Published on
Urgent Message: Fractures of the midshaft ulna, commonly referred to as “nightstick fractures,” typically occur after direct injury to a forearm outstretched above the head as a protective mechanism. Evaluation includes inquiry into the circumstances of the assault, assessment for any other areas of trauma, examination of the skin, wrist and elbow joints, and radiography of the forearm. Management of closed, nondisplaced midshaft ulnar fractures centers around splint immobilization and arrangement of appropriate follow-up.
Chandrika Janumpalli, BS; William Bradley Strauch, MD
Citation: Janumpalli C, Strauch WB. Urgent Care Diagnosis and Management of Midshaft Ulnar (Nightstick) Fractures. J Urgent Care Med. 2024; 19 (3); 23-27
Questions for the Clinician at the Bedside
- What defines a nightstick fracture?
- When should a nightstick fracture be suspected?
- What other considerations are important when a nightstick fracture is identified based on common mechanisms of injury?
- What physical exam findings are suggestive of nightstick or other types of ulnar fracture?
- When is same-day closed reduction appropriate and which cases are more likely to require emergency department referral and immediate surgical fixation?
Clinical Scenario
A healthy, left hand dominant, 14-year-old girl presented to the urgent care (UC) complaining of left forearm pain that started the previous evening after a reported fall. The pain was worsened with movement. She denied any numbness in the hand, wrist, or elbow or any other injuries.
On physical examination, she winced with passive movement of the left arm. There was mild swelling and ecchymoses over the midforearm on the ulnar aspect. There was moderate to severe pain on palpation to this area of bruising and swelling. There were no abrasions, lacerations, or other skin defects. She had no pain with palpation over the left wrist or elbow and the left arm was neurovascularly intact with normal sensation and movement of the hand and fingers as well as strong radial and ulnar pulses.
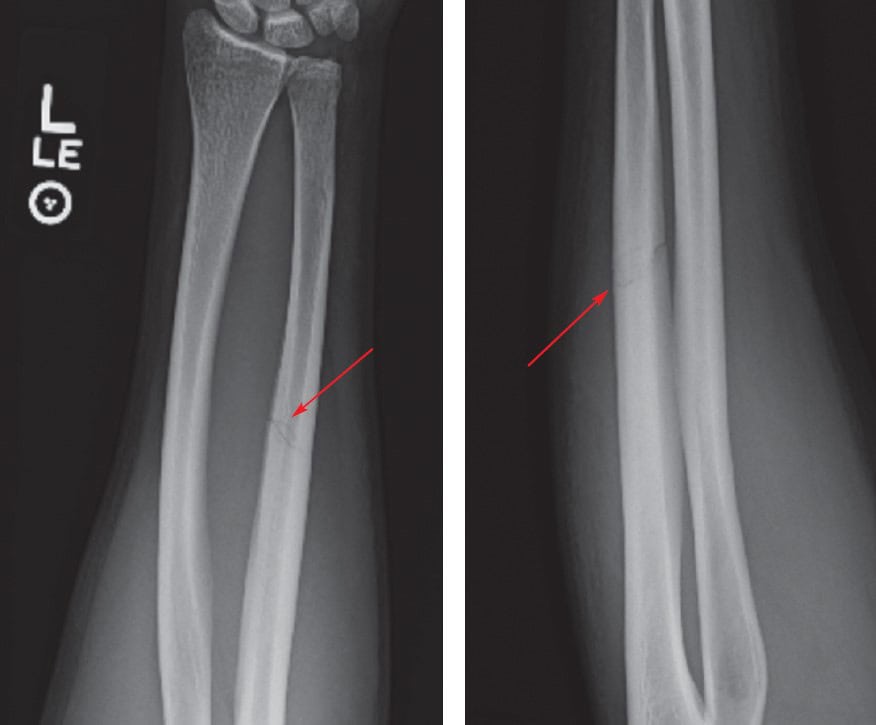
X-rays (XR) of the forearm were obtained revealing a midshaft ulnar fracture (Image 1-2).
Discussion
Isolated midshaft ulnar shaft fractures are commonly called “nightstick fractures” because historically such fractures were associated with a self-defense reaction to bludgeoning from a truncheon (or nightstick) with an outstretched forearm.[1] Midforearm fractures (not isolated specifically to the midshaft of the ulna) are the third most common type of long bone fracture in children,[2] whereas the forearm is generally the most common site of all pediatric fractures and comprises 17% of fractures in children.[3]
Relevant Forearm Anatomy
The forearm consists of the radius and ulna. Rotation of these bones produces supination and pronation of the hand. The ulna forms an important component of the elbow joint and forms 2 of the 3 main points of articulation that allow for elbow stability: the ulnar-humeral joint and the proximal radio-ulnar joint. It is a component of the wrist joint proximally along with 8 carpal bones and distal radius. The proximal and distal articulation of the ulna are important to evaluate on physical examination to associated injuries beyond nightstick fractures.
Clinical History
Midshaft ulnar fractures commonly occur when the forearm is stretched above the head as a defense mechanism and sustains a direct blow.[4] As this injury pattern is suggestive of self-defense, it is important to explore the potential of assault or abuse and inquire about other areas of pain which may indicate associated injuries occurred during an assault.
Self-defense against assault, while common, is not the only potential mechanism for nightstick fractures. A 2015 case series of 70 consecutive nightstick fractures found that 57% of midshaft ulnar fractures in adults occurred after motor vehicle accidents (MVA). Falls (13%) were the next most common mechanism, and direct impact comprised only 11% of cases.[5] Little information regarding the etiology of pediatric isolated midshaft ulnar fractures is available in literature, perhaps due to the rarity. One epidemiological study in the United Kingdom found combined ulna-radius midshaft fractures (not isolated midshaft ulnar) in children under 16 to make up about 5% of all pediatric fractures, with a fall onto a hand stretched outward being the most common etiology.[6]
It is important to inquire about pain either proximal or distal to the ulna to determine likelihood of fracture or dislocation of the elbow or wrist. Inquire with nonjudgmental and open-ended inquiry about the possibility of nonaccidental trauma (NAT), altercation, or intimate partner violence. Additional history gathering should screen for symptoms such as paresthesia or pain out of proportion, which could indicate neurovascular injury or compartment syndrome.
Physical Examination
Perform a standard and stepwise physical exam of the extremity including: inspection, palpation, range of motion (ROM) of the joint proximal and distal, and a neurovascular assessment.
Inspection focuses on examination of the skin for erythema, swelling, lacerations or other skin defects, or ecchymoses. Palpate beginning with the distal extremity (ie, finger and hands) far from area of greatest pain and gradually move toward the area where expected pain would be greatest (ie, the ulnar metaphysis). ROM testing should include active assessment of the movements of the elbow and wrist to determine points of maximum tolerable flexion, extension, supination, pronation, and radial/ulnar deviation. Finally, evaluate neurovascular status including pulses and distal sensation. In the forearm, the ulnar nerve and artery run superficial to the ulna and deep to the flexor carpi ulnaris, but if the pain includes more distal or proximal areas, then it is recommended to assess the radial pulse as well.
Imaging
To evaluate for suspected midshaft ulnar fractures in the UC setting a 3-view XR of the forearm is recommended. Additionally, 3 views of the wrist and/or elbow are recommended if significant pain or tenderness extends to these areas. While the wrist and elbow may be visible in a forearm series, distortion occurs with radiographs as the distance from the center point, or “central ray,” increases. Therefore, both the wrist and elbow joint are suboptimally resolved on forearm radiographs.[7] The preferred views for the standard forearm series are lateral, anteroposterior (AP), and oblique.
Management in Urgent Care
UC management of midshaft ulnar fractures includes proper immobilization with a rigid splint and appropriate analgesia. Early mobilization is increasingly preferred, however, it is prudent to treat conservatively in the absences of real-time orthopedic consultation from UC. Orthopedic specialist follow-up should be arranged within 5-7 days.
Splinting to immobilize the forearm should ensure that supination and pronation of the wrist are restricted. This can be achieved with any of the following methods:
- Modified ulnar gutter slab and sling: This splint allows for immobilization of forearm pronation and supination as well as wrist flexion and extension while leaving elbow flexion and extension intact.[8] Preserving elbow motion helps patients maintain activities of daily living.
- Sugar tong splint: This splint is similar to the ulnar gutter slab, however because elbow flexion and extension are also immobilized, there is risk of elbow stiffness and loss of ROM.8
- Prefabricated or fashioned Muenster orthosis: This splint/brace is similar to the sugar tong splint but allows for elbow flexion and extension while immobilizing forearm pronation and supination.[9]
Analgesia should be individualized for the patient and their pain severity. The World Health Organization Analgesic Ladder is a reasonable paradigm to use for pain associated with nightstick fractures as it emphasizes sequentially using agents beginning with the safest options.[10] Common oral agents such as acetaminophen and non-steroidal anti-inflammatory drugs can be used alone or in combination. A short duration of opioids may be appropriate based in cases of more severe pain. Non-pharmacologic agents include appropriate immobilization and splint fitting, elevation to reduce swelling, and applying ice to the midulna.
When to Mobilize
To evaluate the practice of early mobilization, Cai et al performed a systematic review of 27 studies with over 1,600 patients with nightstick fractures and found that those managed non-operatively with early mobilization had shorter time to fracture union and lower rates of non-union compared to patients with traditional immobilization.1 Based on the findings of the review, the authors recommend starting with a below-elbow brace (which as described above could include the modified ulnar gutter slab and sling) for 1-2 weeks before implementing mobilization, however, they do recognize the need for prospective, randomized controlled trials before this can confidently be adopted as a standard of care.1
Considerations For Surgical Treatment
A 2008 retrospective case-control study by Coulibaly et al compared outcomes among 70 adults with nightstick fracture after non-operative treatment compared to operative internal fixation (ORIF). In this study, the investigators found that older age, female gender and noncompliance with weight-bearing restrictions were associated with anatomical nonunion or malunion after non-operative treatment, however functional recovery was similar in both treatment groups.5 Similarly, a 2017 prospective randomized controlled trial by Hussain et al, assigned patients to non-operative treatment (immobilization with above elbow cast for 6 weeks) or ORIF with intramedullary nails or plates and found no effect of age or gender on functional outcomes. However, there was a significantly shorter time to union (13 vs. 18 weeks) in the surgical treatment group.[11] Therefore, in clinical practice, surgical decision making for a nightstick fracture may take into account age and gender of the patient for prevention of anatomical complications.
Necessity of Closed Reduction
Understanding the degree of displacement and/or angulation that is acceptable for various fracture patterns is important for UC clinicians because inadequate initial reductions may increase the need for surgery and adversely affect long-term outcomes.[12] Recommendations for midshaft ulnar fractures suggest that angulation >10 degrees in children >10 years of age can impede forearm rotation, however, in younger patients, up to 20 degrees of angulation and 1cm of shortening is acceptable.[13]
In adults, there is currently no literature supporting necessity of closed reduction of nightstick fractures. Although the prospective study by Hussain et al involved closed reduction of the fracture to less than 50% displacement before applying an above elbow cast, there was not a comparison group with application of cast without reduction, and this study was limited by a small sample size of 30 subjects. Additionally, this study included subjects who presented with the nightstick fracture within 2 weeks of injury, so even if the fracture was initially fixed with closed reduction, immediate timing was not prioritized.11 Though there are multiple studies that discuss hematoma block to address pain before conducting closed reduction of distal radial fractures and traction as a method to facilitate closed reduction of distal radial fractures, there is no literature supporting effectiveness in the case of a nightstick fracture.12,[14]
Considerations for Emergency Department Referral
Indications for immediate emergency department (ED) referral for urgent orthopedic surgery consultation of midshaft ulnar fractures include the following:11,[15]
- Concerns for possible open fracture
- Instability of either the wrist or elbow joint
- Concerns for possible compartment syndrome
- Evidence of neurovascular compromise
- Fracture of the proximal third of the ulna with associated dislocation of the radial head (ie, Monteggia fracture)
Importantly, a nightstick fracture characterized by less than 50% displacement will often be treated non-operatively.1
Next Level Urgent Care Pearls
- Early mobilization (ie, within 2 weeks of injury) is increasingly recommended to optimize outcomes, however, initial full immobilization with a splint is prudent unless UC clinicians have specific guidance otherwise from an orthopedic specialist.
- Consider assault or NAT especially in pediatric patients. If this history is not available from the patient, explore further history with friends, parents, or caregivers.[16] If the details about the mechanism of injury are not consistent with the characteristics or timing of the injury or with the developmental stage of a child, this should raise suspicion of abuse.16
- If the fracture is less than 50% displaced or involves <10 degrees of angulation, splint the patient and help arrange for non-emergent orthopedic follow-up within 5-7 days.
- While many nightstick fractures may be treated surgically in delayed fashion, the only indication for emergent ORIF is an open fracture.
- In adults, current evidence does not support benefit of closed reduction for isolated ulnar shaft fractures; either they are treated conservatively or with ORIF.
- In pediatrics, closed reduction can be appropriate depending on the patient’s age and degree of angulation.
Clinical Scenario Conclusion
The patient’s radiographs showed an acute midshaft ulnar fracture. The UC clinician requested an opportunity to speak to the patient with her mother out of the room. At that time, the patient stated that her mother’s new boyfriend had assaulted her, and the injury occurred as she protected her head and face with the forearm. The patient was gently splinted without attempts at closed reduction in UC. Child protective services was notified, and the patient was immediately referred with her mother to the nearest pediatric emergency department for further NAT evaluation and assessment of her social situation.
Takeaway Points
- A nightstick fracture is a midulna fracture commonly caused by a protective positioning of the arm in the setting of an assault. Other mechanisms of injury, such as MVA and falls, can also cause this injury pattern and are more common in adults.
- Ensure an adequate history and physical exam is performed to screen for associated injuries.
- A 3-view XR series of the forearm is appropriate initial imaging. If there are concerns for wrist or elbow injury, additional dedicated radiographs are indicated of the joint(s) of concern.
- Initial options for immobilization include a modified ulnar gutter or sugar tong with a sling for arm support.
- Early mobilization (ie, within 2 weeks of fracture) after a brief period of splinting has been shown to improve functional outcomes, namely more rapid fracture union.
- Consider attempting closed reduction in children over 10 years of age if the degree of angulation is >10 degrees or >20 degrees in those under age 10.
Manuscript submitted October 28, 2024; accepted November 11, 2024.
References
- [1]. Cai XZ, Yan SG, Giddins G. A systematic review of the non-operative treatment of nightstick fractures of the ulna. Bone Joint J. 2013;95-B(7):952-959. doi:10.1302/0301-620X.95B7.31669
- [2]. Bae DS. Pediatric distal radius and forearm fractures. J Hand Surg Am. 2008;33(10):1911-1923. doi:10.1016/j.jhsa.2008.10.013
- [3]. Naranje SM, Erali RA, Warner WC Jr, Sawyer JR, Kelly DM. Epidemiology of pediatric fractures presenting to emergency departments in the United States. J Pediatr Orthop. 2016;36(4). doi:10.1097/BPO.0000000000000595
- [4]. Handoll HH, Pearce P. Interventions for treating isolated diaphyseal fractures of the ulna in adults. Cochrane Database Syst Rev. 2012;2012(6):CD000523. Published 2012 Jun 13. doi:10.1002/14651858.CD000523.pub4
- [5]. Coulibaly MO, Jones CB, Sietsema DL, Schildhauer TA. Results of 70 consecutive ulnar nightstick fractures. Injury. 2015;46(7):1359-1366. doi:10.1016/j.injury.2015.02.012
- [6]. Patel A, Li L, Anand A. Systematic review: Functional outcomes and complications of intramedullary nailing versus plate fixation for both-bone diaphyseal forearm fractures in children. Injury. 2014;45(8):1135-1143. doi:10.1016/j.injury.2014.04.020
- [7]. Allen CM. Digital Radiographic Exposure: Principles & Practice. University of Missouri; 2022. Accessed August 16, 2022. Chapter 9. https://umsystem.pressbooks.pub/digitalradiographicexposure/chapter/radiographic-angulations
- [8]. Tawonsawatruk T, Phoophiboon P, Kanchanathepsak T, Tuntiyatorn P. Comparative Analysis of Treatment Outcomes: Modified Ulnar Gutter Slab vs. Sugar Tong Slab for Distal Radioulnar Joint Instability Following Triangular Fibrocartilage Complex Repair. Journal of Clinical Medicine. 2023; 12(20):6574. https://doi.org/10.3390/jcm12206574
- [9]. Jo YH, Lee MK, Lee YS, et al. Radiographic and clinical outcomes of muenster and sugar tong splints for distal radius fractures: a comparative study. BMC Musculoskelet Disord. 2024;25(1):261. Published 2024 Apr 3. doi:10.1186/s12891-024-07362-9
- [10]. Ahmadi A, Bazargan-Hejazi S, Heidari Zadie Z, et al. Pain management in trauma: A review study. J Inj Violence Res. 2016;8(2):89-98. doi:10.5249/jivr.v8i2.707
- [11]. Hussain A, Nema SK, Sharma D, Akkilagunta S, Balaji G. Does operative fixation of isolated fractures of ulna shaft result in different outcomes than non-operative management by long arm cast? J Clin Orthop Trauma. 2017;9:86-91. doi:10.1016/j.jcot.2017.12.004
- [12]. Handoll HH, Madhok R. Closed reduction methods for treating distal radial fractures in adults. Cochrane Database Syst Rev. 2003;(1). doi:10.1002/14651858.CD003763
- [13]. Patel A, Li L, Anand A. Systematic review: Functional outcomes and complications of intramedullary nailing versus plate fixation for both-bone diaphyseal forearm fractures in children. Injury. 2014;45(8):1135-1143. doi:10.1016/j.injury.2014.04.020
- [14]. Maleitzke T, Plachel F, Fleckenstein FN, Wichlas F, Tsitsilonis S. Haematoma block: a safe method for pre-surgical reduction of distal radius fractures. Journal of orthopaedic surgery and research. 2020;15(1), 351. https://doi.org/10.1186/s13018-020-01819-y
- [15]. Smith WR, Stahel PF, Suzuki T, Gabrielle P. Musculoskeletal trauma surgery. In: Skinner HB, McMahon PJ, eds. Current Diagnosis & Treatment in Orthopedics. 5th ed. The McGraw-Hill Companies; 2014: Chapter 2.
- [16]. Christian CW; Committee on Child Abuse and Neglect, American Academy of Pediatrics. The evaluation of suspected child physical abuse [published correction appears in Pediatrics. 2015 Sep;136(3):583. doi: 10.1542/peds.2015-2010]. Pediatrics. 2015;135(5):e1337-e1354. doi:10.1542/peds.2015-0356
Author Affiliations: Chandrika Janumpalli, BS, Kentucky College of Osteopathic Medicine. William Bradley Strauch, MD, Adena Orthopedic and Spine Institute, Chillocothe, Ohio. Authors have no relevant financial relationships with any ineligible companies.
Download the Article PDF: Urgent Care Diagnosis and Management of Midshaft Ulnar (Nightstick) Fractures
