Alan A. Ayers, MBA, MAcc is President of Experity Networks and is Senior Editor, Practice Management of The Journal of Urgent Care Medicine.
Urgent message: Whether an urgent care must have a provider on-site during all operating hours comes down to the operator’s risk tolerance.
As a matter of patient safety, many urgent care centers have adopted a policy that if no provider is on-site, they must lock the doors and refuse entry of any patients. As a result, patients wait outside before the center opens—even if it opens later than scheduled—and the center closes any time the provider is unavailable.
The rationale is that a provider should be on-site any time patients are present so they can administer lifesaving treatment if needed. From a liability perspective, this sounds like a reasonable policy, but it is also one that creates numerous operational challenges.
Reasons Why an Urgent Care May Operate Without a Provider
Urgent care tends to be busiest in the morning, so regardless of the center’s opening time there are typically patients waiting outside as soon as the doors are unlocked. It can take 10–15 minutes to register the first patient, after which the medical assistant takes vitals, records intake notes, and rooms the patient. It’s therefore likely if the center “opens” at 8:00 am that the first patient won’t be “available” to the provider until nearly 8:30. Given provider pay is the center’s biggest expense item, this results in idle time that frequently also puts the center “behind” for several hours until there’s a lull in patient arrivals. Faster throughput and smoother flow can be accomplished by either staggering the provider’s arrival to availability of the first patient, or having the staff open doors 15 minutes early so the first patient is ready to be seen at 8:00 am.
Additionally, many urgent care services do not require a provider, including drug testing and asymptomatic COVID-19 testing. If a provider is absent, rather than close the center resulting in a loss of business (and a loss of pay for staff), a center would continue to see nonprovider visits and first register and then divert medical presentations to other locations. Increasingly, telemedicine can solve this conundrum. Registration and intake processes would occur as usual, but the patient would be escorted to an exam room with a video connection to a provider in another location. Under telemedicine parity laws, this scenario should still enable full reimbursement for the patient visit.
Risk Management Considerations
While patient safety in an emergent situation may be the rationale for requiring a provider to be on-site during all opening hours, our legal researcher could not find sources addressing the situation specifically in urgent care settings. This is keeping in mind that urgent care centers are generally considered “doctors’ offices” not subject to the Emergency Medical Treatment and Labor Act (EMTALA) and therefore not regulated in the same manner as emergency departments. So, lacking precedent to the contrary, we can conclude the policy adaptation comes down to the individual operator’s risk tolerance.
Patients usually don’t call urgent care to assure a provider is present before heading there. From a practical standpoint, if the concern is having a provider available to render lifesaving aid, whether an emergency appears is not dependent on having a provider present. In other words, what’s the staff going to do if a patient is in crisis on the sidewalk or in the parking lot because the center’s doors are locked? In such a situation, the staff should call 911 and render aid as capable, the same as if the patient were in the waiting room.
While lifesaving situations have presented at urgent care, the hypothetical that a provider must be present to deal with them ignores how centers are staffed and equipped. Increasingly, urgent care centers are staffed by physician assistants and nurse practitioners who should have Basic Life Support (BLS) certification, but many employers either do not require ACLS (advanced cardiovascular life support) and PALS (pediatric advanced life support) certification, or they require it within 3–6 months of starting, which leaves a gap without the training.
In addition to special training which must be refreshed regularly, ACLS and PALS require specified equipment, supplies, medications, and staff support—all of which must be periodically refreshed. Even if a physician is ACLS-certified, it’s unlikely MAs will have experience in “running a code.” As a result, most urgent care centers are equipped for BLS, including a wall-mounted AED. In the rare occurrence that a patient falls into cardiac arrest, these centers would administer BLS, call 911, and rely on the lifesaving capabilities and training of the Emergency Medical Technicians who would also transport the patient to the hospital.
Nurse Practitioners and Physician Assistants
While it can be expected that physicians will have had ACLS training, the core clinical workforce in urgent care is transitioning to Advanced Practice Clinicians (APCs).
Nurse practitioners are now working solo in many urgent care centers.1 An NP is an advanced practice registered nurse (APRN) who has additional training and responsibilities for administering patient care compared with registered nurses (RNs).2 Moreover, recently, nurse practitioners have been successful in lobbying many states to broaden their scope of practice, even owning and operating their own urgent care centers.3–5
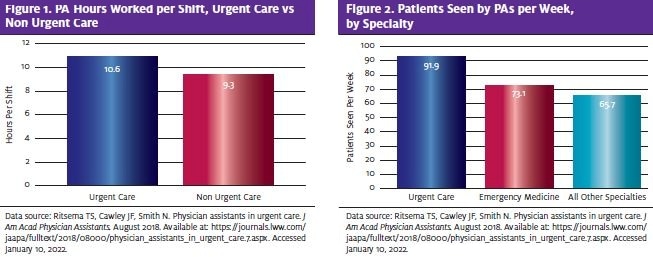
As for physician assistants, the percentage of PAs who work in urgent care has nearly doubled in the last 10 years.6,7 Research also shows that PAs in urgent care work longer shifts (an average of 10.6 hours) than those who don’t practice urgent care (9.3 hours). In addition, PAs in urgent care see many more patients per week (91.9 on average) for their primary employer than those in emergency medicine (73.1) and those in all other specialties combined (65.7).6 PAs in urgent care also perform more procedures (82.3%) than both PAs in emergency medicine (69.2%) and PAs in all other specialties (58.7%).6
These factors mean that APCs are shouldering more of the load and creating more opportunities (as well as more mistakes and potential liability).
One article states, “Although advocates claim that studies show that NPs can provide comparable care to physicians, they fail to acknowledge that this research has always been done with supervised NPs. The truth is that there are absolutely no studies that show nurse practitioner safety and efficacy when practicing independently.”8
If you add to this the situation where APCs are staffing the urgent care without a physician on-site, there is an even greater chance of issues with more complex patient needs.9
Avoiding Services Beyond Capabilities
Of course, if a patient were to arrive with an adverse medical event requiring advanced lifesaving, an on-duty physician would be there to administer emergency treatment. However, there are a number of questions surrounding when APCs are staffing the urgent care without a provider.
While there is no standard, regulation, or requirement (other than basic risk management) as to whether an urgent care center can open its doors daily without a provider being present, research shows that most malpractice claims attributed APC liability are traced to clinical and administrative factors that are easily identified:
- Assumption of too much responsibility
- Inadequate physician supervision
- A lack of written protocols
- Deviation from written protocols
- Failure and delay in seeking referral or physician collaboration
The most obvious way to avoid an unsupervised PA or NP providing services beyond their capabilities is to have a physician on-site during all opening hours. Because that’s not always financially feasible, many operators enable “supervising physicians” to be available by phone at all times.
In any case, urgent care should function as a “team” of physicians, physician assistants, and nurse practitioners to make certain that their APCs don’t attempt to provide services beyond their capabilities or those not permitted by law. An NP’s or PA’s work is initially closely monitored until the physician has a comfort level with the PA’s or NP’s abilities. Monitoring at regular intervals ensures continued quality performance and allows for the detection of misdiagnoses, delays in diagnoses, improper orders, or any other issues requiring attention.10
Midlevel practitioners should not be providing services beyond their capabilities or those not permitted by law. To aid with this, policy and procedure manuals should reflect consistency and adherence to clinical practice guidelines.11 Moreover, position descriptions are a useful tool that urgent care owners and managers can use to make certain that midlevel professionals are practicing within the prescribed practice guidelines.
Takeaways
Whether an urgent care operator should require a provider on-site in order to open its doors is a matter of risk tolerance, as there are business practicalities “for” and “against” yet there is no clear legal precedent. However, given the prevalence of APC staffing, urgent care operators should be cognizant of situations in which an NP or PA may be providing services beyond their capabilities. The best approach is to have clearly defined policies and procedures to assure consistency and compliance across teams, shifts, and facilities.
REFERENCES
- Shaffer P. A review of the Cochrane Review of nurse practitioners as a possible replacement for physicians. physicians for patient protection. October 20, 2021. Available at: https://www.physiciansforpatientprotection.org/a-review-of-the-cochrane-review-of-nurse-practitioners-as-a-possible-replacements-for-physicians/. Accessed January 10, 2022.
- American Association of Nurse Practitioners. Nurse practitioner role grows to more than 270,000. American Association of Nurse Practitioners. January 28, 2019. Available at: https://www.aanp.org/news-feed/nurse-practitioner-role-continues-to-grow-to-meet-primary-care-provider-shortages-and-patient-demands. Accessed January 10, 2022.
- Reno J. Why you might see a nurse practitioner and not a doctor at your urgent care clinic. Healthline. November 3, 2019. Available at: https://www.healthline.com/health-news/nurse-practitioner-no-doctor-urgent-care-center. Accessed January 10, 2022.
- Lake AD. Florida Medical Association resident/fellow physicians oppose HB 607, which allows for advanced practice registered nurse (APRN) autonomous practice. Physicians for Patient Protection. February 26, 2020. Available at: https://www.physiciansforpatientprotection.org/the-voice-of-young-physicians-regarding-scope-of-practice/. Accessed January 10, 2022.
- Bourgeois-Law G. Do nurse practitioners pose a threat to family physicians? Can Fam Physician. December 2008. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2602626/. Accessed January 10, 2022.
- Ritsema TS, Cawley JF, Smith N. Physician assistants in urgent care. J Am Acad Physician Assistants. August 2018. Available at: https://journals.lww.com/jaapa/fulltext/2018/08000/physician_assistants_in_urgent_care.7.aspx.
- Smith N, Ritsema TS. Urgent care, a fast growing specialty for PAs and physicians. American Academy of PAs. February 9, 2018. Available at: https://www.aapa.org/news-central/2018/02/urgent-care-fast-growing-specialty-pas-physicians/. Accessed January 10, 2022.
- Bernard R. The effects of nurse practitioners replacing physicians. Physicians Practice. January 30, 2020. Available at: https://www.physicianspractice.com/view/effects-nurse-practitioners-replacing-physicians. Accessed January 10, 2022.
- Dolan S. How the growth of the urgent care industry business model is changing the healthcare market in 2021. Business Insider. Updated January 29, 2021. Available at: https://www.businessinsider.com/urgent-care-industry-trends. Accessed January 10, 2022.
- Guarisco M. Mid-level providers – who they are, what they do, and why they’re changing emergency medicine. Emergency Physicians Monthly. Available at: https://epmonthly.com/article/mid-level-providers-who-they-are-what-they-do-and-why-they-re-changing-emergency-medicine/. Accessed January 10, 2022.
- Mid-level practitioner liability: preventive action and loss reduction plan. The Doctors Company. July 2018. Available at: http://www.nmms.org/wp-content/uploads/2018/07/Mid-Level-Practitioner-Liability-MD-Resources.pdf. Accessed January 10, 2022.

