In the May issue of JUCM, we outlined what we were seeing with E/M coding levels utilizing the new AMA guidelines vs 2020 and 2019 levels. As COVID-19 visits steadily declined from January through June, we began to see a return to more “normal” urgent care visits. That was short-lived. July’s sharp increase in visit volumes was again driven by COVID-19!
Here’s the update we promised.
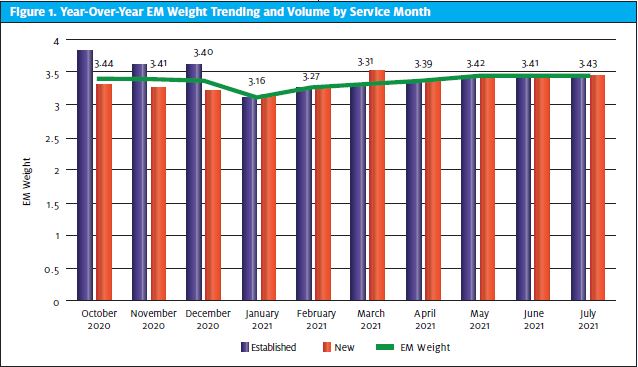
As a reminder, we saw E/M levels decline in January and the first part of February vs 2020 levels, with slow and steady recoveries since. Most of the decrease and subsequent increase was attributed to a learning curve associated with the drastic change in the way codes are derived compared with the old rules, and training providers to document their medical decision making in its entirety.
Since March we have continued to see more recovery to pre-2021 levels, as seen in Figure 1.
During 2020, new patients accounted for 49.9% of total UC visits, a 28% increase from the historical 39% average. In 2021, new patients are still higher than the historical average, but have declined to 45.6% of UC visits while existing patients have risen to 54.4%. Much of the increase in existing patients this year could be related to the new patient surge in 2020, driven by the demand for COVID testing. As urgent care centers were at, or nearing, their peak in terms of visit volumes last fall, they were performing roughly 725,000 COVID tests per week, about 10% of the total in the U.S. at that time, according to a Vox profile.1
As we explained in the May article, the amounts Medicare allowed for established patient E/Ms in 2021 increased approximately 20%, helping to soften the blow of both the degradation in average E/M weights and the shift back to a majority of established patients. We have seen these increased payments from Medicare, as anticipated. We continue to monitor the large commercial payers for similar adjustments. Further, we remain hopeful that commercial payers continue to utilize Medicare guidance and pricing in setting their fee schedules—or a multiple thereof—and follow suit by increasing their established patient E/M allowable amounts, as well.
“We believe providers can benefit from continued training on the new E/M guidelines. There still appear to be many who do not even realize a change took place!”
Unfortunately, our return to a more “normal” life has not materialized. During Fourth of July weekend, many of us celebrated with our vaccine shields and faces unmasked. It felt kind of normal. Little did we know, our new normal would again be interrupted by an unwanted and uninvited guest, the Delta strain, which at the time accounted for a minority of all COVID-19 cases, compared with over 80% today per CDC estimates.
The Delta strain has derailed any normalization of urgent care for the time being, and possibly forever. COVID-19 surge number 4 has been monopolizing many areas in the United States. During the last 3 weeks of July, UC visit levels took off in certain areas like Richard Branson and Jeff Bezos—straight to space and out of Earth’s atmosphere.
“We encourage all urgent care centers to be diligent with insurance follow-up on unpaid claims. We have seen accounts receivable grow as the staffing levels in billing departments are not adequate to follow-up and resolve claims as a result of the record-setting volumes.”
As for the per-visit reimbursement, we believe providers can benefit from continued training on the new E/M guidelines. There still appear to be many who do not even realize a change took place!
There are only two things in life that are certain: death and taxes. So, while we don’t know what will happen industrywide with E/M codes, we do have some suggestions for surviving and thriving in this COVID-dominated environment.
- Continue to educate providers on the documentation requirements for the new E/M coding guidelines
- Be sure you are utilizing your real-time insurance eligibility application.
- Enroll in uninsured COVID-19 testing reimbursement programs.
- Implement a credit-card-on-file program to handle any balances due from patients after insurance has processed.
- Utilize e-statements or text message balance reminders to facilitate easier payments from patients.
It is essential to not overlook the last two items above and assume that patient responsibility is no longer an issue due to COVID-19. Many clinics have become lax in enforcing time-of-service and patient balance protocols during the public health emergency due to pronouncements by many payers that cost-sharing will be waived for patients receiving COVID-19 tests. While those policies are valid, they can be overridden to the extent an employer-funded plan’s policy differs. In 2020, a record 67% of working Americans were insured under self-funded plans.
We encourage all urgent care centers to be diligent with insurance follow-up on unpaid claims. We have seen accounts receivable grow as the staffing levels in billing departments are not adequate to follow-up and resolve claims as a result of the record-setting volumes.
We will keep you posted as we continue to monitor this situation.
References
- Molla R. Covid-19 is turning urgent care centers into America’s favorite clinics. Vox. Available at: https://www.vox.com/recode/21562230/urgent-care-center-covid-19-testing-vaccine-health-care. Accessed August 6, 2021.

