Urgent message: Realistic—and recurring—simulation of emergency scenarios is essential to helping urgent care providers and support staff function as a team when real-life pediatric emergencies take place in the urgent care center.
Ilanalee Cabrera, MSN, RN, CPNP, Wilma Santiago, BSN, RN, CPN, Tiffany Christensen, Rachel Lucas, DO
Citation: Cabrera I, Santiago W, Christensen T, Lucas R. Using simulations and skills stations to enhance emergency preparedness in pediatric urgent care. J Urgent Care Med. 2021;15(10):31-33.
Introduction
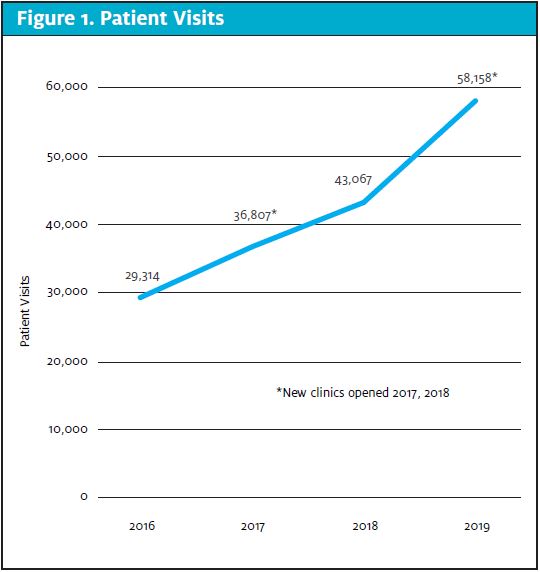
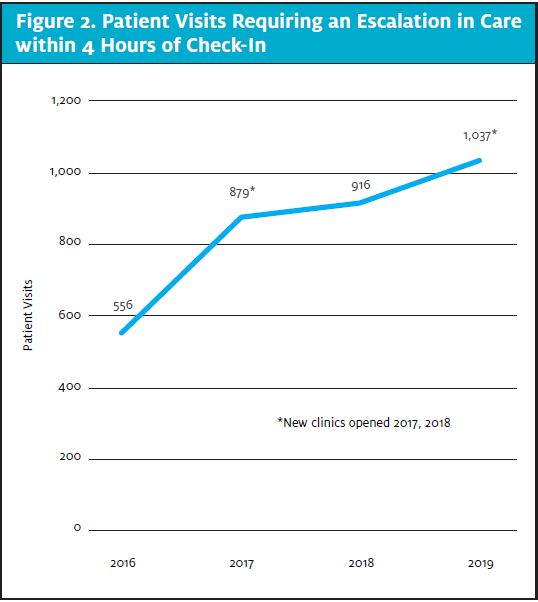
As more patients seek convenient after-hours acute care clinics, effective emergency response requires regularly scheduled, multidisciplinary emergency simulations. Similar to other urgent care clinics across the country, Children’s Wisconsin Urgent Care clinics have encountered higher patient volumes and an increase in patient acuity in recent years. Our patient visits have increased steadily year to year, to the extent that visits in 2019 were almost double those of 2016 (Figure 1). Patients requiring an escalation in care within 4 hours of check-in to urgent care also increased steadily from 556 in 2016 to 1,037 in 2019 (Figure 2).
Research shows that emergency response skills deteriorate quickly after training.1,2 Conversely, regularly and repeatedly practicing a skill may prevent rapid skill deterioration,1-3 and more frequent training is superior to conventional training to ensure high-quality resuscitation skills.1-3
Therefore, our hypothesis is as follows: Using simulated emergency scenarios in the simulation lab, participant assessment of feeling well-prepared or better will increase by 20% from presurvey to postsurvey for all urgent care staff. For in situ (in clinic) simulations, postsimulation surveys will reflect that 75% of participants feel more prepared after the simulation.
Methods
Prior to late 2017, our urgent care team practiced emergency response sporadically. Since that time, we have implemented regularly scheduled multidisciplinary emergency simulations and skills stations in our Simulation Lab and at our urgent care clinics.
While we have been doing regularly scheduled simulations since late 2017, data collection began in January 2019. Eighty-one unique staff members participated through 2019, with a total number of 141 participants, with “participants” including staff members who took part in more than one simulation. (The low number of participants reflected in the graphs reflects the recent start of data collection, as well as the purposeful limitation of participants per simulation.) To evaluate the effectiveness of the simulations, participants completed pre and postsimulation Likert scale surveys.
Simulations were open to all urgent care staff including physicians, nurse practitioners, physician assistants, nurses, medical assistants, and front desk staff. Previous simulation scenarios have included asthma and hypoxia, severe bronchiolitis, anaphylaxis, closed head injury, seizures, hyperthermia, sepsis, diabetic ketoacidosis, and cardiac arrest of the child and adult. Both high- and low-fidelity manikins were used.
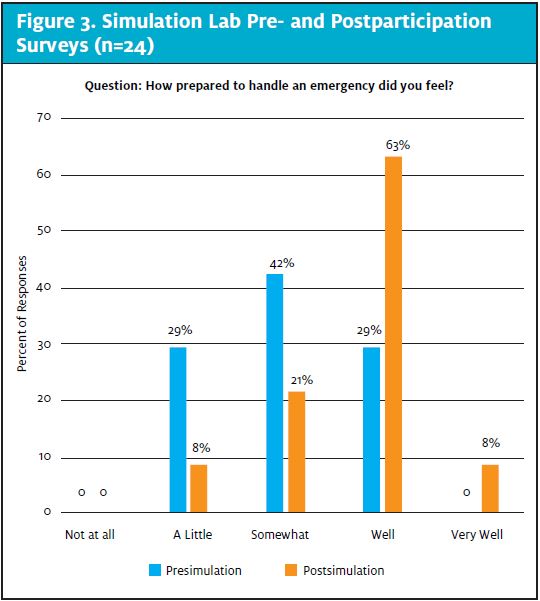
For simulations in the Simulation Lab, a pre- and postparticipation survey was completed by each participant in paper form. Preparticipation survey questions included whether the participant had attended an emergency simulation “prior to today,” whether the participant had been involved in an actual emergency requiring resuscitation in a clinical setting, and how prepared the participant felt regarding handling emergencies in urgent care. Postsurvey questions asked how prepared the participant felt to handle emergencies in urgent care after participating in the simulation.
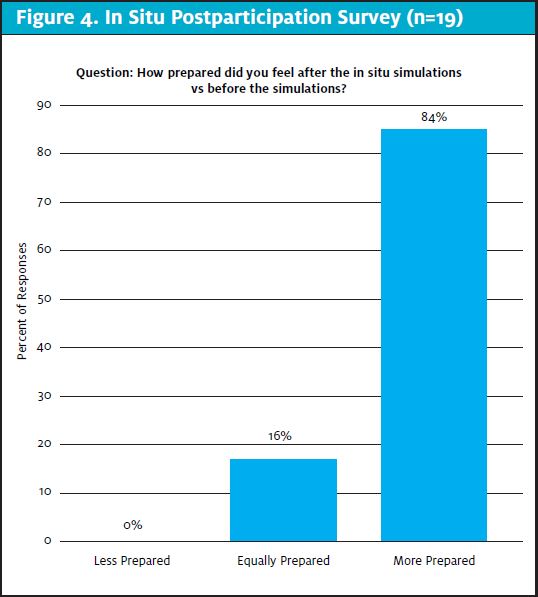
Due to the nature of the surprise for in situ simulations, we were unable to perform a presurvey; however, all participants are sent a postparticipation survey by email, asking whether they felt more prepared for an emergency after attending the simulation.
To complement the emergency scenarios, we also set up skills stations, which included c-collar application with and without helmet removal, weight estimation using a measuring tool, and bagging a patient with a tracheostomy tube. Skills stations were often not accessible for practice during our in situ simulations because of timing related to patient care.
In simulations held in the Simulation Lab, we performed a pre-brief to discuss the basic assumption that all staff are intelligent, capable, and trying their best. We agreed on the fiction contract, which acknowledged that the scenario is as real as possible but that learning depends on full participation. And, finally, preparatory information was provided. The debrief included re-examining the scenario for learning.
Results
Our data indicate that almost universally, participants felt more prepared to handle an emergency after attending the simulation. Participants who felt “a little prepared” decreased from 29% to 8%; those who felt “somewhat prepared” decreased from 42% to 21%; those who felt “well prepared” increased from 29% to 63%; and those who felt “very well prepared” increased from 0% to 8% (Figure 3). Participant responses after the in situ simulations indicated 84% of participants felt more prepared after the simulation, while 16% felt the same level of preparedness (Figure 4).
Conclusions
Because all staff play an important role in caring for the patient and family during an emergency, multidisciplinary simulations are essential to increase staff preparedness to provide high-quality care during such an event.
Limitations
Survey data are self-reported and subjective. We were unable to assess improvement in preparedness from in-situ simulations given no preparticipation survey. It is difficult to compare data between simulation dates, as scenarios may differ between simulations. Additionally, because data were drawn from a small sample size at a single center, results may not be generalizable.
Next Steps
Future work could compare preparedness to years working in urgent care, total years of experience in healthcare, previous simulation attendance, and the participant role within urgent care. Interdepartmental simulations would be beneficial, especially in our clinics that share workspace. Rapid cycle deliberate practice vs traditional simulation would be interesting to study, as would retention of skills at regular intervals after training.
References
- Anderson GS, Gaetz M, Statz C, Bin K. CPR skill retention of first aid attendants within the workplace. Prehosp Disaster Med.2012;27(4):312-318.
- Anderson R, Sebaldt A, Lin Y, Cheng A. Optimal training frequency for acquisition and retention of high-quality CPR skills: a randomized trial. Resuscitation.2019;135:153-161.
- Lin Y, Cheng A, Grant VJ, et al. Improving CPR quality with distributed practice and real-time feedback in pediatric healthcare providers – a randomized controlled trial. Resuscitation. 2018;130:6-12.
- Petersen TL, Rodgers A, Shuh A, Pearce J. Proceedings from Medical College of Wisconsin: Department of Pediatrics Lunch and Learn Faculty Development Lecture: Faculty Development in Medical Simulation: Session 1: Stages of a Simulation: From Pre-Brief to Debrief. Milwaukee, WI. 2019.
Acknowledgements
The authors wish to thank Kathy Szopinski, BSN, RN, Amanda Kotowski, DNP, RN, CPNP-AC/PC, CLC, Lauren Ladwig, RN, Jaspreet Samra, MPH, CPHQ, Laurie Smrz, BSN, RN, AE-C, Danielle Smith, MSN, RN, CNL, Vaishali Singh, MD, Amy Romashko, MD, Heather Paradis, MD, and Tara Petersen, MD, MSEd.
Author affiliations: Ilanalee C. Cabrera, MSN, RN, CPNP, Children’s Wisconsin. Wilma J. Santiago, BSN, RN, CPN, Children’s Wisconsin. Tiffany N. Christensen, Children’s Wisconsin. Rachel C Lucas, DO, Children’s Wisconsin.
Read More on Emergency Preparedness:
- Preparedness For Emergencies In Pediatric Urgent Care Settings
- Developing An Emergency Preparedness Plan For Urgent Care
- Emergencies In The Office: Why Are 911 Calls Placed From Family Medicine And Urgent Care Offices?