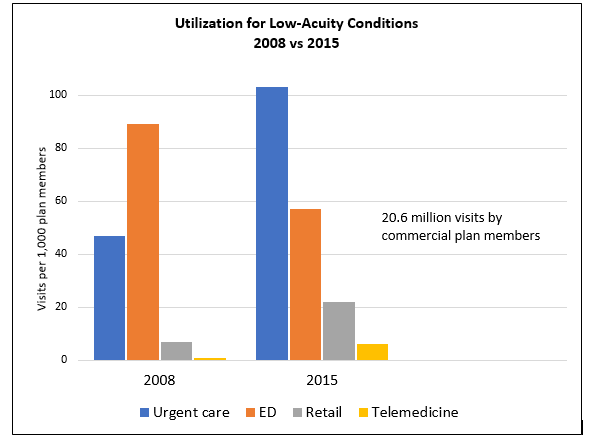
The key question posed by the authors of an article published last month in JAMA Internal Medicine: How have patterns of care for low-acuity patients with acute conditions changed over time among a commercially insured population? The answer is, quite a lot—due largely (and much to the benefit of) urgent care. Working from 2008–2015 claims data supplied by Aetna, the researchers looked at utilization, inflation-adjusted price, and spending associated with approximately 20 million acute care visits per study year for acute respiratory infections, urinary tract infections, rashes, and musculoskeletal strains.
Considering all treatment venues (the ED, urgent care, retail clinics, and telemedicine), treatment of those low-acuity conditions increased 31% over the study period; however, visits to the non-ED acute care setting jumped 140%, with urgent care getting the biggest bump. In what may be the key understatement of the year, the authors concluded that “these findings suggest that patients are more likely to visit urgent care centers than EDs for the treatment of low-acuity conditions.”
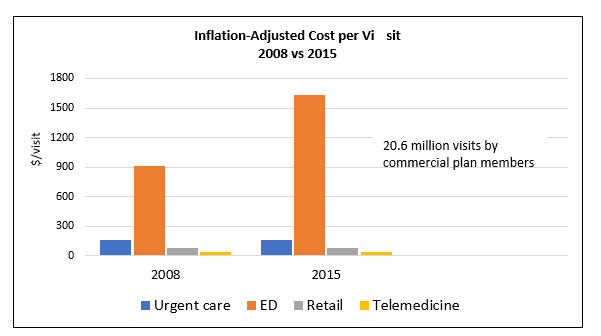
Meanwhile, the cost of a trip to ED rose 79% over the study period, while the average cost of a visit to other nonacute settings is stable.
The particulars (including cost data), illustrated below, paint an even more promising picture for urgent care.
UTILIZATION AND COST FOR LOW-ACUITY CONDITIONS IN ACUTE CARE SETTINGS
Data source: Poon SJ, Schuur JD, Mehrotra A. Trends in visits to acute care venues for treatment of low-acuity conditions in the United States from 2008 to 2015. JAMA Intern Med. September 4, 2018. [Epub ahead of print]
