Urgent message: Spinal epidural abscesses are a rare condition that can be fatal if untreated. Populations most at risk include the elderly, diabetics, and IV drug users. The most common cause of an epidural abscess is the bacteria Staphylococcus aureus.
Savannah Chavez, MD; Jordan Miller, DO; J. Chika Morah, MD
INTRODUCTION
Incidence of spinal epidural abscesses ranges from 0.2 to 2.8 cases per 10,000 per year, with a peak incidence occurring in patients between 60 to 70 years of age. The abscess is most commonly due to Staphylococcus aureus (63%), but may occur from Actinomycosis, gram-negative bacilli, and fungi and can cause spinal epidural abscesses (10%).1,2
Risk factors for spinal epidural abscesses include:
- Spinal trauma
- Spinal procedures or surgery
- IV drug use
- Diabetes mellitus
- Chronic renal failure
- Alcoholism
- AIDS
- Malignancy
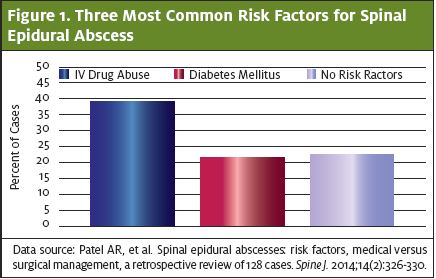
Diabetes mellitus is the most common risk factor for spinal epidural abscesses (23% to 33% of patients have a history of diabetes); however, IV drug use and spinal manipulation (such as placement of an epidural catheter) have become important risk factors in recent years.3-5 (See Figure 1.)
Patients classically present with the triad of back pain, fever, and neurologic deficits due to the compressive nature of the spinal abscess; however, only about 8% of patients will present as such. If spinal epidural abscess is a consideration, prompt diagnosis will minimize morbidity and mortality, although preoperative status predicts mortality rates.6,7
CASE REPORT
History
A 37-year-old female presented to the urgent care clinic with complaints of generalized weakness and the inability to move her legs. She described having to crawl around for parts of the day, saying she felt too weak to move. She said she had basic labs performed at another facility 3 days prior, and that those labs were unremarkable. She continued to grow weaker over the next 24 hours, now presenting to an urgent care for another evaluation. She denied any chest pain, shortness of breath, nausea, vomiting, diarrhea, or skin changes. She admitted to a past history of IV drug use and hepatitis C.
Exam
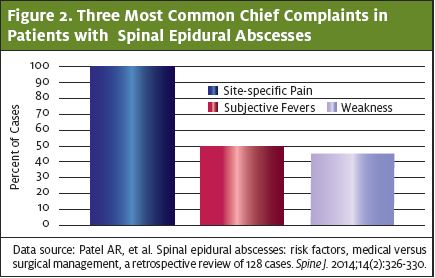
Physical exam revealed a disheveled female who appeared older than her stated age. Her vital signs were remarkable for a heart rate of 100 beats per minute. She otherwise was afebrile, had a normal blood pressure of 115/60, a respiratory rate of 16 breaths per minute, and an oxygen saturation of 100% on room air. Her cardiopulmonary exam was unremarkable. The patient had scabs in different stages of healing over her body, with evidence of track marks in the antecubital fossa of her bilateral arms. She had diminished strength, reflexes, and sensation in all four extremities and denied being able to feel pinpoint sensation. No rashes were seen throughout the integumentary examination and she had normal intact rectal tone. (The most common presenting complaints for patients diagnosed with spinal epidural abscesses are detailed in Figure 2.)
Differential Diagnosis
The differential diagnosis for weakness in an IV drug user includes, but is not limited to:
- Infective endocarditis
- Septic pulmonary emboli
- Spinal epidural abscess
- Drug overdose
- Underlying infection (eg, pneumonia, urinary tract infection, bacteremia)
- Meningitis
- Rhabdomyolysis
Testing/Outcome After the physical exam, the urgent care physician realized that the patient had symptoms consistent with a potentially catastrophic neurological process. The patient was transferred to an emergency department, where laboratory workup revealed a normal white blood cell count of 9.8 (normal 4-11), a hemoglobin of 10.8 (normal 12-16 for women) and a platelet count of 390 (normal 150-450). ESR was elevated at 89 mm/hour (normal 0-20 for women) and CRP was elevated at 62 mm/hour (normal 0-10). Metabolic profile was normal. Urinalysis showed no evidence of infection. Bedside echocardiogram showed no evidence of vegetative lesions on the valves and showed a normal ejection function. The patient had a normal postvoid residual urine volume. CT angiogram of the chest showed no evidence of pulmonary abscesses, pulmonary embolism, or pneumonia. MRI of the spinal cord showed discitis osteomyelitis with a large epidural abscess at C5-6 compressing the spinal cord and epidural phlegmon extending from C3-7 with prevertebral phlegmon extending from C2-T1. The patient was given broad-spectrum antibiotics including vancomycin and cefepime, and was transferred to a tertiary medical center for neurosurgical evaluation.
DISCUSSION
Pathophysiology
Most spinal epidural abscesses are located at the posterior aspect of the thoracic or lumbar spine. Posterior abscesses are thought to originate from a distant focus, such as the skin, or from dental abscesses. Anterior abscesses are predominantly due to discitis or vertebral osteomyelitis and can be caused by direct extension from retropharyngeal or retroperitoneal abscesses.8
Vertebral hematomas due to trauma are seen in up to 35% of cases,9 and a nidus of blood serves as a nutrient source for bacteria to breed. The pathophysiology of spinal epidural abscesses stems from the ability of bacteria to enter the epidural space and seed the areas between the vertebral wall and dura mater, with a suppurative infection forming in the confined area. Bacteria have a few ways to enter this space, the most common being via hematogenous spread. Manipulation of the spinal column with epidural catheter placement, spinal surgeries, and via lumbar puncture are ways for bacteria to enter the central nervous system and spinal column via a direct inoculation.
Diagnosis
Diagnosis of a spinal epidural abscess via physical exam is difficult, as most patients don’t present classically. Pain, which may be found on palpation of the spinous processes near or overlying the spinal epidural abscess, is one of the most common presenting symptoms. Another physical exam finding is pain with straight leg raise, which will cause compression of spinal nerve roots. Neurologic deficits can develop as the disease process progresses, with symptoms consistent with cauda equina such as urinary retention, bowel incontinence, and perianal/saddle anesthesia. Patients may also complain of weakness with walking, paralysis, and numbness.7 Fever is present in 35% to 60% of patients; however, absence of fever cannot rule out spinal epidural abscess.10
Laboratory evaluation includes complete blood count, blood cultures, coagulation studies, and inflammatory markers. Often, erythrocyte sedimentation rate (ESR) is elevated; however, if it is not elevated, one cannot rule out the diagnosis of spinal epidural abscess. ESR sensitivity ranges from 68% to 100%, though only an ESR above 50 mm/hour was considered positive in one case series. In a meta-analysis of 915 patients with spinal epidural abscesses, the sensitivity of an ESR was noted to be 94%. C-reactive protein has a similar sensitivity to ESR at 84% to 100%; however, it is a more effective marker of early disease because it rises faster than an ESR and is influenced less by other plasma factors. Leukocytosis presence is extremely variable and doesn’t predict severity of the disease. A leukocyte count is a nonspecific lab marker and should not be used to exclude the diagnosis of spinal epidural abscess. Magnetic resonance imaging is the test of choice for imaging. If unavailable, CT with IV contrast is another option, although it is less sensitive.10
The bottom line is, if spinal epidural abscess is suspected, do not order outpatient labs as the patient needs emergent imaging with an MRI.
Prompt diagnosis and management are important for patients with an underlying abscess, as delay in diagnosis can result in irreversible neurological damage. Around 4%–22% of patients diagnosed with spinal epidural abscess will have irreversible paraplegia. Around 5% of patients will die from sepsis. A prospective evaluation of clinical decision guidelines to diagnose spinal epidural abscesses in patients showed that 75% of patients diagnosed with spinal epidural abscess suffered delays in diagnosis. A permanent neurological deficit was nearly six times more likely in those who suffered a delay.11
Management
Management includes neurosurgical evaluation, which often requires emergency evacuation to decompress the spinal cord and nerve roots. Endoscopy-assisted surgery and percutaneous drainage have been reported to be successful in some cases. Patients who are deemed surgical candidates will need to undergo aspiration, surgical drainage, and antibiotic therapy for 4–6 weeks postsurgery. Repeat MRI should be obtained at 4–6 weeks of therapy or if there is evidence of worsening symptoms or deteriorating clinical examination. Nonsurgical candidates include those with minimal neurologic deficits or those who are generally poor surgical candidates.
Teaching Points
- Spinal epidural abscess is a difficult diagnosis and should be considered with neurological complaints or back pain, especially those patients at increased risk, such as diabetics and IV drug users.
- Testing of choice is emergent MRI scan.
- Prompt diagnosis and treatment are important for epidural spinal abscesses in order to avoid permanent neurologic damage.
REFERENCES
1. Mackenzie AR, Laing RB, Smith CC, et al. Spinal epidural abscess: the importance of early diagnosis and treatment. J Neurol Neurosurg Psychiatry. 1998;65(2):209–12.
2. Martin RJ, Yuan HA. Neurosurgical care of spinal epidural, subdural, and intramedullary abscesses and arachnoiditis. Orthop Clin North Am. 1996;27(1):125–136.
3. Fotaki A, Anatoliotaki M, Tritou I, et al. Review and case report demonstrate that spontaneous spinal epidural abscesses are rare but dangerous in childhood. Acta Paediatr. 2019;108(1):28-36.
4.Du JY, Schell AJ, Kim CY, et al. 30-day mortality following surgery for spinal epidural abscess: incidence, risk factors, predictive algorithm, and associated complications. Spine. 2019;44(8):E500-E509
5. Patel AR, Alton TB, Bransford RJ, et al. Spinal epidural abscesses: risk factors, medical versus surgical management, a retrospective review of 128 cases. Spine. 2014;14(2):326-330.
6. Ameer MA, Knorr TL, Mesfin FB. Spinal epidural abscess. [Updated 2020 Mar 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan. Available at: https://www.ncbi.nlm.nih.gov/books/NBK441890/.
7. Darouiche RO, Hamill RJ, Greenberg SB, et al. Bacterial spinal epidural abscess. Review of 43 cases and literature survey. Medicine (Baltimore). 1992;71(6):369-385.
8. Jang YJ, Rhee CK. Retropharyngeal abscess associated with vertebral osteomyelitis and spinal epidural abscess. Otolaryngol Head Neck Surg. 1998;119(6):705–708.
9. Lee WS, Moussaoui SM, Moskowitz MA. Blockade by oral or parenteral RPR 100893 (a non-peptide NK1 receptor antagonist) of neurogenic plasma protein extravasation within guinea-pig dura mater and conjunctiva. Br J Pharmacol. 1994;112(3):920-924.
10. Chenoweth CE, Bassin BS, Mack MR, et al. Vertebral osteomyelitis, discitis, and spinal epidural abscess in adults [internet]. Ann Arbor (MI): Michigan Medicine University of Michigan; 2018 Dec. Available at: https://www.ncbi.nlm.nih.gov/books/NBK547443/.
11. Ghobrial GM, Beygi S, Viereck MJ, et al. Timing in the surgical evacuation of spinal epidural abscesses. Neurosurg Focus. 2014;37(2):E1.
Author affiliations: Savannah Chavez, MD, Adena Regional Medical Center. Jordan Miller, DO, Adena Health System. J. Chika Morah, MD, Cleveland Clinic Akron General, University of Toledo College of Medicine.The authors have no relevant financial relationships with any commercial interests.

