predispose patients at risk for respiratory failure.
As the rib cage is necessarily moving continuously to support adequate respirations, the pain associated with rib fractures can be severe and pervasive. The Western Trauma Association guidelines for care of patients after sustaining rib fractures recommend providing appropriate pain management, encouraging frequent pulmonary hygiene exercises, such as coughing, deep breathing, and avoiding prolonged sitting or bedrest with frequent ambulation.[39]
Non-Pharmacologic Intervention
Splinting devices, such as rib belts, have not been shown to reduce pain and may decrease lung excursion, thereby increasing the risk of subacute complications (eg, atelectasis, pneumonia).15 Pulmonary toilet (or pulmonary hygiene) describes practices that encourage maximal diaphragmatic excursion; common pulmonary toilet/hygiene practices include coughing and deep breathing exercises. Incentive spirometry devices, traditionally felt to improve outcomes after rib fractures, have not been shown to reduce complications.[40] However, early mobilization and frequent ambulation have proven very effective in reducing morbidity and subacute complications after rib fractures.[41]
Respiratory rate has not proven effective as a means of predicting respiratory failure after rib fracture.[42] However, patients with fractured ribs who cannot achieve incentive spirometry (IS) volumes >1,000 mL have been found to have a higher likelihood of respiratory failure. Therefore, while of questionable utility for pulmonary hygiene, IS may serve some clinical utility for the determination of need for ED referral.[43],[44]
Pharmacologic Interventions
Pain control should be individualized for patients with chest wall injury. The goals of pain management should to alleviate pain, rather than expect it can be eliminated entirely.[45] Pain management is especially critical after chest trauma to allow for deep breathing, coughing, and ambulation, which may decrease the risk of splinting and pneumonia.41
As with the treatment of any source of acute traumatic pain, the risks and benefits of medications should be carefully weighed. Opioid analgesics, while highly effective for the treatment of acute fracture-related pain, are associated with respiratory depression at highly variable doses based on many patient factors.[46] Therefore, it is important that opioids are used sparingly and not as a sole class of analgesics. Increasingly, multimodal analgesia approaches have gained evidential support, including as they pertain to rib fractures.[47]
Stepwise use of oral analgesics in a multimodal approach can minimize opioid requirements in patients with acute pain. Oral acetaminophen (paracetamol) at the maximum daily dose accompanied by appropriate dosing of non-steroidal anti-inflammatory agents (eg, ibuprofen, naproxen) as first and second-line agents with opioids reserved for breakthrough pain is a sensible analgesic strategy.[48],[49] Early administration of parenteral NSAIDs has been shown to decrease opioid requirements, length of stay, pneumonia incidence, number of ventilator days, and intensive care length of stay.[50]
Topical pharmacotherapy should not be overlooked as well. Topical NSAIDs (eg, diclofenac) can be used in patients who cannot safely take oral NSAIDs. Additionally, lidocaine patches have an excellent safety profile and have been shown to reduce opioid requirements in patients with acute rib fractures.[51] With these considerations for first and second-line agents, it is important to note that in most patients discharged from UC, several days of opioid therapy for breakthrough pain is generally appropriate.48
Considerations For Follow-Up
For patients discharged from UC after rib fracture, ensuring close follow-up and clear return precautions is essential. Worsening shortness of breath and/or fever, for example, could indicate the presence of pneumonia. These precautions should be emphasized most in patients with underlying lung disease (eg, asthma, COPD) as they are at the highest risk of developing pneumonia after chest trauma.[52]
When 3 or more rib fractures are present, there is an increased morbidity and mortality, particularly among patients >65 years of age or displaced fractures.11,[53],[54] Poor functional status, regardless of age, is also a strong predictor of complications.[55] UC clinicians should have a low threshold for referring such patients immediately to the ED.
Next Level Urgent Care Pearls
Increasingly, regional anesthesia techniques have been found to offer significant pain relief for patients with acute rib fractures. These techniques require appropriate training and equipment (ie, POCUS). An intercostal nerve block with the use of a long-acting anesthetic has been shown to provide up to 12 hours of analgesia, however, can result in PTX or HTX as potential.[56] The serratus anterior and erector spinae plane blocks have also proven effective for providing immediate and significant reductions in pain scores in patients with rib fractures. With appropriate training and equipment, these regional anesthetic approaches could be offered to provides safe and effective adjunctive pain relief and reduce the risk of hospitalization and/or intensive care unit admission.[57],[58],[59]
Red Flags and Legal Pitfalls
- Patients at the highest risk of significant morbidity and mortality are elderly patients (age >65 years) and patients with multiple rib fractures.
- The initial evaluation in a patient with suspected rib fracture(s) is to assess for life-threatening injuries such as pneumothorax, hemothorax, flail chest, or great vessel injury.
- Injury to the 1st and 2nd ribs are generally the result of a large amount of force, with consideration of great vessel as well as bronchial injury.1
- Injury to the lower ribs may be associated with intra-abdominal injury.
- A child with multiple rib fractures or rib fractures at different stages of healing is concerning for NAT.
- The most common reason for return visits after rib fractures is pain, so ensuring adequate pain control before discharge is vital to prevent them from returning.[60]
Clinical Scenario Conclusion
In addition to multiple rib fractures, a the right-sided PTX was also identified on the upright CXR. Because of the multiple fractures as well as PTX, the patient was sent to the ED via EMS as he did not have anyone to drive him and was felt to be in too severe of pain to drive. In the ED, he underwent chest CT which showed no HTX but redemonstrated a PTX and multiple rib fractures. He had a small gauge chest tube placed in the ED and was admitted to the trauma service for analgesic titration and monitoring.
For a similar patient without PTX or multiple rib fractures who might be discharged from the UC, an example of an appropriate outpatient plan would be oral acetaminophen 1000mg and NSAID (ibuprofen or naproxen) with a topical lidocaine patch (4%, over-the-counter) over the areas of pain as initial multimodal analgesic treatment. In addition, consider a prescription for 3-4 days of oxycodone 2.5-5mg every 4 hours as needed for breakthrough pain.
Additional instructions for pulmonary hygiene to be given at discharge could include coughing and deep breathing exercises and ambulation at least twice an hour to decrease the risk of atelectasis and pneumonia. Such discharged patients should be instructed to have follow up with primary care in 3-7 days and given strict return precautions for fever, increasing pain, shortness of breath, or lightheadedness.
Takeaway Points
- Rib fractures can occur after blunt thoracic trauma, most commonly MVCs and falls.
- There is little necessity in identifying rib fractures; the management of chest wall contusions is not affected by whether rib fractures are present.
- Avoid the cognitive trap of excessive focus on identification of rib fractures. Instead, ensure adequate evaluation for other areas of injury and possible complications of blunt thoracic trauma such as PTX and HTX.
- Do not order rib radiograph films as they do not affect the management of patients with blunt chest trauma.
- While CXR is the initial recommended study of choice for blunt chest injury, with appropriate training POCUS is more sensitive for identification of PTX and HTX.
- Patients at the highest risk for complications after rib fracture include the elderly (>65 years), those with multiple rib fractures, and/or underlying pulmonary disease.
- Pulmonary toilet, multimodal analgesia (including topical agents), and close follow-up are the key components of outpatient management for reducing the risk of complications.
Manuscript submitted November 23, 2024; accepted December 10, 2024.
References
- [1]. Henry TS, Donnelly EF, et al. Expert Panel on Thoracic Imaging. ACR Appropriateness Criteria Rib Fractures. J Am Coll Radiol. 2019;16(5S):S227-S234.
- [2]. Murphy CE, Raja AS, Baumann BM, et al. Rib Fracture Diagnosis in the Panscan Era. Ann Emerg Med. 2017;70(6):904-909.
- [3]. Tignanelli CJ, Rix A, Napolitano LM, Hemmila MR, Ma S, Kummerfeld E. Association Between Adherence to Evidence-Based Practices for Treatment of Patients with Traumatic Rib Fractures and Mortality Rates Among US Trauma Centers. JAMA Netw Open. 2020 Mar 2;3(3):e201316.
- [4]. Peek J, Ochen Y, Saillant N, et al. Traumatic rib fractures: a marker of severe injury. A nationwide study using the National Trauma Data Bank. Trauma Surg Acute Care Open. 2020;5(1):e000441. Published 2020 Jun 10.
- [5]. Hamilton C, Barnett L, Trop A, et al. Emergency department management of patients with rib fracture based on a clinical practice guideline. Trauma Surg Acute Care Open. 2017;2(1):e000133. Published 2017 Dec 22.
- [6]. Sirmali M, Türüt H, Topçu S, Gülhan E, Yazici Ü, Kaya S, Taştepe İ. A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eur J Cardiothorac Surg. 2003;24(1):133-138.
- [7]. Senekjian L, Nirula R. Rib Fracture Fixation: Indications and Outcomes. Crit Care Clin. 2017;33(1):153-165.
- [8]. Pieracci FM, Leasia K, Bauman Z, Eriksson EA, Lottenberg L, Majercik S, Powell L, Sarani B, Semon G, Thomas B, Zhao F, Dyke C, Doben AR. A multicenter, prospective, controlled clinical trial of surgical stabilization of rib fractures in patients with severe, nonflail fracture patterns (Chest Wall Injury Society NONFLAIL). J Trauma Acute Care Surg. 2020 Feb;88(2):249-257.
- [9]. Sammy IA, Chatha H, Lecky F, et al. Are first rib fractures a marker for other life-threatening injuries in patients with major trauma? A cohort study of patients on the UK Trauma Audit and Research Network database. Emerg Med J. 2017;34(4):205-211.
- [10]. Dennis BM, Bellister SA, Guillamondegui OD. Thoracic Trauma. Surg Clin North Am. 2017 Oct;97(5):1047-1064.
- [11]. Battle C, Carter K, Newey L, Giamello JD, Melchio R, Hutchings H. Risk factors that predict mortality in patients with blunt chest wall trauma: an updated systematic review and meta-analysis. Emerg Med J. 2023;40(5):369-378.
- [12]. Kocjan J, Adamek M, Gzik-Zroska B, Czyżewski D, Rydel M. Network of breathing. Multifunctional role of the diaphragm: a review. Adv Respir Med. 2017;85(4):224-232. doi:10.5603/ARM.2017.0037
- [13]. Petrone P, Asensio JA, Marini CP. Diaphragmatic injuries and post-traumatic diaphragmatic hernias. Curr Probl Surg. 2017 Jan;54(1):11-32.
- [14]. Mulpuri K, Slobogean BL, Tredwell SJ. The epidemiology of nonaccidental trauma in children. Clin Orthop Relat Res. 2011 Mar;469(3):759-67.
- [15]. Rogers FB, Larson NJ, Rhone A, Amaya D, Olson-Bullis BA, Blondeau BX. Comprehensive Review of Current Pain Management in Rib Fractures with Practical Guidelines for Clinicians. J Intensive Care Med. 2023 Apr;38(4):327-339.
- [16]. Katrancioglu O, Akkas Y, Arslan S, Sahin E. Spontaneous rib fractures. Asian Cardiovasc Thorac Ann. 2015 Jul;23(6):701-3.
- [17]. Evans G, Redgrave A. Great Britain Rowing Team Guideline for diagnosis and management of rib stress injury: Part 1. Br J Sports Med. 2016;50(5):266-269.
- [18]. Funakoshi T, Furushima K, Kusano H, et al. First-Rib Stress Fracture in Overhead Throwing Athletes. J Bone Joint Surg Am. 2019;101(10):896-903.
- [19]. Velmahos GC, Tatevossian R, Demetriades D. The “seat belt mark” sign: a call for increased vigilance among physicians treating victims of motor vehicle accidents. Am Surg. 1999;65(2):181-185.
- [20]. Peters ML, Starling SP, Barnes-Eley ML, Heisler KW. The presence of bruising associated with fractures. Arch Pediatr Adolesc Med. 2008 Sep;162(9):877-81.
- [21]. Crandall J, Kent R, Patrie J, Fertile J, Martin P. Rib fracture patterns and radiologic detection–a restraint-based comparison. Annu Proc Assoc Adv Automot Med. 2000;44:235-259.
- [22]. Chen SC, Markmann JF, Kauder DR, Schwab CW. Hemopneumothorax missed by auscultation in penetrating chest injury. J Trauma. 1997;42(1):86-89. doi:10.1097/00005373-199701000-00015
- [23]. Rostas JW, Lively TB, Brevard SB, Simmons JD, Frotan MA, Gonzalez RP. Rib fractures and their association with solid organ injury: higher rib fractures have greater significance for solid organ injury screening. Am J Surg. 2017 Apr;213(4):791-797.
- [24]. Biswas S, Adileh M, Almogy G, Bala M. Abdominal injury patterns in patients with seatbelt signs requiring laparotomy. J Emerg Trauma Shock. 2014;7(4):295-300.
- [25]. Nishimura E, Finger A, Harris M, Yoon HC. One-View Chest Radiograph for Initial Management of Most Ambulatory Patients with Rib Pain. J Am Board Fam Med. 2021;34(1):144-150. doi:10.3122/jabfm.2021.01.200276
- [26]. Shuaib W, Vijayasarathi A, Tiwana MH, Johnson JO, Maddu KK, Khosa F. The diagnostic utility of rib series in assessing rib fractures. Emerg Radiol. 2014 Apr;21(2):159-64.
- [27]. Mowery N, et al. Practice Management Guidelines for Management of Hemothorax and Occult Pneumothorax. Journal of Trauma: Injury, Infection, and Critical Care. 70(2):p 510-518, February 2011. doi: 10.1097/TA.0b013e31820b5c31
- [28]. Aswin K, et al.Comparing Sensitivity and Specificity of Ultrasonography With Chest Radiography in Detecting Pneumothorax and Hemothorax in Chest Trauma Patients: A Cross-Sectional Diagnostic Study. Cureus. 2023;15(8):e44456. Published 2023 Aug 31. doi:10.7759/cureus.44456
- [29]. Roberts DJ, Leigh-Smith S, Faris PD, et al. Clinical Presentation of Patients With Tension Pneumothorax: A Systematic Review. Ann Surg. 2015;261(6):1068-1078. doi:10.1097/SLA.0000000000001073
- [30]. Gurney D. Tension Pneumothorax: What Is an Effective Treatment?. J Emerg Nurs. 2019;45(5):584-587. doi:10.1016/j.jen.2019.06.003
- [31]. Bhavnagri SJ, Mohammed TL. When and how to image a suspected broken rib. Cleve Clin J Med. 2009;76(5):309-314.
- [32]. Forbes-Amrhein MM, Gensel AJ, Cooper ML, Karmazyn B. Multi-modality imaging characteristics of costochondral fractures, a highly specific rib fracture for child abuse. Pediatr Radiol. 2022 May;52(5):910-923.
- [33]. Hansen W, Mitchell CE, Bhattarai B, Ayutyanont N, Stowell JR. Perception of point-of-care ultrasound performed by emergency medicine physicians. J Clin Ultrasound. 2017;45(7):408-415. doi:10.1002/jcu.22443
- [34]. Awais M, Salam B, Nadeem N, Rehman A, Baloch NU. Diagnostic Accuracy of Computed Tomography Scout Film and Chest X-ray for Detection of Rib Fractures in Patients with Chest Trauma: A Cross-sectional Study. Cureus. 2019;11(1):e3875. Published 2019 Jan 13. doi:10.7759/cureus.3875
- [35]. Zarei Jelyani N, Mousavi-Roknabadi R S, Mohammadi R, Hosseini-Marvast S R, Goudarzi F, et al. Diagnosis of Rib Fracture and Related Complications in Patients with Blunt Chest Wall Trauma Using Point-of-Care Ultrasound vs. Computed Tomography Scan. Shiraz E-Med J. 2023;24(11):e138379
- [36]. Oikonomou A, Prassopoulos P. CT imaging of blunt chest trauma. Insights Imaging. 2011;2(3):281-295. doi:10.1007/s13244-011-0072-9
- [37]. Rodriguez RM, Langdorf MI, Nishijima D, Baumann BM, Hendey GW, Medak AJ, Raja AS, Allen IE, Mower WR. Derivation and validation of two decision instruments for selective chest CT in blunt trauma: a multicenter prospective observational study (NEXUS Chest CT). PLoS Med. 2015 Oct 6;12(10):e1001883. doi: 10.1371/journal.pmed.1001883. eCollection 2015.
- [38]. Smith CB, Barrett TW, Berger CL, Zhou C, Thurman RJ, Wrenn KD. Prediction of blunt traumatic injury in high-acuity patients: bedside examination vs computed tomography. Am J Emerg Med. 2011;29(1):1-10.
- [39]. Brasel KJ, Moore EE, Albrecht RA, deMoya M, Schreiber M, Karmy-Jones R, Rowell S, Namias N, Cohen M, Shatz DV, Biffl WL. Western Trauma Association Critical Decisions in Trauma: Management of rib fractures. J Trauma Acute Care Surg. 2017 Jan;82(1):200-203.
- [40]. Dote H, Homma Y, Sakuraya M, Funakoshi H, Tanaka S, Atsumi T. Incentive spirometry to prevent pulmonary complications after chest trauma: a retrospective observational study. Acute Med Surg. 2020;7(1):e619. Published 2020 Dec 31. doi:10.1002/ams2.619
- [41]. Weinberg BJ, Roos R, van Aswegen H. Effectiveness of nonpharmacological therapeutic interventions on pain and physical function in adults with rib fractures during acute care: A systematic review and meta-analysis. S Afr J Physiother. 2022;78(1):1764. Published 2022 Jun 28.
- [42]. Butts CA, Brady JJ 3rd, Wilhelm S, et al. Do simple beside lung function tests predict morbidity after rib fractures? Am J Surg. 2017;213(3):473-477. doi:10.1016/j.amjsurg.2016.11.026
- [43]. Carver TW, Milia DJ, Somberg C, Brasel K, Paul J. Vital capacity helps predict pulmonary complications after rib fractures. J Trauma Acute Care Surg. 2015;79(3):413-416.
- [44]. Warner R, Knollinger P, Hobbs G, Lilly C, Grabo D, Wilson A. Forced vital capacity less than 1: A mark for high-risk patients. J Trauma Acute Care Surg. 2018;85(2):271-274.
- [45]. Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain-United States, 2022. MMWR Recomm Rep 2022;71(No. RR-3):1–95.
- [46]. Nadpara PA, Joyce AR, Murrelle EL, Carroll NW, Carroll NV, Barnard M, Zedler BK. Risk factors for serious prescription opioid-induced respiratory depression or overdose: comparison of commercially insured and Veterans Health Affairs populations. Pain Med. 2018;19(1):79-96.
- [47]. Burton SW, Riojas C, Gesin G, et al. Multimodal analgesia reduces opioid requirements in trauma patients with rib fractures. J Trauma Acute Care Surg. 2022;92(3):588-596. doi:10.1097/TA.0000000000003486
- [48]. Amaechi O, Mccann Human M, Featherstone K. Pharmacologic therapy for acute pain; Am Fam Physician. 2021;104(1):63-72
- [49]. Van Zyl T, Ho AM, Klar G, et al. Analgesia for rib fractures: a narrative review. Analgésie pour les fractures des côtes : une revue narrative. Can J Anaesth. 2024;71(4):535-547. doi:10.1007/s12630-024-02725-1
- [50]. Martin TJ, Eltorai AS, Dunn R, Varone A, Joyce MF, Kheirbek T, Adams C Jr, Daniels AH, Eltorai AEM. Clinical management of rib fractures and methods for prevention of pulmonary complications: A review. Injury. 2019 Jun;50(6):1159-1165.
- [51]. Johnson M, Strait L, Ata A, et al. Do Lidocaine Patches Reduce Opioid Use in Acute Rib Fractures? Am Surg. 2020;86(9):1153-1158. doi:10.1177/0003134820945224
- [52]. Chauny JM, et al. Patients with rib fractures do not develop delayed pneumonia: a prospective, multicenter cohort study of minor thoracic injury. Ann Emerg Med 60(6):726, December 2012.
- [53]. Shi HH, Esquivel M, Staudenmayer KL, Spain DA. Effects of mechanism of injury and patient age on outcomes in geriatric rib fracture patients. Trauma Surg Acute Care Open. 2017 Mar 16;2(1):e000074.
- [54]. Chien CY, Chen YH, Han ST, Blaney GN, Huang TS, Chen KF. The number of displaced rib fractures is more predictive for complications in chest trauma patients. Scand J Trauma Resusc Emerg Med. 2017;25(1):19. Published 2017 Feb 28.
- [55]. Leichtle SW, Pendleton A, Wang S, Torres B, Collins R, Aboutanos MB. Triage of Patients With Rib Fractures : Patient’s Age and Number Don’t Tell the Whole Story. Am Surg. 2020;86(9):1194-1199.
- [56]. Witt C, Bulger E. Comprehensive approach to the management of the patient with multiple rib fractures: a review and introduction of a bundled rib fracture management protocol. Trauma Surgery & Acute Care Open. 2017;2:e000064.
- [57]. Hwang EG, Lee Y. Effectiveness of intercostal nerve block for management of pain in rib fracture patients. J Exerc Rehabil. 2014 Aug 31;10(4):241-4.
- [58]. Kring RM, Mackenzie DC, Wilson CN, Rappold JF, Strout TD, Croft PE. Ultrasound-Guided Serratus Anterior Plane Block (SAPB) Improves Pain Control in Patients With Rib Fractures. J Ultrasound Med. 2022;41(11):2695-2701.
- [59]. Schnekenburger M, Mathew J, Fitzgerald M, Hendel S, Sekandarzad MW, Mitra B. Regional anaesthesia for rib fractures: A pilot study of serratus anterior plane block. Emerg Med Australas. 2021;33(5):788-793.
- [60]. Armin E, Movahedi M, Najafzadeh MJ, Honarmand A, Rukerd MRZ, Mirafzal A. Comparison Of Ultrasound-Guided Erector Spinae Plane Block With Intercostal Nerve Block For Trauma-Associated Chest Wall Pain. J Emerg Med. 2022;63(4):520-527.
Author Affiliations: Dustin M. Nelson, BS, Lincoln-Memorial University in Knoxville, Tennessee. Shering Torres, MAS, MD, Department of Emergency Medicine, The Ohio State University in Columbus, Ohio. Michael Weinstock, MD, Department of Emergency Medicine, Adena Health System and Department of Emergency Medicine, The Wexner Medical Center, at The Ohio State University, Chillicothe, Ohio. Authors have no relevant financial relationships with any ineligible companies.
Download the Article PDF: Urgent Care Considerations for the Patient with Suspected Rib Fracture

