Published on
Urgent message: Fragile skin lacerations in geriatric patients require a different repair strategy from those in younger patients. Despite the increased complexity of their wounds, most elderly patients with lacerations can be appropriately managed in the urgent care center.
Oscar D. Almeida, Jr., MD, FACOG, FACS and Amy Hunter, DNP, FNP-BC, MSN-RN
INTRODUCTION
Skin tears form a subcategory of traumatic lacerations frequently affecting older adults. A study that searched Medline and Cochrane Reviews found that patients over 65 years accounted for 88.2% of skin tears, with 41.3% reported in the 75- to 84-year-old group.1 Falls in this patient demographic account for a significant number of lacerations: 60% occur in the home, 30% outside the home, and 10% in an assisted healthcare center such as a hospital, clinic, or nursing/rehabilitation facility. Although falling is not considered a normal part of the aging process, there are age-related changes that may place older adults at a greater risk.2 Interestingly, individuals 65 years of age or older were found to have a 27% annual probability of falling.3 This age group represents 15.2% of the population, approximately one in every seven Americans.4
In the geriatric population, even a minor injury may cause a skin tear. These traumatic lesions usually result from friction or blunt trauma on fragile skin. Additional risk factors include problems with mobility and balance, alterations in cognitive status, and visual impairment. Patients on anticoagulant therapy and those with comorbidities such as diabetes and peripheral vascular disease may suffer delayed wound healing and secondary infections.
As we age, collagen and hyaluronic acid production decrease, progressively making our skin thinner. The loss of dermal thickness and subcutaneous fat, in a setting with sufficient force against fragile skin, may produce skin-tearing injuries. Although a skin tear can occur on any anatomical location, they are often sustained on the extremities. The pretibial and forearm/dorsal aspect of the hands are common sites for these injuries. Unfortunately, due to skin fragility, some skin tears are not amenable to repair using standard suture or tissue adhesive techniques. Clinically, skin tears may be classified according to the STAR (Skin Tear Audit Research) system (Table 1).5 The usefulness of this instrument is twofold: First, to describe and document the degree of epidermal loss and state of the remaining epidermal tissue of a particular wound; second, to assist the healthcare provider with the treatment plan depending on the extent of the acute lesion. For example, a Category 1a skin tear, although having a fragile thin skin flap, can often be repaired by employing a Steri-Strips and suture or skin adhesive techniques, whereas a Category 3 skin tear where the skin flap is completely absent will heal by secondary intention.
| Category 1a | The edges can be realigned to the normal anatomical position (without undue stretching) and the skin or flap color is not pale, dusky, or darkened |
| Category 1b | The edges can be realigned to the normal anatomical position (without undue stretching) and the skin or flap color is pale, dusky, or darkened |
| Category 2a | The edges cannot be realigned to the normal anatomical position and the skin or flap color is not pale, dusky, or darkened |
| Category 2b | The edges cannot be realigned to the normal anatomical position and the skin or flap color is pale, dusky, or darkened |
| Category 3 | The skin flap is completely absent |
STRATEGIES FOR SKIN TEAR REPAIR
Due to aging, the junction where the papillae bond the epidermis and dermis thins out, resulting in less cohesiveness of the two layers of the skin. This normal physiologic process leads to increased susceptibility to injury from friction and shear. Elderly patients with skin tears, especially the critically or chronically ill, may develop secondary wound infections. Any strategy that minimizes the possibility of infection and delayed wound healing are paramount for a successful outcome. Therefore, management of these lesions should include the use of aseptic technique.6 Prophylactic antibiotic therapy may be considered, and a tetanus toxoid vaccine administered if the patient has not received one in the past 10 years. Since elderly patients have a degree of osteoporosis which place them at an increased risk of fractures, x-rays should be obtained as the patient may have simultaneously sustained a fracture. Finally, these injuries may be the result of an underlying condition such as loss of equilibrium, visual impairment, or cognitive changes and must be investigated.
Cleansing and Suture Technique
The first step in repairing a skin tear is to gently cleanse the wound with soap and water in order to achieve dilution of the microbial load. Although sterile water or isotonic saline may be used, tap water has been evaluated and found to be safe for wound cleansing. Since many elderly patients are on anticoagulant therapy, applying pressure alone over the wound may not stop the bleeding. Topical LET gel (lidocaine 4%, epinephrine 1:2000, tetracaine 0.5%) provides a safe and cost-effective adjunct for hemostasis and analgesia in these circumstances.7
After an initial wound assessment, including classification of the skin tear, appropriate debridement is undertaken. If hemostasis cannot be achieved by pressure alone, apply 1–3 mL of LET gel directly on the wound and cover the lesion with waterproof dressing (eg, Tegaderm) for 15–30 minutes. Although several hemostatic agents are available to stop/slow down bleeding, they are more expensive and not as readily available in the urgent care clinics. When hemostasis is achieved, carefully remove the dressing.
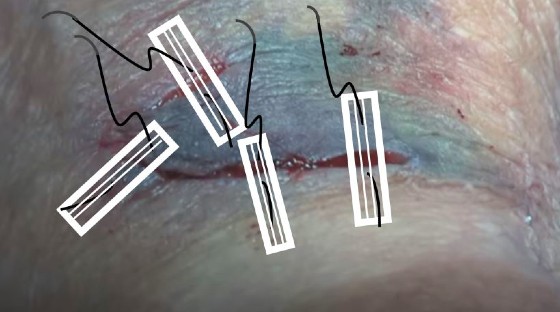
Unlike a younger patient’s skin whose thicker dermis can tolerate the increased tensile strength of sutures, fragile skin in geriatric patients usually cannot withstand a typical laceration repair. Placing sutures in the friable skin of an elderly patient may create a “suture drag” or “cheese-wire” effect as the suture under tension will often tear through the skin. This iatrogenic skin damage will increase morbidity and delay wound healing. Applying Steri-Strips over the skin tear in an elderly patient functions as an added layer of skin, allowing suturing and withstand increased tension. Figure 1 illustrates how a skin tear flap can be properly repaired following the strategic placement of Steri-Strips and suture. Additionally, using 4-0 nylon suture in a single interrupted fashion provides optimal tensile strength for the repair. Skin tears that cannot be realigned to the normal anatomical position due to partial absence of the skin flap (Category 2a, 2b) may be partially repaired with Steri-Strips and suture or tissue adhesives and depend on the remainder of healing by secondary intention. Complete skin tears (Category 3) must rely entirely on healing by secondary intention. Skin tears usually follow a 7- to 14-day course for healing. Once the wound is healed and sutures removed, gently take off the Steri-Strips. Examine the healed wound carefully for any signs of infection that may have been obscured.
Tissue Adhesives Technique
Tissue adhesives provide another treatment option for repairing fragile skin tears in small superficial lacerations. When the “surgical glue” is applied to an epidermal flap, it forms a strong bond across apposed wound edges, allowing normal healing to occur. The tissue adhesive forms a “scab” when applied and falls off after 5 to 10 days. Irregular-shaped skin tears do well with tissue adhesives as they can be approximated to the underlying dermis and surrounding epidermis. This is especially useful in shredded thinner-width skin tears when suturing is not feasible due to a smaller horizontal width section of the epidermal flap. In order for the tissue adhesive to adhere properly, the epidermal tissue must be dry and without bleeding. Generally, at least three applications of the tissue adhesive are necessary for an optimum repair. Advantages of tissue adhesives include decreased procedure time because of its quick spread over the tissues, lack of sutures/subsequent suture removal, pain-free application, and providing a water-resistant protective coating. Contraindication for using tissue adhesives include repair of tissues requiring sutures to achieve increased tensile strength, deep and crush wounds, and infected lacerations.
Unna Boot Technique
Skin tears in the lower extremity of geriatric patients, if neglected or improperly treated, can progress to a venous leg ulcer (VLU). The Unna boot was developed by the German dermatologist Paul Gerson Unna using a zinc paste to treat dermatitis associated with VLUs by producing high counter-pressure during ambulating and a low resting pressure.
The Unna boot is a prepackaged gauze bandage soaked with zinc oxide. Zinc oxide keeps the wound moist and expedites the healing process. Once the Unna boot is applied by wrapping the foot, ankle, and lower leg to just below the knee, it is covered with an outer wrap (Ace wrap or Coban) and must be changed every 3–7 days. Although not intended for exercise, you can walk with the Unna boot. Contraindications for using the Unna boot include acute pulmonary edema, cellulitis, deep vein thrombosis, arterial insufficiency, infected venous ulcers, and phlebitis.
Prophylactic Measure to Enhance Skin Thickness in the At-Risk Elderly Patient
As stated earlier, thinner skin places elderly patients at higher risk for a more cumbersome healing process in the event of traumatic lacerations. Regular skin application of 12% ammonium lactate lotion8 in at-risk areas such as the pretibial, forearm, and dorsal aspects of the hand increases the thickness of the epidermis and dermis. This effect enhances tensile strength, allowing for suture placement in these delicate skin areas.
Pearls
- Achieve hemostasis prior to closing the skin tear.
- Practice aseptic technique in order to minimize the risk of secondary infections.
- Document the STAR system category to communicate the degree of skin tear with the healthcare providers involved in the patient’s care.
- Consider using the Unna boot technique when continued lower extremity pressure over a wound ulcer may be beneficial.
- Application of 12% ammonium lactate solution in at-risk skin areas will increase the thickness of the epidermis and dermis.
● Investigate and address the underlying condition that led to the injury in the elderly patient.
CONCLUSION
Older adults are considered one of the most vulnerable populations to care for in an urgent care setting. The increased prevalence of chronic wounds due to loss of skin elasticity as well as episodic acute injuries resulting in wounds can greatly affect the quality of life in the elderly. Normal changes that occur during the aging process in combination with multiple comorbidities, chronic medical conditions, multiple medications, and slowed wound healing make early recognition and proper knowledge and treatment of laceration and wounds imperative. Delayed, inadequate, or incorrect wound treatment and repair can lead to negative outcomes for older adults, such as secondary infection, skin ulceration, and in extreme cases amputation.
Utilization of the STAR system provides the clinician with an evidenced-based tool that supports decision-making on wound repair and/or closure as well as providing a documentation system that can be useful when tracking wound healing progress over an extended period of time. Once a wound-closure method is chosen, achieving hemostasis and practicing proper aseptic technique are standards of clinical practice. Knowledge and empathy of older adults combined with pathophysiology and psychology of aging are also essential skills in wound and laceration care.
By utilizing the strategies discussed here for skin assessment, wound repair, and documentation, urgent care clinicians can feel confident in their knowledge and skill to achieve optimal outcomes for older adults in the event of acute or chronic skin injury. The clinical pearls are of great value in an urgent care environment when caring for older adults with wounds and lacerations, and can help guide the decision-making process for evidenced-based treatment plans and improved outcomes in the geriatric population.
REFERENCES
- Ratliff CR, Fletcher KR. Skin tears: A review of the evidence to support prevention and treatment. Ostomy Wound Manage.2007;53(3):32-42.
- Alexander S, Hunter A. Challenges in the prevention of falls and fall-related injuries in older adults. Clin Nurse Specialist. 2017;31(1):20-22.
- Al-Aama T. Falls in the elderly: spectrum and prevention. Can Fam Physician. 2014;60(3):225.
- U.S. Census Bureau, Population Estimates: 2017 Profile of Older Americans; April 2018.
- Carville K, Lewin G, Newall N, Haslehurst P. STAR: a consensus for skin tear classification. Primary Intention. 2007;15(1):18–28.
- Almeida OD Jr. The role of aseptic technique during repair of traumatic lacerations in the urgent care center. J Urgent Care Med. Available at: https://www.jucm.com/the-role-of-aseptic-technique-during-repair-of-traumatic-lacerations-in-the-urgent-care-center/. Accessed May 2, 2021.
- Kundu S, Achar S. Principles of office anesthesia: Part II. Topical anesthesia. Am Fam Physician. 2002;66(1):99-102.
- Lavker RM, Kaidbey K, Leyden JJ. Effects of topical ammonium lactate on cutaneous atrophy from a potent topical corticosteroid. J Am Acad Dermatol. 1992;26(4):535-544.
Author affiliations: Oscar D. Almeida, Jr., MD, FACOG, FACS, Urgent Medcare Center, in Huntsville, AL. Amy Hunter, DNP, FNP-BC, MSN-RN, University of Alabama in Huntsville; Urgent Medcare in Huntsville, AL.


