Urgent message: Neck and back pain are common issues preceding surgical intervention. Given differences in care plans, outcomes, cost, and length of stay associated with spinal surgeries, the option of referring urgent care patients to either neurosurgeons or orthopedic spine surgeons requires careful consideration.
Rami Musleh, PA-C; Angela Blagojevski, MPAS, PA-C; Randy Brush, MS, PA-C; and Jessica Bruskoski, MS, PA-C
INTRODUCTION
Neck and back pain are two of the most common reasons for people to miss work; back pain is the leading cause of disability, preventing many from performing activities of daily living.1 Up to 80% of the population will experience back pain, and 54% will have some degree of neck pain at some time in their lives.1,2 Most episodes of low back pain are short lived and require little or no treatment.3 However, those who have recurrent episodes or have structural deformities may require a surgical procedure. An estimated 650,000 to 700,000 neck and back surgeries are performed annually in the United States.4 Those who need surgery typically choose to have it performed by either by a neurosurgeon (NS) or an orthopedic spine surgeon (OS). Most patients may not know the difference between the two, and usually elect to go where they are referred to by their primary care provider.5 Similarly, urgent care providers are in a position to refer patients presenting with neck or back pain for surgical consideration.
This paper will compare the direct medical costs, length of stay, complications rates, and plan of care as they pertain to neurosurgeons and orthopedic spine surgeons.
ETIOLOGY AND PATHOPHYSIOLOGY
There are a variety of surgical approaches available for the treatment of spine diseases.9 Neurosurgeons, and orthopedic spine surgeons both perform spinal surgery, and there are significant overlaps in the different procedures that are performed. However,there are differences between the two specialties in clinical decision-making regarding spinal disorders.6
Procedures
Anterior cervical discectomies and fusions (ACDF) are the most common cervical procedures performed and utilized for the treatment of multiple cervical pathologies.2 A majority of spine surgeons utilize similar techniques in performing anterior cervical discectomies and fusions.2 A small minority of procedures are done posteriorly. Posterior cervical fusion (PCDF) is usually reserved for patients who have multiple level disease and have a higher rate of complications compared to an anterior approach.2
There are a variety of lumbar spine procedures for diseases affecting the lumbar spine, of which the most common is a spondylolisthesis.7 The treatment plan can be different between the two specialties, depending on whether the patient with spondylolisthesis has pain.7 The most common procedures performed for lumbar spine issues include anterior lumbar interbody fusion (ALIF), posterior lumbar interbody fusions (PLIF), laminectomies, and discectomies.5,7
COMPLICATIONS
Surgical complications play a significant role in postoperative outcomes. These complications include adverse intraoperative complications, postoperative complications, readmissions, surgical revisions, and prolonged hospital stays.5
Surgical complications associated with cervical procedures can include, but are not limited to, esophageal perforation, epidural hematoma, C5 nerve palsy, recurrent laryngeal nerve palsy, superior laryngeal nerve palsy, dural tears, brachial plexopathies, graft extrusion, hardware migration, infection, vascular injury, Horner syndrome, and psuedomeningeocele.2
Postoperative complications for lumbar procedures can include but are not limited to wound infections and dehiscence, hematomas, pulmonary complications, surgical revisions, incidental dural tears, and hospital readmissions.5,8-13
ECONOMIC IMPACT
Low back pain accounts for at least $50 billion in healthcare costs to Americans each year.14 When adding the cost of lost wages and decreased productivity, the figure rises to more than $100 billion.14
The cost of low back pain and the procedures that are associated with treatment are generally reported as direct medical costs and indirect (productivity and absenteeism) costs.15 These costs include transportation, cost of nonprescription medications, and visits to complementary and alternative practitioners.15
The major direct medical costs that are seen and studied most frequently are the cost of procedures, length of stay, wound complications (infections and dehiscence), urinary tract infections, reoperations, and unplanned readmissions.5,6 Any complications increase the total cost of the treatment and significantly raise the chance of prolonging hospital length of stay and time off of work.5,6,15
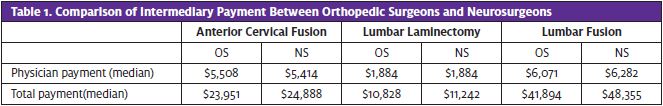
Consider the cost of the procedures each specialty performs. The median cost of physician payments for an anterior cervical discectomy and fusion are almost identical between orthopedic spine surgeons and neurosurgeons. The same holds true for total costs. (See Table 1.)5 Even though the payment analysis showed that the median total intermediary payments were higher for neurosurgery procedures for all three treatment groups, there were no statistically significant differences.5
MALPRACTICE LITIGATION
Medical malpractice is an important issue to consider due to concerns of increased healthcare costs and medical decision-making for the sole purpose of reducing legal liability. Agarwal, et al conducted a descriptive analysis of state and federal spine surgery malpractice litigation in the United States and found that there were no differences in the frequency of plaintiff verdicts in those cases where an OS was cited as a defendant compared to those case where an NS was cited as a defendant.16
SURGICAL TREATMENT OPTION COMPARISONS
Anterior Cervical Discectomy and Fusion
An anterior cervical discectomy and fusion (ACDF) is a technique commonly utilized on patients with underlying degenerative disc disease, cervical radiculopathy, and cervical myelopathy.2 Patient selection to perform an ACDF with comorbidities has been shown to be almost the same between the two specialties. Neurosurgeons were a little more willing to perform the procedure with patients that have more complex comorbidities.5,17 The only comorbidity that neurosurgeons were statistically more likely to treat was patients with osteoporosis.5
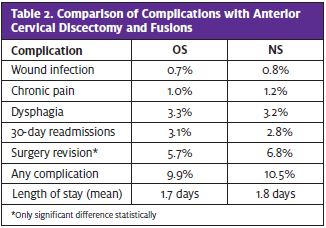
No significant differences were observed in median length of stay postoperatively after an ACDF between the two specialties.5,17 The average postoperative length of stay is 1.7 days for OS and 1.8 days for neurosurgery.5
Numerous complications can occur postoperatively after an ACDF. The most common are wound infections, continued pain, dysphagia, 30-day readmission, and revisional surgery.2 Spine surgeon specialty was not a risk factor for any of the prementioned postoperative complications for a single level ADCF, 17 and there was no significant association between the two surgeon types of any particular complications in ACDF procedures in general.5 There was a higher revisional surgery rate noted with neurosurgery as compared to orthopedic spine surgery.5 (See Table 2.)
Lumbar Fusions
Lumbar spine fusions are the most common procedure performed to correct degenerative spondylolisthesis.7 Most insurance companies will only approve lumbar fusions if there is a spondylolisthesis documented in the patient’s record.7 As a result, most researchers used that diagnosis of spondylolisthesis as a search tool to study how the presence or absence of back pain, along with spondylolisthesis, would be addressed by each specialty.7
When presented with a patient with spondylolisthesis and back pain, there were no significant differences between NS and OS on the treatment plan.7 Of the neurosurgeons given the scenario, 85% stated they would perform some kind of fusion; 15% stated they would only perform a laminectomy.7 Orthopedic surgeons responded similarly, where 80% would choose to perform a fusion, and 20% would only perform the more conservative laminectomy.7
The second scenario was a spondylolisthesis without back pain, with significant differences between the two groups.7 Neurosurgeons had 3.4 times greater odds of performing simpler laminectomies and 2.1 times greater odds of performing interbody fusions.7 Orthopedic surgeons preferred to treat this scenario with a laminectomy with posterolateral fusion and pedicle screws.7 In this scenario, 73% of OS would perform some kind of fusion, where only 61% of NS would.7
Lumbar Fusions
Lumbar spine fusions are the most common procedure performed to correct degenerative spondylolisthesis.7 Most insurance companies will only approve lumbar fusions if there is a spondylolisthesis documented in the patient’s record.7 As a result, most researchers used that diagnosis of spondylolisthesis as a search tool to study how the presence or absence of back pain, along with spondylolisthesis, would be addressed by each specialty.7
When presented with a patient with spondylolisthesis and back pain, there were no significant differences between NS and OS on the treatment plan.7 Of the neurosurgeons given the scenario, 85% stated they would perform some kind of fusion; 15% stated they would only perform a laminectomy.7 Orthopedic surgeons responded similarly, where 80% would choose to perform a fusion, and 20% would only perform the more conservative laminectomy.7
The second scenario was a spondylolisthesis without back pain, with significant differences between the two groups.7 Neurosurgeons had 3.4 times greater odds of performing simpler laminectomies and 2.1 times greater odds of performing interbody fusions.7 Orthopedic surgeons preferred to treat this scenario with a laminectomy with posterolateral fusion and pedicle screws.7 In this scenario, 73% of OS would perform some kind of fusion, where only 61% of NS would.7
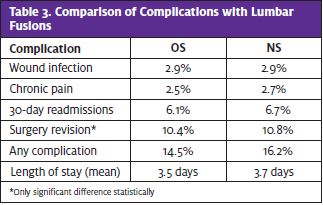
Research by Mabud, et al showed that lumbar fusions as a whole had no significant differences in length of stay (3.5 days for OS, 3.7 days for NS),5 wound infection, continued pain, and 30-day readmission.5,8,11,12 It was also shown that surgeon specialty is not a risk factor for any complications at the 30-day postoperative mark after undergoing a single level fusion.8 There was only a slightly higher incidence of surgery revisions and total complications with NS compared with OS.5 (See Table 3.)
Lumbar Laminectomy
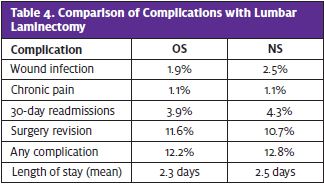
Lumbar laminectomies are the most common low back procedure performed for back pain.15 This procedure can be performed as a single procedure for lumbar stenosis without a spondylolisthesis, or with a fusion when there is instability within the spine.15 The risks of surgical complications, all-cause readmission, and revisional surgery were very similar for NS and OS.5,9,18 (See Table 4.) No significant differences were found in the average length of stay (2.3 days for OS, and 2.5 days for NS).5 One study did note that laminectomies performed by OS have double the odds for undergoing perioperative transfusion compared with those performed by NS.9
CONCLUSION
Findings suggest that both NS and OS training backgrounds produce similar outcomes in cervical and lumbar spine surgery for most parameters, including postoperative length of stay, readmission rates, direct medical costs, and most complications. Few significant associations between surgeon type and complications exist, and those that do are quite small and unlikely to be clinically meaningful. Finally, there was no difference in the frequency of plaintiff verdicts between the two specialties in studies on malpractice outcomes.
REFERENCES
- Rubin Dl. Epidemiology and risk factors for spine pain. Neurol Clin. 2017; May;25(2):353-71.
- Hemmer C. Surgical complications associated with cervical spine surgery. Orthop Nursing. 2018;37(6):348-354.
- Dyrda L. 10 things to know about spine surgery in ASCs. Becker’s ASC Review. Available at: https://www.beckersasc.com/outpatient-spine/10-things-to-know-about-spine-surgery-in-ascs.html. Accessed October 16, 2019.
- Baek J, Malik AT, Khan I, et al. Orthopedic versus neurosurgery–Understanding 90-day complications and costs in patients undergoing elective 1-level to 2-level posterior lumbar fusions by different specialties. World Neurosurg. 2019;131:e447-e453.
- Mabud T, Norden J, Veeravagu A, et al. Complications, readmissions, and revisions for spine procedures performed by orthopedic surgeons versus neurosurgeons. Clin Spine Surg. 2017;30(10):e1376-e1381.
- Bronheim RS, Cheung ZB, Phan K, et al. Anterior lumbar fusion: differences in patient selection and surgical outcomes between neurosurgeons and orthopedic surgeons. World Neurosurg. 2018;120:e221-e226.
- Lubelski D, Alentado VJ, Williams SK, et al. Variability in surgical treatment of spondylolisthesis among spine surgeons. World Neurosurg. 2018;111:e564-e572.
- Kim BD, Edelstein AI, Hsu WK, et al. Spine surgeon specialty is not a risk factor for 30-day complication rates in single-level lumbar fusion. Spine. 2014;39(15):e919-e927.
- Seicean A, Alan N, Seicean S, et al. Surgeon specialty and outcomes after elective spine surgery. Spine. 2014;39(19):1605-1613.
- Wadhwa RK, Ohya J, Vogel TD, et al. Risk factors for 30-day reoperation and 3-month readmission: analysis from the Quality and Outcomes Database lumbar spine registry. J Neurosurg Spine. 2017;27(2):131-136.
- McCutcheon BA, Ciacci JD, Marcus LP, et al. Thirty-day perioperative outcomes in spinal fusion by specialty within the NSQIP database. Spine. 2015;40(14):1122-1131.
- Singh S, Sparapani R, Wang MC. Variations in 30-day readmissions and length of stay among spine surgeons: a national study of elective spine surgery among US Medicare beneficiaries. J Neurosurg. 2018;29(3):286-291.
- Swann M, Hoes K, Aoun S, McDonagh DL. Postoperative complications of spine surgery. Best Pract Res Clin Anaesthesiol. 2016;30(1):103-120.
- American Chiropractic Association. Back Pain Facts and Statistics. Available at: https://www.acatoday.org/Patients/Health-Wellness-Information/Back-Pain-Facts-and-statistics. Accessed October 29, 2019.
- Hartvigsen J, Hancock MJ, Kongsted A, et al. Low back pain series: what low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356-2367.
- Agarwal N, Gupta R, Agarwal P, et al. Descriptive analysis of state and federal spine surgery malpractice litigation in the United States. Spine. 2018;43(14):984-990.
- Minhas SV, Chow I, Patel AA, Kim JYS. Surgeon specialty differences in single-level anterior cervical discectomy and fusion. Spine. 2014;39(20):1648-1655.
- Lad SP, Babu R, Ugiliweneza B, et al. Surgery for spinal stenosis: long-term reoperation rates, health care cost, and impact of instrumentation. Spine. 2014;39(12):978-987.
Author affiliations: Rami Musleh, MSPA, PA-C, Valparaiso University PA Program. Angela Blagojevski, MPAS, PA-C, Valparaiso University PA Program. Randy Brush, MS, PA-C, Valparaiso University PA Program. Jessica Bruskoski, MS, PA-C, Valparaiso University PA Program. The authors have no relevant financial relationships with any commercial interests.
Read Similar Articles
- Management Of Acute Exacerbation Of Chronic Low Back Pain In The Urgent Care Setting
- An Urgent Care Approach To Low Back Pain
- High-Risk Conditions Presenting As Back Pain
